Abstract
Purpose
To investigate the relationship between circulation hemodynamics and morphology in the choroid during systemic corticosteroid therapy for patients with Vogt–Koyanagi–Harada (VKH) disease.
Methods
This retrospective case series includes 18 eyes of nine patients with VKH disease (two men and seven women; average age, 40.8 years) who received systemic corticosteroid therapy. Laser speckle flowgraphy (LSFG) and enhanced-depth imaging optical coherence tomography (EDI-OCT) were performed before treatment and at 1 week and 1 and 3 months after treatment. The average values of the mean blur rate (MBR) at the macula and the central choroidal thickness (CCT) were compared at each stage.
Results
The changing rates of the average MBR significantly increased at all examinations after the start of treatment compared with the pre-treatment value with resolution of serous retinal detachment (SRD) (P = 0.0002 for all). The CCT decreased significantly at all examinations after the start of treatment compared with the pre-treatment value (P = 0.0002 for all). Changes in MBR and CCT during the 3-month follow-up period correlated significantly (R = −0.5913, P = 0.0097). The best-corrected visual acuity at pre-treatment correlated significantly with the changing rate of the MBR from 0 to 3 months (R = 0.5944, P = 0.0093) but not with CCT.
Conclusions
Our data suggest that circulatory disturbances and increased thickness of the choroid relate to the pathogenesis of VKH disease with link mutually. LSFG is useful as an index for evaluating the choroiditis activity of VKH disease as well as EDI-OCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vogt–Koyanagi–Harada (VKH) disease is a multisystemic syndrome that may be caused by autoimmunity against melanocytes [1]. In the eye, this disease initially targets the choroid, and its histopathology is characterized by diffuse infiltration of lymphocytes with focal granulomas in the choroidal stroma [2]. Large doses of systemic corticosteroid administered as early as possible after disease onset may prevent recurrence [3]. Therefore, ophthalmologists must evaluate the severity of inflammation in the choroidal stroma in tapering the dose of systemic corticosteroids; however, the most suitable indices for this purpose are not established.
Recent studies using enhanced-depth imaging optical coherence tomography (EDI-OCT) and swept-source OCT (SS-OCT) show that choroidal thickness increases markedly in acute VKH disease, and rapidly decreases together with the resolution of serous retinal detachment (SRD) after administration of systemic corticosteroids [4, 5]. Moreover, an increase in choroidal thickness recurs concurrently with recurrence of SRD [6, 7]. Therefore, measurements of choroidal thickness may be useful as an index of evaluating disease activity quantitatively. However, it is difficult to quantitate choroidal thickness in the initial stage of VKH disease even using SS-OCT, because the thickness often increases beyond 1,000 μm [4–6]. Moreover, pretreatment choroidal thickness has been shown not to correlate with retinal thickness or visual acuity [5]. These observations suggest that choroidal thickness measurements using available techniques are not sufficiently robust to provide an index of choroiditis activity.
Laser speckle flowgraphy (LSFG) is a noninvasive technique that determines choroidal blood flow velocity [8, 9]. LSFG evaluates the blood flow of the deep choroidal layers, particularly in the macular area [10], and has the advantage of providing quantitative and repeated measurements of choroidal circulation at intervals during the course of a disease [11–16]. We previously showed using LSFG that square blur rate, a relative value of the blood flow at the macula, increased significantly over time together with improved visual acuity during systemic corticosteroid therapy of the eyes of patients with VKH disease [11], suggesting that LSFG is a potent technique for evaluating disease activity. A modified system, LSFG-NAVI generates mean blur rate (MBR), a new index of the blood flow (MBR = 2 × SBR) , and can obtain reproducible data in a short time of approximately 4 seconds [17]. However, there are no studies on the relationship between choroidal blood flow velocity and choroidal thickness or visual acuity in chorioretinal diseases, including VKH disease [18]. The aim of this study, therefore, was to examine relationships between choroidal blood flow, choroidal thickness, and visual acuity in VKH disease by measuring sequential changes in the thickness of the choroid as well as blood flow during systemic corticosteroid therapy. We used EDI-OCT and LSFG to analyze these variables in patients with VKH disease.
