Abstract
Purpose
The purpose of this study was to describe the treatment of giant retinal tears (GRTs) with 25-gauge pars plana vitrectomy (PPV) and medium-term postoperative perfluoro-n-octane (MT-PFO).
Methods
The study was a retrospective interventional case series of consecutive patients with GRTs treated with 25-gauge PPV and postoperative MT-PFO for a period of 2–3 weeks. A second, staged procedure was performed in all patients for PFO removal.
Results
Twenty-three eyes of 22 patients were studied, with a mean follow-up of 33.04 ± 19.74 months. Successful reattachment was achieved in 91.3 % of eyes (21/23) after MT-PFO. Retinal re-detachment occurred in five eyes, which was caused by proliferative vitreoretinopathy. Additional complications included cataract progression (n = 10), foreign body response (30.4 %, 7/23), and transient intraocular pressure (IOP) elevation (8/23, 34.8 %). Transient IOP elevation was associated with worse visual outcome (p = 0.01).
Conclusions
MT-PFO was found to be an effective and safe technique for operative management of GRTs. In the majority of patients, retinas remained attached without further surgical intervention. Cataract progression, intraocular inflammation, and associated increased intraocular pressure are potential complications of MT-PFO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Giant retinal tears (GRTs) are full-thickness circumferential retinal breaks extending 90° or greater (≥ 3 clock-hours) associated with posterior vitreous detachment. The management of GRTs remains controversial, with several surgical methods currently employed. Regardless of the approach, GRTs pose specific surgical challenges due to their irregular and complex anatomy, high rates of proliferative vitreoretinopathy (PVR), and an increased incidence of retinal slippage and re-detachment [1–3]. To overcome these challenges, the use of heavy liquids such as perfluoro-n-octane (PFO) have gained popularity in recent years, most frequently as an adjunct intraoperative tool for unfolding and tamponade of retinal tissue. The increased density of PFO makes it particularly useful for intraoperative retinal flattening, management of retinal folds and inverted retinal flaps, and prevention of retinal slippage. Several recent reports have indicated that PFO may be safely left in the vitreous cavity for short durations, and is thus useful for short- and intermediate-term retinal tamponade in the setting of retinal detachment and PVR [4–9].
This series focuses on a subset of GRT cases in which we describe the use of “medium-term” postoperative PFO (MT-PFO), as opposed to more standard approaches such as silicone oil or C3F8 gas tamponade and encircling scleral buckle elements. Traditionally, we have used longer-term agents such as silicone oil or C3F8 for GRT cases, with or without scleral buckling procedures, due to the higher risk of PVR formation. The impetus for studying medium-term tamponade with perfluorocarbons arose from our experience with inferior retinal detachment, with and without PVR [4, 5]. In our prior published report of 157 eyes, the overall reattachment rate for rhegmatogenous inferior retinal detachment was 87.5 %, which parallels previously described reattachment procedure success rates. Our follow-up study involving cases of inferior detachment with grade C PVR or worse showed a reattachment rate of 86 %, or 38/44 eyes, in these more complex cases, with rates statistically equivalent between eyes with and without previous scleral buckle.
Given the anatomic complexity and propensity for PVR formation in GRT cases, we postulated that medium-term tamponade with PFO may yield long-term results similar to those of our previous series with inferior detachment, allowing an alternative approach for repair in cases where strict postoperative positioning or scleral buckle may not be feasible. With this technique, we have experienced less intraoperative posterior slippage than previously with the use of silicone oil or gas. We often noticed increased slippage during PFO exchange with gas or oil, which can lead to worse anatomic outcomes such as macular fold formation. By unfolding and flattening the retina in a single step, without gas or oil exchange, we have been able to avoid posterior slippage and reduce operating times. The duration of perfluorocarbon tamponade was again based on our past experience with detachment using MT-PFO. In our initial series, we examined postoperative patients weekly until laser scars were mature, and secondarily removed PFO only after that time. In summary, the purpose of the present study was to describe our experience involving 25-gauge PPV and intermediate (2–3-week duration) MT-PFO followed by staged PFO removal in patients presenting with GRTs.
Methods
Inclusion criteria
This retrospective interventional case series evaluated consecutive patients presenting with large-circumferential retinal tears measuring ≥ 90°, or ≥ 3 contiguous clock hours. All operations were performed by a single surgeon (author S.C.), and patients were recruited from a single vitreoretinal referral center (Charles Retina Institute, Memphis, TN, USA). The study period, including follow-up, encompassed the period from March 2008 to April 2012. Consecutive patients were considered only after meeting the following inclusion criteria:
-
1.
Age 18–75 years
-
2.
