Abstract
Purpose
The objective of his study was to compare the visual and anatomical outcomes in treatment-naïve patients with macular edema secondary to retinal vein occlusion after intravitreal injections of dexamethasone implants (DEX) and anti-VEGF.
Methods
One hundred two patients (64 in the anti-VEGF group, 38 in the DEX group) without previous treatment were included in this multi-center retrospective study and evaluated at baseline and 1, 3, 6, and 12 months after the onset of treatment. Patients were defined as "good responders" if central macular thickness (CMT) was less than or equal to 250 μm in TD-OCT or 300 μm in SD-OCT after the injections.
Results
At month 3 (n = 102), BCVA had increased significantly, by 0.1 ± 0.3 logMAR in the anti-VEGF group (p = 0.04) and 0.4 ± 0.4 logMAR in the DEX group (p < 0.001); the difference between the two groups was statistically significant (p = 0.007). CMT decreased significantly, by 138 ± 201 μm (−19 %, p < 0.001) in the anti-VEGF group and 163 ± 243 μm (−21 %, p < 0.001) in the DEX group. After 3 months, five patients (13 %) in the DEX group and 20 (31 %) in the anti-VEGF group (p < 0.001) changed treatment. Among the 77 patients who did not switch from their initial treatment, no significant functional or anatomical difference between the two groups was observed at months 6 and 12. Elevation of intraocular pressure > 21 mmHg was more frequent in the DEX group (21 %) than in the anti-VEGF group (3 %, p = 0.008).
Conclusions
Visual acuity recovery was better in the DEX group than in the anti-VEGF group at month 3, but with no difference in CMT. In patients who did not change treatment, the long-term anatomical and visual outcome was similar between the DEX and anti-VEGF groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Macular edema (ME) remains the most frequent complication of central [1, 2] and branch retinal vein occlusion [3]. Research has shown that ME leads to visual deterioration, with some studies reporting visual acuity (VA) less than 20/40 after 3 years [1, 4, 5]. Since 2005, there has been extensive research on recombinant monoclonal antibodies against human vascular endothelial growth factor (VEGF), either the full-length recombinant antibody (bevacizumab) or the Fab fragment that specifically binds all isoforms of VEGF-A (ranibizumab) [6–10]. The dexamethasone intravitreal implant (DEX) is a water-soluble synthetic glucocorticoid that delivers dexamethasone with an estimated half-life of 5.5 h. This implant was recently commercialized for the treatment of ME due to retinal vein occlusion [11–13]. Randomized clinical trials comparing anti-VEGF and DEX are under way, and will help clinicians in refining the indications and the limitations of these drugs in clinical practice. Real-life use of these medications has given rise to recommendations for the management of retinal vein occlusion and associated ME [2, 14]. Recent clinical studies have demonstrated the efficacy and safety profile of anti-VEGF intravitreal injections using both ranibizumab (BRAVO [10, 15, 16], CRUISE [15–17], HORIZON [18]) and bevacizumab [19, 20] for up to 24 months as well as for the dexamethasone intravitreal implant [11, 12].
The objective of this multi-center retrospective study was to analyze the 3- and 12-month visual outcome in previously untreated (treatment-naïve) patients with ME secondary to retinal vein occlusion (RVO), who received DEX or anti-VEGF intravitreal injections.
Methods
This was a retrospective multi-center study conducted at the University Hospitals of Dijon and Grenoble, France, between 2008 and 2012. The study adhered to the tenets of the Declaration of Helsinki regarding research involving human subjects and was approved by the local institutional review board (#IRB 00008855).
We collected the charts of treatment-naïve patients presenting with central retinal vein occlusion (CRVO) or branch retinal artery occlusion (BRVO) complicated by ME, with a visual acuity of +0.3 logarithm of minimum angle of resolution (logMAR) or worse and a baseline central macular thickness (CMT) greater than 250 μm using TD-OCT or 295 μm using SD-OCT. Patients presenting with other retinal vascular diseases, particularly diabetic retinopathy and age-related macular degeneration, were excluded from the study. Patients who had already undergone treatment for ME (corticosteroids, anti-VEGF injections, or laser) were also excluded.
