Abstract
Purpose
Descemet membrane endothelial keratoplasty (DMEK) is a standard procedure in patients with endothelial corneal disorders. We investigated the difficulty of unfolding and attaching the graft lamella and its correlation to characteristics of the graft lamella donor, preoperative patient characteristics, and the postoperative outcome.
Methods
After preparation of the graft lamella, we prospectively graded the unfolding of the graft lamella in 169 consecutive DMEK procedures between September 2012 and August 2013 at the Charité-Universitätsmedizin Berlin with four different grades. Various donor characteristics and preoperative patient characteristics were analyzed and correlated to the grading. Additionally, visual acuity, corneal thickness and endothelial cell density were measured and correlated.
Results
Donor characteristics (age [range, 49 – 79 years], gender, endothelial cell density, total storage time, storage de-swelling time, postmortem time) did not correlate to the grading. Preoperative visual acuity significantly influenced the grade of unfolding and attaching of the graft lamella (p = 0.023), while all other preoperative parameters (age, gender, indication for DMEK, preoperative endothelial cell density and preoperative central corneal thickness) showed no correlation. Visual acuity improved significantly after surgery (p < 0.001, preoperative 0.73 ±0.43 LogMAR versus 0.31 ±0.28 LogMAR after one month, 0.25 ±0.29 LogMAR after three months, and 0.21 ±0.25 LogMAR after six months). Visual acuity did not differ significantly between the grading groups at any time point postoperatively. After 6 months, the mean loss rate of endothelial cell density was 24.7 %. Grading group IV developed significantly higher endothelial loss after one month, after three months and after six months compared to the other groups (p = 0.039, p = 0.008, p = 0.048). Graft detachment requiring an additional intracameral air injection to fix the graft detachment (re-bubbling) occurred in 61 eyes (38.1 %). In eyes graded IV, more re-bubblings were necessary than in all other groups (grade I: 37.0 %; grade II: 44.7 %; grade III: 43.8 %; grade IV: 50.0 %; p = 0.128; df = 3; χ 2 = 5.676).
Conclusion
There is no correlation between corneal donor tissue characteristics and the degree of difficulty of unfolding using graft lamella older than 49 years. Therefore, it is not possible to select grafts best suited for DMEK surgery on the basis of donor characteristics when the donor age is above 50 years. Preoperative visual acuity influences the grade of difficulty. The rate of graft detachments and endothelial cell loss increases significantly with a more difficult graft unfolding. The proposed grading system may therefore be relevant for postoperative management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Posterior lamellar keratoplasty, especially Descemet stripping (automated) endothelial keratoplasty (DSAEK) and Descemet membrane endothelial keratoplasty (DMEK), have become the standard treatments of corneal endothelial disorders like Fuchs corneal endothelial dystrophy and bullous keratopathy in the past years.
Both procedures replace the corneal endothelium selectively and are, therefore, less invasive corneal transplant techniques. In the DSEK procedure, first described by Melles et al. [1], the posterior corneal stroma, the Descemet membrane and the endothelium of a donor are transplanted [1–3]. In contrast, the DMEK procedure, first described by Melles, replaces the diseased endothelium and Descemet membrane by an isolated endothelium Descemet membrane layer without adherent corneal stroma [4, 5]. Whereas, in the DSAEK procedure the technique with graft preparation and graft unfolding is well standardized and reproducible DMEK surgery remains challenging [6], especially the main step, the unfolding of the lamella to attach the graft to the posterior stroma. Most of the manipulations to the graft occur during this step [6].
In our study, we graded the unfolding and attaching the graft lamella in the anterior chamber. We investigated if the more difficult unfolding correlated with donor characteristics, preoperative patient characteristics, the final outcome, visual acuity, the endothelial cell density, and the rate of re-bubbling.