Medically stable for surgical intervention
-
3.
Large retinal break with circumferential measurement of ≥ 90°, or ≥3 clock-hours, in any quadrant of the retina
-
4.
No previous ocular conditions other than refractive error, glaucoma, or prior cataract surgery with intraocular lens implantation
-
5.
Willing to provide informed consent for study participation
Patients with documented prior retinal detachment repair, previous retinal breaks requiring treatment, or complete funnel retinal detachment were initially excluded. At the conclusion of the study period, patients with less than 6 months of postoperative follow-up were also excluded.
Surgical technique
The informed consent process was reviewed with all patients, detailing the staged two-procedure approach as well as potential benefits and possible risks (known and unknown). The surgical technique was developed by the senior author, Steve Charles, and consisted of 25-gauge PPV with medium-term PFO for the repair of retinal detachment, including GRTs [4, 5, 10–13]. The first procedure utilized 25-gauge PPV using a sutureless transconjunctival approach and contact-based wide-angle visualization. Any PVR membranes present during the primary surgery were removed with 25-gauge internal limiting membrane forceps before infusion of PFO (Perfluoron; Alcon Laboratories, Inc., Fort Worth TX, USA). PFO was slowly infused overlying the optic nerve head using a viscous fluid controller connected to a 25-gauge dual-bore cannula (MedOne Surgical, Inc., Sarasota, FL, USA), and the cannula tip was positioned at the apex of the single PFO bubble and moved anteriorly to remain in the apex as the bubble increased in size during injection. Infusion of PFO was continued until the retina was adequately unfolded and reattached, and a complete fill of the vitreous cavity was achieved. Subretinal fluid was allowed to egress through the giant tear during unfolding and reattachment. If residual subretinal fluid did not adequately exit through the primary GRT, a small peripheral retinotomy was created to allow complete drainage of fluid during PFO infusion. Following reattachment, all GRTs were surrounded by confluent laser retinopexy using a straight- or flex-tipped 25-gauge endophotocoagulation probe. No cryotherapy was performed. Postoperatively, patients were instructed to maintain head positioning in accordance with the location of the GRT.
Follow-up examinations were initially performed at day 1 postoperatively and again at approximately 2–3 weeks (mean, 18.78 ± 5.17; range, 7–31 days), based on patient convenience. At this time, a staged second procedure was performed only after adequate pigmentation of the laser sites was noted on indirect ophthalmoscopic examination in the clinic setting. PFO was removed from the vitreous cavity using a silicone soft-tip extrusion cannula. Repeat fluid/air exchange was performed in order to ensure that all PFO droplets were removed from the vitreous cavity. Any anterior-chamber PFO that was present was removed using a 30-gauge needle on extrusion inserted through the limbus. Difluprednate 0.05 % ophthalmic emulsion (Durezol; Alcon Laboratories, Inc., Fort Worth, TX, USA) was prescribed four times daily for 2 weeks to manage postoperative inflammation.
Serial measurement of best-corrected Snellen visual acuity (BCVA), intraocular pressure (IOP), and dilated retinal examination were performed at all pre- and postoperative visits. Patients with visible PFO in the anterior chamber or transient IOP elevation were further examined using gonioscopy. Removal of retained anterior chamber PFO was performed in the office setting using a 30-gauge needle inserted through the inferior limbus. If, on follow-up, any area of the retina was found to have inadequate laser photocoagulation, it was augmented using laser indirect ophthalmoscopy in the clinic setting.
Data analysis
The primary outcome measures were anatomic reattachment and BCVA at final postoperative visit. Any postoperative complication was recorded and analyzed as a secondary outcome. The Retina Society classification system [14] was used to classify patients with PVR. The Standardization of Uveitis Nomenclature (SUN) system was employed to categorize any inflammation present [15]. Data including demographics, preoperative BCVA, BCVA at final follow-up, macula status, reoperation rate, PVR grade, and IOP were recorded. All BCVA was converted to logarithm of minimum angle of resolution (logMAR) for statistical analysis. A transient IOP elevation was defined as IOP greater than 21 mmHg despite maximum medical therapy and when the IOP persisted for at least two weeks after secondary PPV. Data analysis was performed using JMP 10 (SAS Institute Inc., Cary, NC, USA). One-way analysis of variance (ANOVA) and Student’s t tests were used to compare continuous variables among categorical variables. Bivariate analysis using the fit line function was employed to compare two continuous variables. Matched-pairs analysis was utilized to compare means between continuous variables, and Fisher’s exact test was used to analyze categorical variables. Statistical significance was considered present for p values < 0.05.