Methods
Patients and diagnosis
This observational case series included 18 eyes of nine patients [two men and seven women aged 40.8 years ± 14.0; mean ± standard deviation (SD)] with VKH disease who were admitted to Hokkaido University Hospital from July 2012 to May 2014. Their medical records were retrospectively reviewed. All patients were treatment-naïve at an early stage of disease, and were followed using LSFG and EDI-OCT. VKH disease was diagnosed according to the criteria of Sugiura [19] and the VKH Disease Committee [20]. Exclusion criteria were as follows: patients who were unable to undergo LSFG or EDI-OCT, patients with presumed recurrent disease with the sunset glow fundus at the initial visit, patients with bullous retinal detachment at the macula, and patients with poor fixation due to poor visual acuity. None of the patients had any medical or ocular history, including systemic or ocular hypertension and ocular trauma or surgery. The current study was approved by the ethics committee of Hokkaido University Hospital, and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects for chart review after the nature and possible consequences of the study had been explained.
Treatment
Administration of prednisolone was started at 200 mg⁄day. The tapering schedule for prednisolone required intravenous (i.v.) administration of 200 mg⁄day, 150 mg⁄day, and 100 mg⁄day, with each dose administered over a 2-day period. After the first 6 days of i.v. administration, tapering was continued using oral doses according to the following schedule: 4 days at 60 mg⁄day, 10 days at 40 mg⁄day, 14 days at 30 mg⁄day, 1 month at 20 mg⁄day, 1 month at 15 mg⁄day, 1 month at 10 mg⁄day, 1 month at 7.5 mg⁄day, and 1 month at 5 mg⁄day. No other immunosuppressants were administered. No recurrence of uveitis was noted within 3 months of the initiation of systemic corticosteroid therapy.
Ophthalmologic examination
On the initial visit, all patients underwent a complete ophthalmic examination, including decimal best-corrected visual acuity (BCVA), indirect ophthalmoscopy, fundus photograph, fluorescein angiography (FA), indocyanine green angiography spectral-domain OCT (cross-sectional retinal B-scans of 5 × 5 lines), EDI-OCT (RS-3000 Advance; Nidek Co., Ltd., Gamagori, Japan), and LSFG. During follow-up, BCVA assessment and EDI-OCT were performed at pre-treatment, every week for 1 month after treatment, and every month thereafter.
EDI-OCT
Using EDI-OCT, the central choroidal thickness (CCT) was determined by manually measuring the distance from the outer border of the hyperreflective line corresponding to the retinal pigment epithelium (RPE) to the outer border of the choroid beneath the fovea, using a horizontal scan through the fovea. Further, the height of SRD within 3 mm from the fovea was examined by manually measuring from the outer border of the RPE to the outer border of the detached sensory retina. YH and KH independently evaluated OCT images in a masked fashion, not knowing any subject’s clinical information. When choroidal thickness reached >800 μm, these were defined as 800 μm, because the inner scleral border could not be visualized using EDI-OCT. We determined the statistical significance of the differences in average CCT values between each stage.
LSFG
LSFG measurements using LSFG-NAVI (Softcare, Fukuoka, Japan) were conducted 5 consecutive times for each phase before treatment, and at 1 week and 1 and 3 months after initiation of systemic prednisolone therapy. The mechanism of LSFG has been published [8, 9]. The pupils of the subjects were dilated with 0.5 % tropicamide and 0.5 % phenylephrine hydrochloride. To evaluate the changes in the relative blood flow velocity, a circle was set at the fovea (Fig. 1f, h, j). The positions of circles were determined manually by comparing the fundus photograph and the LSFG color map images, sparing the large retinal vessels. The MBR was calculated in each circle using LSFG Analyzer software (v 3.0.47; Softcare) that automatically set each circle at the same site where a circle had been set at baseline during follow-up. To evaluate changes in average MBR, the changing rate of the average MBR relative to the initial baseline value was utilized [12, 13, 16], because MBR is a quantitative index of the “relative” blood flow velocity.