Materials and methods
Patients
One-hundred sixty-nine consecutive DMEKs were performed at the Department of Ophthalmology, Charité – Universitätsmedizin Berlin, Campus Virchow Klinikum between September 2012 and August 2013 by one experienced surgeon (N.T.), who had previously performed more than 80 DMEK surgeries and was, therefore, no longer in the learning curve [7–9]. The DMEKs were analyzed prospectively. This study follows the ethical standards of the Declaration of Helsinki. Institutional ethical approval was obtained (EA2/108/12).
Donor characteristics
All patients received organ-cultured grafts from the Cornea Bank Berlin (University Tissue Bank, Institute of Transfusion Medicine, Charité – Universitätsmedizin Berlin). The minimum central endothelial density accepted for transplantation was 2,000 cells/mm2. Donor age and gender, the preoperative endothelial cell density, the total storage time in organ-culture, the storage deswelling time in dextran-containing media, and the postmortem time between cardiac arrest and cornealscleral excision were documented.
Surgical technique
The graft was prepared by stripping of the Descemet membrane from the donor corneal stroma immediately prior to transplantation as described in detail by Melles et al. [4, 5]. The diameter of the grafts were between 8.0 and 9.0 mm.
In all cases, clear corneal incisions without sutures were used. Descemetorhexis was performed with a diameter of 9.0 mm. In 54 of the 160 cases, a combined procedure (triple DMEK) with DMEK following standard cataract surgery was performed. A glass injector was used to insert the graft lamella into the anterior chamber. After injection, unfolding of the graft lamella was performed using the no touch technique as described by Dapena et al. [10]. We deviated from this technique only in grade IV cases. For unfolding the graft lamella, the rolled graft lamella was positioned with the opening in front of the approach. An air bubble was injected inside the graft lamella role. The air bubble was used to move the graft lamella into the correct position. After centering of the graft lamella, the air bubble was removed. After unfolding, the complete anterior chamber was filled with air and left for 1 h to attach the graft lamella. After 1 h, some of the air was released and exchanged with balanced salt solution (BSS) such that the anterior chamber was half-filled with air. The unfolding and attaching of the graft was graded as described below and documented after the intervention.
During the two weeks after surgery, an additional air injection (re-bubbling) was performed in eyes with a detached lamella graft and focal corneal edema for more than 2 clock hours.
Standard postoperative topical treatment in the first week included prednisolone acetate 1 % (five times daily), lubricant eye drops (five times daily) and oxfloxacin (five times daily). After one week, the ointment was stopped and prednisolone acetate 1 % was used topically (five times daily for the first month) with lubricant eye drops five times daily. The prednisolone acetate 1 % was tapered over a period of nine months.
Grading system
The unfolding and attaching of the graft lamella was graded with regards to its difficulty in four grading groups using the following specifications:
-
I.
Graft lamella primarily oriented correctly in the anterior chamber, straight and direct unfolding and centering;
-
II.
Slightly complicated, indirect unfolding and centering (duration less than five min);
-
III.
Difficult indirect unfolding and centering (duration longer than five min), repeated air injection with BSS exchange necessary;
-
IV.
Direct manipulation of the graft lamella for unfolding and centering by cannula or forceps.
Pre- and postoperative evaluation
We performed clinical examinations one day before the DMEK surgery as well as one, three and six months after the DMEK surgery. All examinations included an assessment of the best corrected visual acuity (BCVA; tested with a Snellen chart), a slit-lamp examination, applanation tonometry (Goldmann applanation tonometer, Haag Streit, Bern Switzerland or pneumatic tonometer, CT20D computerized Tonometer, Topcon, Japan), an endothelial cell density assessment (NONCON-ROBO CA specular microscope, Konan Medical Inc., Nishinomiya, Japan) and funduscopy. The Snellen decimal number was converted to logMAR visual acuity using a conversion table [11]. Preoperative central corneal thickness was analyzed using the Spectralis-OCT device with an anterior segment module (Spectralis optical coherence tomography, Heidelberg Engineering GmbH, Heidelberg, Germany).