The indication for each treatment was left to the discretion of each physician, depending on the systemic and ocular history (glaucoma, retinal ischemia, or neovascularization). Patients with medically uncontrolled glaucoma were not treated with DEX. Anti-VEGF treatment was available in our centers from 2008, DEX treatment from 2011.
All patients received intravitreal injection of either anti-VEGF (bevacizumab 1.25 mg or ranibizumab 0.5 mg) or DEX. All patients treated with anti-VEGF agents received three injections within the first 3 months. Patients treated with DEX received one intravitreal implant for a minimum period of 4 months before a new injection. Grid laser treatment was not used during the study period.
All patients were evaluated at baseline and at months 1, 3, 6, and 12 with best-corrected visual acuity (BCVA), slit-lamp examination, fundus assessment, intraocular pressure (IOP) measurement (Goldmann applanation tonometry), and time-domain (TM-OCT, Stratus®; Carl Zeiss Meditec, Inc., Dublin, CA, USA) or spectral-domain OCT (SD-OCT, Cirrus®; Carl Zeiss Meditec, Inc., Dublin, CA, USA; or HRA+OCT®; Heidelberg Engineering, Heidelberg, Germany). For each patient, the same OCT device was used throughout the follow-up period. Fluorescein angiography (FA) was performed in all patients using the Topcon TRC-50IX retinal camera (Topcon Corp., Tokyo, Japan) or the Spectralis® HRA (Heidelberg Engineering) to evaluate the perfusion of the macula and peripheral retina at baseline. Response to treatment was graded at each visit, and a patient was defined as a "good responder" if CMT was less than or equal to 250 μm in TD-OCT or 300 μm in SD-OCT [21]. Retinal non-perfusion was defined as 10 or more disc areas absent of capillary perfusion [22]. Macular ischemia was graded on a five-point scale, as follows: 0, normal; 1, questionable; 2, less than half the original circumference destroyed; 3, more than half the contour destroyed but some remnants remaining; and 4, capillary outline completely destroyed [23].
Intravitreal drug administration
Topical anesthesia was administered by instilling one tetracaine eye drop (tetracaine faure 1 %, 1 mg/mL; Novartis Pharma S.A.S., Paris, France) in the conjunctival fornix. After skin and conjunctival disinfection (Betadine® 5 % Sterile Ophthalmic Prep; Méda Pharma, Paris, France) and draping, a lid speculum was put in place, and the product was injected 3.5 mm from the limbus, as follows: bevacizumab (Avastin, 1.25 mg; Genentech, Inc., South San Francisco, CA, USA), ranibizumab (Lucentis®, 0.5 mg; Genentech/Novartis Pharma S.A.S.) or the DEX implant (Ozurdex; Allergan, Inc., Irvine, CA, USA). A prophylactic antibiotic treatment (Azyter® 15 mg/g; Spectrum Thea Pharmaceuticals Ltd, Clermont-Ferrand, France) was prescribed twice a day for 3 days, immediately after the injection.
Retreatment
Patients were eligible for retreatment if retinal thickness increased by 50 μm and/or if CMT was greater than 250 μm TD-OCT or 300 μm in SD-OCT and/or if visual improvement was less than three lines on the logMAR scale.
Visual acuity and central macular thickness
A significant change in VA was defined as a gain or loss of three or more lines on the logMAR scale (increase of three lines on the logMAR scale is equal to doubling the visual angle) [24]. Because of different retinal thickness measurement techniques using OCT, all macular thickness measurements were converted to an SD OCT measurement from the Cirrus® device. The conversion of CMT measurements was defined as CMT (using an SD-OCT [Cirrus®]) = CMT (Spectralis®) × 0.6 + 96.2 or CMT [Stratus®] × 0.9 + 93.5 [25].
Statistics
For statistical analysis, the BCVA measurements were converted to the logMAR scale [26]. Descriptive statistics are given as the mean and standard deviation (SD). Nonparametric tests were used for comparisons between the two treatment groups (Mann–Whitney test) and for paired comparisons (Wilcoxon test). We used the chi-square test (Fisher exact test) for dichotomous data and the Spearman test for nonparametric correlations. We used the Statistical Package for the Social Sciences (SPSS, version 17.0; SPSS Inc., Chicago, IL, USA). A value of P < 0.05 was considered statistically significant. All tests were two-tailed.