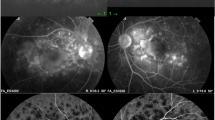
Images of the right eye in a patient with Vogt–Koyanagi–Harada (VKH) disease (case 3). a The fundus shows serous retinal detachment (SRD) extending from the optic disc to the posterior pole, choroidal folds, and optic disc swelling at the initial visit. b Late-phase fluorescein angiography shows subretinal pooling of the dye corresponding to SRD and leakage from the optic disc. c Initial-phase indocyanine green angiography (ICGA) shows fuzzy choroidal vessels at the posterior pole. d ICGA 10 min after the dye injection shows multiple hypofluorescent spots extending beyond the posterior pole. e–j Images of enhanced-depth imaging optical coherence tomography (EDI-OCT; e, g, i) and laser speckle flowgraphy (LSFG; f, h, j). e EDI-OCT at pre-treatment demonstrates SRD at the macular area and marked choroidal thickening. Central choroidal thickness (CCT) was >800 μm. g, i The CCT sequentially decreased to 472 μm and 378 μm at 1 month (g) and 3 months (i) after the initiation of systemic corticosteroid administration respectively, together with the resolution of macular SRD. f, h, j Composite color maps of the mean blur rate (MBR) measured using LSFG. The warm and cool colors indicate high and low MBR respectively. The MBR at the macula (within a circle) was 6.0, 11.6, and 12.0 at pre-treatment (f), and 1 month (h) and 3 months (j) after treatment, respectively, and increased thereafter
Hemodynamics
There is a linear relationship between choroidal blood flow and ocular perfusion pressure (OPP) [21]. The patient’s blood pressure and intraocular pressure (IOP) were measured after each LSFG measurement. Mean blood pressure (mBP) was calculated from systolic blood pressure (sBP) and diastolic blood pressure (dBP), according to the following equation: mBP = dBP + 1/3(sBP−dBP) [22]. OPP was calculated using the following equation: OPP = 2/3 mBP–IOP. The significance of variations in IOP, mBP, and OPP before treatment, and at 1 week and 1 and 3 months after treatment, were evaluated using statistical tests.
Statistical analyses
All results were expressed as the mean ± SD. The BCVA was converted to the logarithm of minimal angle of resolution (logMAR). The Friedman test and/or Wilcoxon signed rank test were used to compare changes in logMAR BCVA, the height of SRD, CCT, the changing rate of MBR, and OPP. Spearman’s rank correlation test was used to determine the relationship between the changing rate of the MBR and the CCT, and the MBR or CCT and variables including logMAR BCVA and SRD height. For all tests, P < 0.05 was considered statistically significant.
Results
Ocular findings and retinal morphology
Ocular findings in eyes with VKH disease are summarized in Table 1. Before treatment, SRD was present in 14 of 18 eyes in the macular area, surrounding of the optic disc, or both. It was detected by OCT retinal scan in nine eyes especially in the macular area. SRD was reduced 1 week after treatment, and was undetectable in all eyes within 3 months after treatment. The height of SRD was reduced significantly at 1 week and later compared with the pre-treatment value (P = 0.0117 for all). The BCVA improved to more than 1.0 in all except two eyes 3 months after treatment.
CCT
The CCT of all eyes 3 months after treatment markedly decreased compared with pretreatment values (Figs. 1e, g, i, 2a, Table 2). There was a statistically significant difference in the CCT values during the 3-month follow-up period (Friedman test, P = 0.000000012) and significant decreases at all examinations after the start of treatment against the pre-treatment value (Fig. 2a, Wilcoxon signed rank test, P = 0.0002 for all).