Statistical methods
Statistical analysis was performed using IBM SPSS statistics 19 (SPSS Software, Munich, Germany). Normality was tested for all outcome measures. None of the measures followed a normal distribution. Therefore, nonparametric tests (Krukal-Wallis, Wilcoxon signed-rank test) were used for analysis. Descriptive statistics were expressed as the median and range or mean ± standard deviation (SD). Chi square distribution was used in order to analyze the distribution of proportions. Multivariate analysis was performed using multinomial logistic regression analysis for association of the donor characteristics/preoperative patient characteristics for the grading. Differences were considered statistically significant when p values were less than 0.05.
Results
One-hundred sixty-nine consecutive DMEKs were undertaken during the study period. The mean follow-up was 17.7 ±8.6 months. Nine eyes were excluded because of missing grading data during the DMEK surgery. Demographic, surgical and preoperative results are summarized in Table 1.
Grading system and preoperative patient characteristics
For 63 eyes, the DMEK surgery was assigned a grade I, for 47 eyes, a grade II, for 32 eyes, a grade III, and for 18 eyes, a grade IV. The preoperative central corneal thickness did not differ significantly between the four grading groups (grade I: 672.4 ±78.2 μm; grade II: 689.5 ±93.6 μm; grade III: 683.1 ±120.7 μm; grade IV: 697.7 ±117.1 μm; p = 0.833) as well as the preoperative endothelial cell density (p = 0.713). Preoperative visual acuity was significantly different between the grading groups (p = 0.017). Multinominal logistic regression showed a significant correlation between preoperative visual acuity and the grade of unfolding and attaching of the graft lamella (p = 0.023), while all other preoperative parameters (age, gender, indication for DMEK, preoperative endothelial cell density and preoperative central corneal thickness) showed no significantly correlation (p > 0.05).
Donor characteristics and grading system
Donor characteristics are presented in Table 2. Using the multinomial logistic regression we found that the donor characteristics did not significantly influence the grade of unfolding and attaching the graft lamella (p > 0.05).
Outcome and grading system
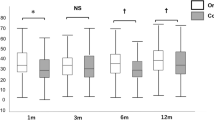
Visual acuity
Visual acuity data are presented in Fig. 1 and Table 3. Visual acuity improved significantly after surgery (p < 0.001, preoperative 0.73 ±0.43 LogMAR versus 0.31 ±0.28 LogMAR after one month, 0.25 ±0.29 LogMAR after three months and 0.21 ±0.25 LogMAR after six months). Preoperative visual acuity was significantly different between the grading groups (p = 0.017). But postoperatively, the visual acuity did not differ significantly between the grading groups at any time point (p = 0.453, p = 0.437, p = 0.910).
A retinal disease with macular involvement was present in 11 cases, diabetic macular edema was present in 3 cases (n = 3), age-related maculopathy was present in 5 cases (n = 5), iuxtafoveolar teleangiectasia was present in 1 case (n = 1), and epiretinal gliosis was present in 2 cases (n = 2). Visual acuity was reduced in four eyes because of a pre-existing amblyopia.
Endothelial cell density
Endothelial cell density decreased within the first month, a statistically significant decrease (p < 0.001; 2,279.2 ±270.2 cells/mm2 versus 1,796.0 ±463.3 cells/mm2). Between the first and third and the third and sixth month after surgery, no further statistically significant differences in endothelial cell density were observed (after 3 months: 1,792.3 ±428.1 cells/mm2, p = 0.247; after 6 months: 1,730.0 ±521.2 cells/mm2, p = 0.295). After 6 months, the mean loss rate of endothelial cell density was 24.7 %.
The mean endothelial cell density differs significantly between the grading groups at any time point postoperatively. Grading group IV developed a significantly higher endothelial loss after one month, after three and after six months compared to the other groups (p = 0.039, p = 0.008, p = 0.048; Fig. 2, Table 3).