Results
Baseline characteristics
One hundred two patients with ME secondary to CRVO or BRVO were included in the study; 64 treatment-naïve patients comprised the anti-VEGF group and 38 the DEX group. The main characteristics of the study population are summarized in Table 1. Both groups were comparable at baseline, with the exception that pseudophakia was more frequent in the anti-VEGF group.
After 3 months, 25 patients (5 patients [13 %] in the DEX group and 20 patients [31 %] in the anti-VEGF group, p < 0.001) switched treatment, i.e., changed from anti-VEGF to DEX or vice versa. For this reason, the analysis at months 1 and 3 was based on the overall population (n = 102) before a possible switch. Analysis was also performed at months 6 and 12 on the 77 patients who did not switch their initial treatment (44 patients in the anti-VEGF group and 33 patients in the DEX group).
Visual acuity
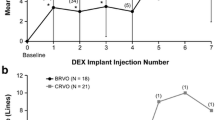
At month 3, for the overall population (n = 102 eyes), the BCVA mean values showed no significant difference (p = 0.5) between the anti-VEGF group (0.6 ± 0.5 logMAR) and the DEX group (0.5 ± 0.4 logMAR) (Fig. 1). BCVA was significantly increased, by 0.1 ± 0.3 logMAR in the anti-VEGF group (p = 0.04) and 0.4 ± 0.4 logMAR in the DEX group (p < 0.001); the difference between the two groups was statistically significant (p = 0.007).
For the population that did not change treatment (n = 77), no significant difference in BCVA mean values was noted between the two groups at months 6 and 12 (p = 0.01 and 0.02, respectively; Fig. 2). In the anti-VEGF group, BCVA was significantly increased from baseline only at month 6, by 0.1 ± 0.4 logMAR (p = 0.02), but there was a non-significant increase at month 12 (increase by 0.1 ± 0.5 logMAR, p = 0.1). In the DEX group, BCVA was significantly increased from baseline at both month 6 (0.3 ± 0.4 logMAR (p = 0.001) and month 12 (0.3 ± 0.5 logMAR (p = 0.005). There was no significant difference between the two groups in terms of increased VA at either the 6-month or 12-month visits.
Central macular thickness
At month 3, mean CMT values in the anti-VEGF Group (430 ± 160 μm) were significantly higher (p = 0.04) than those of the DEX group (368 ± 141 μm) (Fig. 3). CMT had decreased significantly, by 138 ± 201 μm (−19 %, p < 0.001) in the anti-VEGF group and 163 ± 243 μm (−21 %, p < 0.001) in the DEX group. There was no statistically significant difference in CMT changes from baseline between the two groups (p = 0.8).
CMT in both groups at 1-month (M1) and 3-month (M3) visits for the 102 treatment-naïve patients. At M3, there was a statistically significant difference (p = 0.04) in the mean CMT value between the two groups. However, CMT changes from baseline were not significantly different between the two groups (p = 0.8)
At month 6 (Fig. 4), there was no significant difference (p = 0.2) between CMT mean values in the anti-VEGF group (409 ± 158 μm) and the DEX group (378 ± 164 μm). CMT decreased by 138 ± 207 μm (−20 %) in the anti-VEGF group (p = 0.001) and 153 ± 234 μm (−17 %) in the DEX group (p = 0.001). The CMT values from baseline were not statistically different between the two groups (p = 0.2)
At month 12 (Fig. 4), there was no significant difference (p = 0.5) in mean CMT values between the anti-VEGF (342 ± 140 μm) and DEX (386 ± 192 μm) groups. CMT was decreased by 210 ± 211 μm (−32 %) in the anti-VEGF group (p < 0.001) and 137 ± 178 μm (−20 %) in the DEX group (p = 0.005). There was no statistically significant difference in change in CMT values from baseline between the two groups (p = 0.2).