Results
Twenty-three eyes in 22 patients presented with a GRT. The study sample comprised 19 male and 3 female patients, of whom 16 were Caucasian and 6 were African-american. The right eye was involved in 16 cases and the left eye in 7 cases. The mean age was 50.47 ± 11.12 years. Eighteen eyes had no evidence of PVR on presentation, two eyes had grade A PVR, and three eyes had grade B PVR. Sixty-one percent (14/23) of eyes presented with macula involving retinal detachment. The mean initial BCVA was 1.01 ± 0.75 logMAR units, and the mean final BCVA was 1.08 ± 0.81 logMAR units. The mean visual change was a deterioration of −0.08 ± 0.79 logMAR units, with 11 (48 %) eyes showing visual improvement, 4 (17 %) with no change, and 8 (35 %) with decreased vision postoperatively. The mean follow-up was 33.04 ± 19.74 months. Anatomic reattachment was achieved in 91.3 % (n = 21) of cases after initial staged surgery. Five eyes in four patients (23.8 %) had re-detachment due to new/recurrent PVR formation after initial successful reattachment.
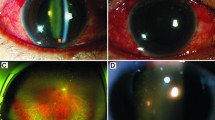
Postoperative complications, encompassing both initial and secondary postoperative periods, included foreign body response, cataract progression, re-detachment, and transient IOP elevation. Of the 14 initially phakic eyes, 10 eyes (71.4 %) eventually required cataract surgery at some point during the follow-up period, and all pre-existing cataracts progressed during the study period. Seven eyes (30.4 %) experienced mild to moderate inflammation. In addition, these seven eyes had a typical PFO foreign body response, consisting of multiple irregular, small, white precipitates within the indwelling PFO or in the retinal and/or posterior lens/IOL surface. In all cases, removal of PFO and treatment with topical corticosteroids were sufficient to control this foreign body response within 3 weeks. Eight of 23 eyes (34.8 %) had transient IOP elevation, with one patient (4.3 %) requiring filtering surgery due to uncontrolled IOP unresponsive to topical agents.
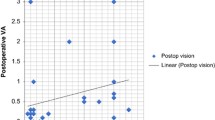
Logistic regression was used to investigate categorical variables related to final BCVA and BCVA change. Visual outcome was not associated with either age (p = 0.11) or gender (p = 0.58). Mean final BCVA was slightly better among macula-on patients (mean, 0.94 ± 0.83 logMAR) than macula-off patients (mean, 1.17 ± 0.81 logMAR), but this difference was not statistically significant (p = 0.53, t test). Macula-off status was significantly associated with change (improvement) in BCVA (p = 0.02). The presence of a foreign body response was not associated with either final BCVA (p = 0.77) or BCVA change (p = 0.40). Transient IOP elevation was significantly associated with worse final BCVA (p = 0.01) and with a decrease in BCVA (p = 0.03). The association of filtering surgery with visual outcome was not possible to evaluate, as the study was underpowered.
Fisher’s exact test was used to investigate the relationship between categorical variables. Neither the foreign body response (p = 0.66, two-tailed) nor the presence of PFO in the anterior chamber during the postoperative period (p = 1.0, two-tailed) were associated with transient IOP elevation.
Discussion
The management of GRTs poses unique surgical challenges, given the high incidence of PVR and the complicated anatomical configurations and variable locations of GRTs within the peripheral retina. Various techniques have been employed for retinal reattachment, including the use of a scleral buckle [16, 17], silicone oil [18–21], intraocular gas [22, 23], and heavier-than-liquid compounds such as PFO [6, 7, 24]. The initial use of PFO in vitreoretinal surgery was as an adjunct intraoperative tool to aid in retinal unfolding and prevention of slippage during placement of long-term tamponade agents such as silicone oil. Recently, the use of longer-duration postoperative PFO has been reported in the literature, with favorable results in cases of retinal detachment both with and without PVR and of GRTs [4–7, 10, 11]. The results of the present study indicate that a high anatomic success rate can be achieved with medium-duration postoperative PFO in the treatment of GRTs. Despite the need for multiple operations and the risk of certain PFO-specific side effects, this technique represents an effective surgical option for an otherwise challenging subset of retinal detachment disorders.
In our series, the success rate for reattachment after staged primary repair with MT-PFO was 91.3 % (23/25). Re-detachment remained the most frequent complication, occurring in five eyes in four patients (23.8 %) over long-term follow-up. The formation of new PVR membranes was responsible for re-detachment in all five eyes.