Re-bubbling
Graft detachment requiring an additional intracameral air injection (re-bubbling) occurred in 61 eyes (38.1 %). Forty-six eyes received 1 air injection, 10 eyes received 2 air injections, 4 eyes received 3 air injections and 1 eye received 4 air injections. In the patient who needed 4 air injections, the cornea was very cloudy preoperatively. In all eyes the graft reattached. In eyes graded IV, more re-bubblings were necessary than in all other groups (grade I: 37.0 %; grade II: 44.7 %; grade III: 43.8 %; grade IV: 50.0 %; p = 0.128, df = 3, χ 2 = 5.676).
Complications
After 12 months, a clear cornea and attached grafts were achieved in all eyes (100 %). In one case, there was graft rejection (0.9 %). However, after steroid therapy, visual acuity recovered and reached 0.1 LogMAR.
Seven eyes (3.8 %) developed cystoid macular edema after surgery, which regressed and completely declined in all cases. Twenty-two eyes presented intraocular pressure (IOP) elevation during the follow-up period. In seventeen eyes, steroid-induced IOP elevation was suggested as a reason, as IOP normalized when local steroid administration was ceased.
Discussion
In this consecutive prospective study we investigated:
-
1.
The effects of cornea donor characteristics on the unfolding and attachment of the graft lamella to the posterior recipient stroma;
-
2.
The effects of preoperative patient characteristics on the difficulty of unfolding and attaching the graft lamella; and,
-
3.
The effects of the difficulty of unfolding and attaching the graft lamella on the clinical outcome.
In the first part of our study, we found no correlation between any corneal donor tissue characteristic, such as donor age, donor gender, preoperative endothelial cell density, total storage time, storage de-swelling time or postmortem time, and the difficulty of the surgery. Characteristics of the analyzed corneal donor were provided by the cornea bank, prior to preparation of the graft lamella before the DMEK surgery. Therefore, in our opinion it is not possible to select grafts best suited for surgery based on certain donor characteristics prior to the DMEK (preparation and surgery) in order to simplify the demanding step of unfolding and attaching the graft lamella during surgery. Similar results were described by Heindl et al. [12].
Heinzelmann et al. correlated donor characteristics to the width of DMEK grafts and to the duration of graft unfolding and postoperative endothelial cell loss [6]. They found donor age has an impact on the width of the DMEK graft rolls and that older grafts are faster to unfold; they surmised that the increased thickness and decreased elasticity of the older graft lamella are the reason for an easier unfolding [6]. Although this explanation is plausible and given that we also found differences in elasticity and width of the graft lamella during the preparation, we did not find a correlation between donor age and the difficulty of unfolding in our cohort. This might be due to the fact that, in our study, the donor age ranged between 49 and 79 years, in contrast to the study of Heinzelmann et al. that also involved grafts from younger donors (<40 years) [6]. Therefore, it might be that a donor age > 49 years has no influence on the difficulty of the DMEK surgery.
Additionally, we did not find an influence from total storage time and storage de-swelling time. Our grafts were stored in organ culture, which is widely used in Europe. Therefore, those results might be different for corneal grafts preserved in cold storage as it is known that the preparing/stripping of the Descemet membrane is easier in short-term-cultured donor corneas because those stored in organ culture seem to be more vulnerable [13].
By analyzing the influence of the preoperative patient characteristics on the difficulty of unfolding and attaching the graft lamella we found a correlation between the preoperative visual acuity and the difficulty, but no correlation between age, gender, the indication for DMEK, the preoperative endothelial cell density and/or the preoperative central corneal thickness and the difficulty of the procedure.