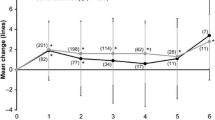
The frequency of “good responders” was significantly lower in the anti-VEGF group (11 %) than in the DEX group (28 %) at M1 (p = 0.04). There was no longer a significant difference between the two groups at M3 (9 % vs 13 %) (Fig. 5a). Within the population that had not changed treatment (n = 77), the “good-responder” rate was similar between the two groups, 11 % at month 6 and 25 % at month 12 in the anti-VEGF group, and 21 % and 26 % in the DEX group at months 6 and 12, respectively (Fig. 5b).
a Good-responder rate at 1-month (M1) and 3-month (M3) visits for the 102 treatment-naïve patients. The number of “good responders” was significantly lower in the anti-VEGF group than in the DEX group at M1 (p = 0.04). There was no significant difference between the two groups at M3. b Good-responder rate at 6-month (M6) and 12-month (M12) visits for the 77 treatment-naïve patients. There was no significant difference between the two groups at M6 or M12.
Intravitreal injection
During the follow-up, patients received 6 ± 1.5 injections in the anti-VEGF group and 1.6 ± 0.6 intravitreal injections (IVIs) in the DEX group. The period between two injections was 1.7 ± 1.2 months and 3.3 ± 3.6 months in the anti-VEGF and DEX groups, respectively.
Adverse events
Ocular hypertension defined as an intraocular pressure (IOP) > 21 mmHg occurred significantly more frequently in the DEX group than in the anti-VEGF group (21 % and 3.1 %, respectively; p = 0.008). No endophthalmitis or ocular inflammation was noted during the follow-up. Three patients (7.9 %) in the DEX group versus seven patients (10.9 %) in the anti-VEGF group had cataract surgery during the follow-up period (p > 0.05).
Discussion
In patients naïve to any therapeutic intervention for ME, this non-randomized interventional study demonstrated that over the short term (3 months), the DEX implant induced greater improvement in VA than three anti-VEGF injections, with similar anatomical (OCT) results and a lower switch rate. For patients who underwent the same treatment for 12 months, the longer-term results (months 6 and 12) were similar between the two treatments with regard to VA, retinal thickness, and good-responder rates as defined by OCT measurements.
This study is unique in that it reports the first-line use of DEX and anti-VEGF therapy in treatment-naïve patients under conditions of daily practice, which differ from those of randomized studies in which the choice of therapy was dependent on the patients' ophthalmological and systemic history. In addition, our results at 6 and 12 months take into account only patients who did not change treatments (for reasons of efficacy, compliance, or side effects), and therefore reflect the efficacy of a medication in optimal conditions of use. Results analyzed in a “real-life environment” could thus differ significantly from the “intention to treat” analysis normally used in randomized trials. Our results may overestimate the efficacy of one or both treatments. Among studies including patients who were naïve to any treatment, only three have investigated patients with BRVO [20, 27, 28] and five have studied patients with CRVO [27–31]. The absence of prior treatment suggests that the time to treatment is often shorter and there is less inclusion bias (patients presenting significant recurrence or resistance to treatment). On the other hand, prior treatment is susceptible to introducing greater response variability.
Two therapeutic families, DEX and anti-VEGFs, are currently authorized for use in treating RVO. Macular edema in retinal vein occlusion results in the rupture of the hematoretinal barrier via two associated processes: one hemorheologic, with an increase in venous pressure, and one metabolic, with secretion of angiogenic factors (VEGF) and pro-inflammatory substances [32]. Dexamethasone has an anti-inflammatory action, including reduction in vascular permeability, inhibition of inflammatory cell migration, stabilization of the tight junctions of endothelial cells, and inhibition of VEGF synthesis, cytokines (IL-6, IL-8, MCP-1), and prostaglandins [33, 34]. Ranibizumab inhibits endothelial cell proliferation and reduces vascular permeability by blocking the liaison between VEGF-A and its receptor [35]. There are currently at least five ongoing prospective randomized studies comparing the efficacy of DEX and ranibizumab (see clinical trials NCT01427751, NCT01231633, NCT01580020, NCT01827722, and NCT01427751). One published study (31 treatment-naïve eyes with CRVO) compared the efficacy of intravitreal injections of triamcinolone and bevacizumab [19], demonstrating no significant differences between the two groups in terms of VA or CMT at 3, 6, and 9 months. Given the paucity of comparative data between DEX and anti-VEGF [36, 37], we analyzed the results obtained with these two treatments over the short (3-month) and intermediate (12-month) terms. Before treatment, the two groups of patients in our series were similar with regard to the main prognostic factors, including VA, age, retinal ischemia, type of RVO, time from diagnosis to treatment, and baseline CMT [22, 38, 39]. Macular ischemia is associated with poor visual outcome [6], and most often does not deteriorate after anti-VEGF treatment [40].