Excluding the foreseeable complication of re-detachment with any GRT repair, our results also demonstrated three particular complications associated with MT-PFO: cataract progression, foreign body response, and transient IOP elevation. The foreign body response observed in this report is similar in appearance and frequency to our previous clinicopathologic study, where intermediate-duration PFO was used for inferior retinal detachment repair [25]. Twenty-eight percent of cases developed a typical foreign body response characterized by multiple white precipitates within the indwelling PFO, almost identical to that in the present series. We hypothesize that the foreign body response observed in this series is a macrophage-predominant reaction similar to our previous report [25]. Other experimental [26] and clinicopathologic [27] studies have described similar inflammation with the use of PFO.
Our results revealed a 30.4 % incidence of foreign body response, a much higher percentage than those of previous clinical studies using postoperative PFO for retinal detachment [6, 8, 9]. The longer mean duration of PFO in the vitreous cavity and close follow-up in the present study may have contributed to an increased recognition of foreign body response cases. Consistent with our earlier report [5], the presence of foreign body response did not correlate with IOP elevation or anatomic or visual outcomes, and resolved within 3 weeks after PFO removal and topical corticosteroid treatment. We did not observe recurrent inflammation or uveitis of any form over the extended study period. As previously reported [5], the white precipitates characteristic of the foreign body response may hinder the removal of PFO, but to our knowledge, no additional significant complications have been observed.
A more concerning complication of MT-PFO involves the development of transient IOP elevation, with the potential need for filtering surgery. The elevated IOP observed in silicone oil studies [18, 28] led authors to investigate this complication among patients treated with PFO. Several retrospective series [6–8] have found no incidence or a lower rate of IOP elevation than our present results. In contrast, a retrospective series of inferior retinal detachment and GRTs repaired with PPV and short-term (mean, 11 days) PFO duration [9] reported a 35.9 % incidence of IOP > 21 mmHg, a slightly higher percentage than our results. While the authors found no association between patient age or the presence of inflammation and IOP elevation, a significant association was found between IOP and the presence of PFO in the anterior chamber. Similar to our findings, all patients in this series were satisfactorily controlled with topical antiglaucoma drugs. The potential for long-term IOP elevation requiring filtering surgery makes this technique less appealing, especially for uncomplicated cases that may be appropriately managed with vitreous substitutes, silicone oil, or intraocular gas. The 4.3 % rate of patients requiring filtering surgery falls within a range similar to our previous MT-PFO series, which found a need for filtering surgery in 6 % of inferior retinal detachment surgeries [4] and in 5 % of cases of recurrent inferior retinal detachment repair with advanced PVR [5]. These findings require further investigation, including nerve fiber layer analysis in patients who develop transient IOP elevation.
The present study may be limited by a relatively small sample size, the lack of a control group, and the potential bias of a single-center retinal referral practice. In addition, the extensive experience of the surgeon with small-gauge vitrectomy may limit the application of this technique in other clinical settings. In conclusion, MT-PFO appears to be an efficient and safe technique for the management of giant retinal tears, and may avoid the need for silicone oil in some patients. Potential complications such as elevated IOP, cataract progression, and foreign body response warrant consideration.
References
Girard P, Boscher C, Navarro F, Forest A (1984) Retinal detachments caused by giant tear. J Fr Ophtalmol 7(3):205–209
Glaser BM (1986) Treatment of giant retinal tears combined with proliferative vitreoretinopathy. Ophthalmology 93(9):1193–1197
Scott IU, Murray TG, Flynn HW Jr, Feuer WJ, Schiffman JC, Perfluoron Study G (2002) Outcomes and complications associated with giant retinal tear management using perfluoro-n-octane. Ophthalmology 109(10):1828–1833
Sigler EJ, Randolph JC, Calzada JI, Charles S (2013) 25-gauge pars plana vitrectomy with medium-term postoperative perfluoro-n-octane tamponade for inferior retinal detachment. Ophthalmic Surg Lasers Imaging Retina 44(1):34–40. doi:10.3928/23258160-20121221-10