Although the elasticity and width of the graft lamella certainly play a decisive role for the degree of difficulty of the unfolding and attaching, as shown by Heinzelmann et al. [6], it seems that poor preoperative visual acuity leads to a more difficult DMEK surgery, possibly because the intraoperative insight is inferior and, therefore, the unfolding and attaching of the graft lamella becomes more difficult. Despite poor preoperative visual acuity, a comparable good postoperative visual acuity was achieved in all groups. Therefore, the limiting effect of preoperative visual acuity seems to be on corneal dysfunction and no other eye disease. Although there was no significant difference between the grading groups according to the preoperative central corneal thickness and no significant correlation between the grade of difficulty and the preoperative central corneal thickness, there was a tendency towards a larger preoperative central corneal thickness and, therefore, a more edematous cornea in group grade IV compared to group I. Additionally, it should be taken into account that not only the edema has an influence on the degree of pre-operative corneal dysfunction and, therefore, the preoperative visual acuity in patients with Fuchs endothelial dystrophy and bullous keratopathy, but also the grade of ultrastructural matrix changes, such as formation of epithelial bullae, sub-epithelial fibroblast and collagen infiltration, reduction of sub-basal corneal nerve density, reduced anterior keratocyte density and fibroblastic transformation of stressed keratocytes in the stroma [14]. As reported, there was no significant correlation between difficulty of unfolding and attachment of the graft lamella and the indication for DMEK. It seems that performing a DMEK surgery in patients with graft failure after DSAEK or penetrating keratoplasty is not automatically more difficult.
Investigating the difficulty for the clinical outcome, we found no differences for the four groups regarding the visual acuity. Independent of the difficulty of unfolding, a good postoperative visual acuity can be achieved. But although the prognosis for patients with a difficult surgery is still very good, they might require more intensive early postoperative care as we find a tendency for a higher re-bubbling rate in grading group IV, although not statistically significant (p = 0.128). While patients with an easy surgery (grade I) needed repeated air injection to attach the graft lamella in only 37.0 % of all cases, patients with a demanding surgery (graded IV) required repeated air injection in up to 50.0 % of the cases.
Poor sight might cause difficult centering of the graft lamella. A bad centering of the graft lamella could lead to an overlap of the graft lamella and the recipient's Descemet peripheral. Consequently, the graft lamella would have no contact with the posterior stroma and cannot attach tightly [15]. But again, these findings are in organ-cultured corneas and will likely be different in short-term-stored organs, as described by Laaser et al., that graft detachments occur more often in short-term-stored corneas [13].
We found a significant correlation (p = 0.048) between the grade of surgery difficulty and the six-month postoperative endothelial cell density. A higher manipulation rate by forceps or cannula (grade IV) leads to a reduction in endothelial cell density due to mechanical stress of the tissue in comparison to easier surgeries graded I-III, which were performed using a no-touch technique. Therefore, the no-touch technique should be attempted for the unfolding and attaching of the graft lamella. However, the different grades of difficulty I-III using the no-touch technique and, thus, the different surgical times, then seems to make no difference in the postoperative endothelial cell density. Although in our study the increased loss in group grade IV does not correlate with an impaired visual acuity six months, we need long term results to find out if those patients have any disadvantages because of their lower endothelial cell density.
To conclude, preoperative visual acuity influences the grade of difficulty, but we find no correlation between any corneal donor tissue characteristic and the degree of surgery difficulty. Therefore, it is not possible to select grafts that are appropriate for DMEK surgery on the basis of donor characteristics when the donor age is older than 50 years.
But if the surgery is demanding (grade IV), graft detachment seems to occur more often and early postoperative follow-up visits should be performed more frequently. Additionally, the postoperative endothelial cell loss increases if direct manipulation is necessary. Although this has no influence on the visual acuity six months postoperatively, long term results are needed.