The functional improvement observed after 3 months of anti-VEGF treatment in the present study was less than that described in the CRUISE [17] and BRAVO [10] studies, in which a gain in visual acuity ≥ 15 letters (0.3 logMAR) was reported in 36–50 % of cases 3 months after injection of ranibizumab, with a mean gain in visual acuity of 16 letters for BRVO and 12.7 letters for CRVO. Similarly, in a randomized study of eyes with BRVO, Moradian et al. reported a mean increase of 0.4 ± 0.3 logMAR at month 3 after two intravitreal injections of bevacizumab, similar to what was found in the sham group [20]. Over the longer term (12 months), our series describes a population for which the poor responders and patients presenting side effects were excluded, which induced a bias. However, the less favorable results obtained at month 3 in comparison to BRAVO and CRUISE were confirmed at month 12 (mean increase of 0.1 ± 0.5 logMAR in the present series compared to a mean VA improvement of 0.3 logMAR for BRAVO and CRUISE). The less favorable results in our series are likely related to the less stringent injection protocol (based on patient needs and not systematically every month) and to the selection of treated populations (BRVO/CRVO ratio, naïve eyes, preferential indications for one of the two products) in our study. There are no available data in the literature for comparing the effects of bevacizumab and ranibizumab in vein occlusions, but there is little difference among published studies with regard to the efficacy of the two drugs in patients with age-related macular degeneration [41–44].
The mean gain in visual acuity achieved in our study 3 months after injection of DEX is comparable to that reported in the GENEVA study [11] (gain ≥ 0.3 logMAR in 22 % of eyes and a mean gain of 7 letters at month 3, 8 letters for BRVO and 4 letters for CRVO). In a recent retrospective study [29], intravitreal injections of DEX produced a gain of ≥ 0.3 logMAR in VA at month 3, estimated at 30 % of cases for BRVO and 38 % of cases for CRVO. In the latter study, over 12 months, the number of DEX injections was three or more for 23 % of the patients.
With regard to changes in CMT, at month 3, the data reported in the literature show a 16 to 59 % decrease in retinal thickness with anti-VEGF treatment. Over the longer term, at 6 and 12 months, the reduction in retinal thickness ranges from 31 to 53 %. The GENEVA study reported a significant decrease in CMT after DEX injections, ranging from 27 % in patients with BRVO to 41 % in those with CRVO. In our study, the results for mean change in CMT, like those for visual acuity, are in the lower range of results published in the literature. Considering the CMT results according to the “good-responder” classification, DEX and anti-VEGF are equivalent at month 3 (9 and 13 %, respectively) and M12 (25 % and 26 %, respectively).
The recurrence rate (defined as a decrease in macular thickness followed by an increase > 30 %) and the rebound effect rate (defined as recurrence with CMT > 110 % compared to baseline) [45] were similar between patients receiving bevacizumab injections (52 % and 11 %, respectively) [45] and DEX (56 % and 13 %, respectively) [46]. The rebound effect appeared to be associated with excessively early treatment and/or lower retinal thickness (i.e., which is not at the maximum during treatment) [45]. The mean time to recurrence was 8–12 weeks for patients treated with bevacizumab [45] and 18 weeks for patients treated with DEX [46]. The incidence of medication switches in our study was higher with anti-VEGF (31 %, versus 13 % for DEX), with the decision to change treatment based on an insufficient therapeutic response or the occurrence of side effects. It is possible that introducing anti-VEGF treatment earlier (2008–2011) than DEX treatment (2011–2012) in our daily practice was a bias for switching medication.
During our study, 8 % of the patients in the DEX group and 11 % of the patients in the anti-VEGF group underwent cataract surgery, which is consistent with the GENEVA study [12]. Intraocular hypertension (IOP > 21 mmHg) was more frequent after injection of DEX (21 % in our study, from 9 % to 27 % in the literature) [47] compared to anti-VEGF (absence of hypertension in our study, from 5.5 % to 6 % in the literature) [47]. A history of ocular hypertension and/or glaucoma very clearly conditioned the choice of anti-VEGF treatment, in accordance with the guidelines.