Sigler EJ, Randolph JC, Calzada JI, Charles S (2013) Pars plana vitrectomy with medium-term postoperative perfluoro-N-octane for recurrent inferior retinal detachment complicated by advanced proliferative vitreoretinopathy. Retina 33(4):791–797. doi:10.1097/IAE.0b013e31826a6978
Rofail M, Lee LR (2005) Perfluoro-n-octane as a postoperative vitreoretinal tamponade in the management of giant retinal tears. Retina 25(7):897–901
Sirimaharaj M, Balachandran C, Chan WC, Hunyor AP, Chang AA, Gregory-Roberts J, Hunyor AB, Playfair TJ (2005) Vitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tears. Br J Ophthalmol 89(9):1176–1179. doi:10.1136/bjo.2004.065409
Drury B, Bourke RD (2011) Short-term intraocular tamponade with perfluorocarbon heavy liquid. Br J Ophthalmol 95(5):694–698. doi:10.1136/bjo.2009.175216
Rush R, Sheth S, Surka S, Ho I, Gregory-Roberts J (2012) Postoperative perfluoro-N-octane tamponade for primary retinal detachment repair. Retina 32(6):1114–1120. doi:10.1097/IAE.0b013e31822f56f6
Charles S, Calzada J, Wood B (2011) General posterior segment techniques. In: Pine J (ed) Vitreous microsurgery, 5th edn. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, pp 58–64
Charles S, Calzada J, Wood B (2011) Giant breaks. In: Pine J (ed) Vitreous microsurgery, 5th edn. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, pp 138–143
Charles S (2004) An engineering approach to vitreoretinal surgery. Retina 24(3):435–444
Sigler EJ, Charles S, Calzada JI (2014) Interface vitrectomy. Retina 34(3):616–617. doi:10.1097/IAE.0000000000000091
The Retina Society Terminology Committee (1983) The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology 90(2):121–125
Jabs DA, Nussenblatt RB, Rosenbaum JT (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140(3):509–516
Chen CH, Tsai MH, Su CC, Kou HK, Kao ML, Tsai SH, Chen YJ (2001) Results of 12-year clinical study of giant retinal tear. Chang Gung Med J 24(10):633–639
Goezinne F, La Heij EC, Berendschot TT, Gast ST, Liem AT, Lundqvist IL, Hendrikse F (2008) Low redetachment rate due to encircling scleral buckle in giant retinal tears treated with vitrectomy and silicone oil. Retina 28(3):485–492. doi:10.1097/IAE.0b013e318150d879
Leaver PK, Billington BM (1989) Vitrectomy and fluid/silicone-oil exchange for giant retinal tears: 5 years follow-up. Graefes Arch Clin Exp Ophthalmol 227(4):323–327
Camacho H, Bajaire B, Mejia LF (1992) Silicone oil in the management of giant retinal tears. Ann Ophthalmol 24(2):45–49
Karel I, Michalickova M, Soucek P (1996) Long-term results of pars plana vitrectomy and silicone oil for giant tears. Eur J Ophthalmol 6(3):315–321
Unlu N, Kocaoglan H, Acar MA, Sargin M, Aslan BS, Duman S (2003) The management of giant retinal tears with silicone oil. Eur J Ophthalmol 13(2):192–195
Hoffman ME, Sorr EM (1986) Management of giant retinal tears without scleral buckling. Retina 6(4):197–204
Batman C, Cekic O (1999) Vitrectomy with silicone oil or long-acting gas in eyes with giant retinal tears: long-term follow-up of a randomized clinical trial. Retina 19(3):188–192
Al-Khairi AM, Al-Kahtani E, Kangave D, Abu El-Asrar AM (2008) Prognostic factors associated with outcomes after giant retinal tear management using perfluorocarbon liquids. Eur J Ophthalmol 18(2):270–277
Sigler EJ, Randolph JC, Charles S (2014) Foreign body response within postoperative perfluoro-N-octane for retinal detachment repair: clinical features, grading system, and histopathology. Retina 34(2):237–246. doi:10.1097/IAE.0b013e31829d002e
Chang S, Sparrow JR, Iwamoto T, Gershbein A, Ross R, Ortiz R (1991) Experimental studies of tolerance to intravitreal perfluoro-n-octane liquid. Retina 11(4):367–374
Elsing SH, Fekrat S, Green WR, Chang S, Wajer SD, Haller JA (2001) Clinicopathologic findings in eyes with retained perfluoro-n-octane liquid. Ophthalmology 108(1):45–48
Aylward GW, Cooling RJ, Leaver PK (1993) Trauma-induced retinal detachment associated with giant retinal tears. Retina 13(2):136–141
Ethical standards
This study conformed to the tenets set forth in the Declaration of Helsinki, and was performed in accordance with the Health Insurance Portability and Accountability Act of 1996 (HIPAA). The study was approved by the institutional review board of the University of Tennessee Health Science Center at Memphis, TN. Patients were included only after providing informed consent for study participation.
Conflict of interest
Dr. Charles is a consultant for Alcon Laboratories, Fort Worth, TX.
All other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Randolph, J.C., Diaz, R.I., Sigler, E.J. et al. 25-gauge pars plana vitrectomy with medium-term postoperative perfluoro-n-octane for the repair of giant retinal tears. Graefes Arch Clin Exp Ophthalmol 254, 253–257 (2016). https://doi.org/10.1007/s00417-015-3049-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3049-4