References
Melles GR, Wijdh RH, Nieuwendaal CP (2004) A technique to excise the descemet membrane from a recipient cornea (descemetorhexis). Cornea 23(3):286–288
Price FW Jr, Price MO (2005) Descemet’s stripping with endothelial keratoplasty in 50 eyes: a refractive neutral corneal transplant. J Refract Surg 21:339–345
Price FW Jr, Price MO (2006) Descemet’s stripping with endothelial keratoplasty in 200 eyes: Early challenges and techniques to enhance donor adherence. J Cataract Refract Surg 32:411–418
Melles GR, Ong TS, Ververs B, van der Wees J (2006) Descemet membrane endothelial keratoplasty (DMEK). Cornea 25:987–990
Melles GR, Ong TS, Ververs B, van der Wees J (2008) Preliminary clinical results of Descemet membrane endothelial keratoplasty. Am J Ophthalmol 145(2):222–227
Heinzelmann S, Hüther S, Böhringer D, Eberwein P, Reinhard T, Maier P (2014) Influence of donor characteristics on descemet membrane endothelial keratoplasty. Cornea 33(6):644–648
Dapena I, Ham L, Droutsas K, van Dijk K, Moutsouris K, Melles GR (2011) Learning curve in Descemet’s membrane endothelial keratoplasty: first series of 135 consecutive cases. Ophthalmology 118(11):2147–2154
Droutsas K, Giallouros E, Melles GR, Chatzistefanou K, Sekundo W (2013) Descemet membrane endothelial keratoplasty: learning curve of a single surgeon. Cornea 32(8):1075–1079
Monnereau C, Quilendrino R, Dapena I, Liarakos VS, Alfonso JF, Arnalich-Montiel F, Böhnke M, Pereira NC, Dirisamer M, Parker J, Droutsas K, Geerling G, Gerten G, Hashemi H, Kobayashi A, Naveiras M, Oganesyan O, Orduña Domingo E, Priglinger S, Stodulka P, Torrano Silva J Jr, Venzano D, Vetter JM, Yiu E, Melles GR (2014) Multicenter study of descemet membrane endothelial keratoplasty: first case series of 18 surgeons. JAMA Ophthalmol 132(10):1192–1198
Dapena I, Moutsouris K, Droutsas K, Ham L, van Dijk K, Melles GR (2011) Standardized “no-touch” technique for descemet membrane endothelial keratoplasty. Arch Ophthalmol 129(1):88–94
Joussen AM, Heussen FM, Joeres S, Llacer H, Prinz B, Rohrschneider K, Maaijwee KJ, van Meurs J, Kirchhof B (2006) Autologous translocation of the choroid and retinal pigment epithelium in age-related macular degeneration. Am J Ophthalmol 142(1):17–30
Heindl LM, Bucher F, Caramoy A, Hos D, Matthaei M, Cursiefen C (2014) Safety of donor tissue preparation and use of descemetoschisis and torn tissue in descemet membrane endothelial keratoplasty. Cornea 33(10):e7–e9
Laaser K, Bachmann BO, Horn FK, Schlötzer-Schrehardt U, Cursiefen C, Kruse FE (2011) Donor tissue culture conditions and outcome after descemet membrane endothelial keratoplasty. Am J Ophthalmol 151(6):1007–1018
Zhang J, Patel DV (2015) The pathophysiology of Fuchs’ endothelial dystrophy - A review of molecular and cellular insights. Exp Eye Res 130C:97–105
Dirisamer M, van Dijk K, Dapena I, Ham L, Oganes O, Frank LE, Melles GR (2012) Prevention and management of graft detachment in descemet membrane endothelial keratoplasty. Arch Ophthalmol 130(3):280–291
Acknowledgments
The authors thank Simone Baar and Dirk Scharf for technical support.
Anna-Karina B. Maier financial support provided by the “Friedrich C. Luft” Clinical Scientist Pilot Program funded by the Volkswagen Foundation and the Charité Foundation
Enken Gundlach financial support provided by the “Ernst und Bertha Grimmke Stiftung.”
Competing interest
None declared for all authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Anna-Karina B. Maier and Enken Gundlach contributed equally to this work.
Rights and permissions
About this article
Cite this article
Maier, AK.B., Gundlach, E., Schroeter, J. et al. Influence of the difficulty of graft unfolding and attachment on the outcome in descemet membrane endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol 253, 895–900 (2015). https://doi.org/10.1007/s00417-015-2939-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-2939-9