The limitations of this study were primarily its retrospective design, the absence of ultrastructural data in OCT, and the combined analysis of patients presenting CRVO or BRVO, with different anatomic and functional response to treatment [12, 18, 28, 48]. Both treatment groups were imbalanced at baseline with regard to frequency of pseudophakia. Despite this difference before treatment, the number of cataract surgeries was not higher in the DEX group, as would have been expected. These results should be interpreted with caution, as lens opacity was not classified according to standardized measures and a double-blind method.
In conclusion, in previously untreated patients, DEX appeared to be more effective than anti-VEGF treatment in terms of improvement in visual acuity and reduction in macular thickness (higher good-responder rate) at 1 month. At 3 months, the visual gain was better with DEX compared to anti-VEGF injections, whereas the decrease in macular thickness was similar. At both 6 months and 1 year, the anatomic efficacy of the two treatments was comparable for patients who had not switched medications.
References
McIntosh RL, Rogers SL, Lim L, Cheung N, Wang JJ, Mitchell P, Kowalski JW, Nguyen HP, Wong TY (2010) Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology 117:1113–1123
Coscas G, Loewenstein A, Augustin A, Bandello F, Battaglia Parodi M, Lanzetta P, Mones J, de Smet M, Soubrane G, Staurenghi G (2011) Management of retinal vein occlusion–consensus document. Ophthalmologica 226:4–28
Rogers SL, McIntosh RL, Lim L, Mitchell P, Cheung N, Kowalski JW, Nguyen HP, Wang JJ, Wong TY (2010) Natural history of branch retinal vein occlusion: an evidence-based systematic review. Ophthalmology 117:1094–1101. doi:10.1016/j.ophtha.2010.01.058
The Branch Vein Occlusion Study Group (1984) Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 98:271–282
Hansen LL, Danisevskis P, Arntz HR, Hovener G, Wiederholt M (1985) A randomised prospective study on treatment of central retinal vein occlusion by isovolaemic haemodilution and photocoagulation. Br J Ophthalmol 69:108–116
Campochiaro PA, Hafiz G, Channa R, Shah SM, Nguyen QD, Ying H, Do DV, Zimmer-Galler I, Solomon SD, Sung JU, Syed B (2010) Antagonism of vascular endothelial growth factor for macular edema caused by retinal vein occlusions: two-year outcomes. Ophthalmology 117:2387–2394. doi:10.1016/j.ophtha.2010.03.060
Ferrara DC, Koizumi H, Spaide RF (2007) Early bevacizumab treatment of central retinal vein occlusion. Am J Ophthalmol 144:864–871
Kreutzer TC, Alge CS, Wolf AH, Kook D, Burger J, Strauss R, Kunze C, Haritoglou C, Kampik A, Priglinger S (2008) Intravitreal bevacizumab for the treatment of macular oedema secondary to branch retinal vein occlusion. Br J Ophthalmol 92:351–355
Stahl A, Agostini H, Hansen LL, Feltgen N (2007) Bevacizumab in retinal vein occlusion-results of a prospective case series. Graefes Arch Clin Exp Ophthalmol 245:1429–1436
Campochiaro PA, Heier JS, Feiner L, Gray S, Saroj N, Rundle AC, Murahashi WY, Rubio RG (2010) Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology 117:1102–1112
Haller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jacques ML, Jiao J, Li XY, Whitcup SM (2010) Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology 117:1134–1146
Haller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jiao J, Li XY, Whitcup SM, Li J (2011) Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology 118:2453–2460
Moisseiev E, Goldstein M, Waisbourd M, Barak A, Loewenstein A (2013) Long-term evaluation of patients treated with dexamethasone intravitreal implant for macular edema due to retinal vein occlusion. Eye (Lond) 27:65–71
Channa R, Smith M, Campochiaro PA (2011) Treatment of macular edema due to retinal vein occlusions. Clin Ophthalmol 5:705–713
Campochiaro PA, Brown DM, Awh CC, Lee SY, Gray S, Saroj N, Murahashi WY, Rubio RG (2011) Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: twelve-month outcomes of a phase III study. Ophthalmology 118:2041–2049
Brown DM, Campochiaro PA, Bhisitkul RB, Ho AC, Gray S, Saroj N, Adamis AP, Rubio RG, Murahashi WY (2011) Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology 118:1594–1602
Brown DM, Campochiaro PA, Singh RP, Li Z, Gray S, Saroj N, Rundle AC, Rubio RG, Murahashi WY (2010) Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology 117:1124–1133
Heier JS, Campochiaro PA, Yau L, Li Z, Saroj N, Rubio RG, Lai P (2012) Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology 119:802–809
Ding X, Li J, Hu X, Yu S, Pan J, Tang S (2011) Prospective study of intravitreal triamcinolone acetonide versus bevacizumab for macular edema secondary to central retinal vein occlusion. Retina 31:838–845
Moradian S, Faghihi H, Sadeghi B, Piri N, Ahmadieh H, Soheilian M, Dehghan MH, Azarmina M, Esfahani MR (2011) Intravitreal bevacizumab vs. sham treatment in acute branch retinal vein occlusion with macular edema: results at 3 months (Report 1). Graefes Arch Clin Exp Ophthalmol 249:193–200
Bhisitkul RB, Campochiaro PA, Shapiro H, Rubio RG (2013) Predictive value in retinal vein occlusions of early versus late or incomplete ranibizumab response defined by optical coherence tomography. Ophthalmology 120:1057–1063
The Central Vein Occlusion Study (1993) Baseline and early natural history report. Arch Ophthalmol 111:1087–1095
Conrath J, Giorgi R, Raccah D, Ridings B (2005) Foveal avascular zone in diabetic retinopathy: quantitative vs qualitative assessment. Eye (Lond) 19:322–326
Ferris FL 3rd, Kassoff A, Bresnick GH, Bailey I (1982) New visual acuity charts for clinical research. Am J Ophthalmol 94:91–96
Giani A, Cigada M, Choudhry N, Deiro AP, Oldani M, Pellegrini M, Invernizzi A, Duca P, Miller JW, Staurenghi G (2010) Reproducibility of retinal thickness measurements on normal and pathologic eyes by different optical coherence tomography instruments. Am J Ophthalmol 150:815–824
Holladay JT (1997) Proper method for calculating average visual acuity. J Refract Surg 13:388–391
Figueroa MS, Contreras I, Noval S, Arruabarrena C (2010) Results of bevacizumab as the primary treatment for retinal vein occlusions. Br J Ophthalmol 94:1052–1056
Pai SA, Shetty R, Vijayan PB, Venkatasubramaniam G, Yadav NK, Shetty BK, Babu RB, Narayana KM (2007) Clinical, anatomic, and electrophysiologic evaluation following intravitreal bevacizumab for macular edema in retinal vein occlusion. Am J Ophthalmol 143:601–606
Joshi L, Yaganti S, Gemenetzi M, Lightman S, Lindfield D, Liolios V, Menezo V, Shao E, Taylor SR (2013) Dexamethasone implants in retinal vein occlusion: 12-month clinical effectiveness using repeat injections as-needed. Br J Ophthalmol 97:1040–1044
Kriechbaum K, Michels S, Prager F, Georgopoulos M, Funk M, Geitzenauer W, Schmidt-Erfurth U (2008) Intravitreal Avastin for macular oedema secondary to retinal vein occlusion: a prospective study. Br J Ophthalmol 92:518–522
Risard SM, Pieramici DJ, Rabena MD, Basefsky JC, Avery RL, Castellarin AA, Nasir MA, See RF, Couvillion SS (2011) Intravitreal ranibizumab for macular edema secondary to central retinal vein occlusion. Retina 31:1060–1067
Yoshimura T, Sonoda KH, Sugahara M, Mochizuki Y, Enaida H, Oshima Y, Ueno A, Hata Y, Yoshida H, Ishibashi T (2009) Comprehensive analysis of inflammatory immune mediators in vitreoretinal diseases. PLoS One 4:e8158
Felinski EA, Antonetti DA (2005) Glucocorticoid regulation of endothelial cell tight junction gene expression: novel treatments for diabetic retinopathy. Curr Eye Res 30:949–957
Nauck M, Karakiulakis G, Perruchoud AP, Papakonstantinou E, Roth M (1998) Corticosteroids inhibit the expression of the vascular endothelial growth factor gene in human vascular smooth muscle cells. Eur J Pharmacol 341:309–315
Ferrara N, Damico L, Shams N, Lowman H, Kim R (2006) Development of ranibizumab, an anti-vascular endothelial growth factor antigen binding fragment, as therapy for neovascular age-related macular degeneration. Retina 26:859–870
Gado AS, Macky TA (2014) Dexamethasone intravitreous implant versus bevacizumab for central retinal vein occlusion-related macular oedema: a prospective randomized comparison. Clin Exp Ophthalmol 42:650–655
Guignier B, Subilia-Guignier A, Fournier I, Ballonzoli L, Speeg-Schatz C, Gaucher D (2013) Prospective pilot study: efficacy of intravitreal dexamethasone and bevacizumab injections in the treatment of macular oedema associated with branch retinal vein occlusion. Ophthalmologica 230:43–49
Glacet-Bernard A, Coscas G, Chabanel A, Zourdani A, Lelong F, Samama MM (1996) Prognostic factors for retinal vein occlusion: prospective study of 175 cases. Ophthalmology 103:551–560
Klein R, Moss SE, Meuer SM, Klein BE (2008) The 15-year cumulative incidence of retinal vein occlusion: the Beaver Dam Eye Study. Arch Ophthalmol 126:513–518
Manousaridis K, Talks J (2012) Macular ischaemia: a contraindication for anti-VEGF treatment in retinal vascular disease? Br J Ophthalmol 96:179–184. doi:10.1136/bjophthalmol-2011-301087
Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Wordsworth S, Reeves BC (2012) Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology 119:1399–1411
Kodjikian L, Souied EH, Mimoun G, Mauget-Faysse M, Behar-Cohen F, Decullier E, Huot L, Aulagner G (2013) Ranibizumab versus bevacizumab for neovascular age-related macular degeneration: results from the GEFAL noninferiority randomized trial. Ophthalmology 120:2300–2309
Krebs I, Schmetterer L, Boltz A, Told R, Vecsei-Marlovits V, Egger S, Schonherr U, Haas A, Ansari-Shahrezaei S, Binder S (2013) A randomised double-masked trial comparing the visual outcome after treatment with ranibizumab or bevacizumab in patients with neovascular age-related macular degeneration. Br J Ophthalmol 97:266–271
Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ (2011) Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 364:1897–1908
Yasuda S, Kondo M, Kachi S, Ito Y, Terui T, Ueno S, Terasaki H (2011) Rebound of macular edema after intravitreal bevacizumab therapy in eyes with macular edema secondary to branch retinal vein occlusion. Retina 31:1075–1082
Parodi MB, Iacono P, De Benedetto U, Cascavilla M, Bandello F (2012) Rebound effect after intravitreal dexamethasone implant for the treatment of macular edema secondary to central retinal vein occlusion. J Ocul Pharmacol Ther 28:566–568
Good TJ, Kimura AE, Mandava N, Kahook MY (2011) Sustained elevation of intraocular pressure after intravitreal injections of anti-VEGF agents. Br J Ophthalmol 95:1111–1114
Mayer WJ, Remy M, Wolf A, Kook D, Kampik A, Ulbig M, Reznicek L, Haritoglou C (2012) Comparison of intravitreal bevacizumab upload followed by a dexamethasone implant versus dexamethasone implant monotherapy for retinal vein occlusion with macular edema. Ophthalmologica 228:110–116
Acknowledgments
The authors maintain full control of all primary data, and have agreed to allow Graefes Archive for Clinical and Experimental Ophthalmology to review their data upon request. The authors have no financial interests in any device or drug mentioned in this study.
Grants
Financial support was provided by the Association for Research and Education in Ophthalmology (ARFO).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiquet, C., Dupuy, C., Bron, A.M. et al. Intravitreal dexamethasone implant versus anti-VEGF injection for treatment-naïve patients with retinal vein occlusion and macular edema: a 12-month follow-up study. Graefes Arch Clin Exp Ophthalmol 253, 2095–2102 (2015). https://doi.org/10.1007/s00417-015-2947-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-2947-9