Changes in CCT measured using EDI-OCT (a) and MBR at the macular region (circles shown in Fig. 1f, h, j) measured using LSFG (b) during the 3 months after the initiation of systemic corticosteroid therapy in patients with VKH disease. a The mean CCT decreased gradually after systemic corticosteroid treatment, and the values at all examinations after the start of treatment were significantly reduced compared with the pre-treatment value. b Changing rates of the average macular MBR values relative to baseline values (100 %) increased with time, and significantly increased at all examinations after the start of treatment compared with the pre-treatment value
MBR
The MBR values at the macula gradually increased compared with the pre-treatment values in all eyes (Fig. 1f, h, j, Table 2). When the changes of macular MBRs were compared with the pre-treatment value (100 %), increases of 50.2 ± 37.6 %, 74.3 ± 52.8 %, and 80.8 ± 46.2 % were detected at 1 week and 1 and 3 months after treatment respectively (Fig. 2b). There was a statistically significant increase in the MBR changing rate values (Friedman test, P = 0.000000025), and significant increases at all examinations after the start of treatment compared with the pre-treatment value (Fig. 2b, Wilcoxon signed rank test, P = 0.0002 for all).
Correlation between MBR and CCT or BCVA
There was a statistically significant inverse correlation between the increase in the magnitude of the MBR changing rate and the decrease of the changing rate of CCT during the 3-month follow-up period after treatment was initiated (Fig. 3a, R = −0.5913, P = 0.0097). There was a positive correlation between the increase in the magnitude of the changing rate of the MBR and the logMAR values of the BCVA at pre-treatment (Fig. 3b, R = 0.5944, P = 0.0093).
Correlation between the MBR and CCT or the best-corrected visual acuity (BCVA). a There was a statistically significant inverse correlation between the decreased or increased changing rates of CCT and MBR during the 3-month follow-up period with systemic corticosteroid therapy. b There was a statistically significant positive correlation between the logMAR BCVA at pre-treatment and the increased amount of macular MBR changing rate during the 3-month follow-up period
Correlation between CCT and BCVA
The differences between the decrease of CCT (0–3 months) and pre-treatment BCVA were not statistically significant (R = 0.3942, P = 0.1055). Moreover, there were no significant correlations between the decrease of CCT and BCVA improvement (0–3 months) (R = −0.1103, P = 0.6630).
Correlation between height of SRD and other variables
There was a statistically significant correlation between the pre-treatment values of the SRD height and BCVA (R = 0.8367, P = 0.000015) and the decrease in SRD height and the BCVA changes during the 3-month follow-up period (R = −0.8328, P = 0.000018). There was a significant correlation between the SRD height at pre-treatment and the differences of MBR (0–3 M) (R = 0.4815, P = 0.0431), but not between the SRD height at pre-treatment and the CCT change (0–3 M) (R = 0.1235, P = 0.6254).
OPP and hemodynamics
The mean OPP was 40.7 ± 3.4, 38.5 ± 4.0, and 39.6 ± 5.3 mmHg at pre-treatment and 1 and 3 months after treatment respectively. There were no significant differences between pre-treatment values and values at 1 month or 3 months after treatment (P = 0.1989, P = 0.4204, respectively).
Discussion
In the present study, using LSFG and EDI-OCT to analyze patients with VKH disease who received systemic corticosteroid therapy, we made the following observations:
-
(1)
Macular MBR significantly increased over time after treatment, whereas CCT decreased significantly together with improvement of BCVA and SRD.
-
(2)
There was a negative correlation in the changing rates of MBR and CCT during the 3-month follow-up period after initiation of therapy.
-
(3)
BCVA at pre-treatment significantly correlated with the changing rate of MBR but not that of CCT during the 3-month follow-up.
-
(4)
Height of SRD at pre-treatment significantly correlated with MBR changes (0–3 M) but not with CCT changes.
In the present study, the changes in choroidal blood flow velocity and thickness correlated negatively during systemic corticosteroid therapy of patients with VKH disease. This result suggests that there is a causal relationship between choroidal circulation and morphology. The relationship may be explained as follows: diffuse infiltration of lymphocytes, which is histopathologically observed in VKH disease [2], compresses the vessels in the choroidal stroma, leading to decreased blood flow; inflammation extending to the choroidal vessels causes vascular hyperpermeability and the resultant accumulation of the fluids in the choroidal stroma, leading finally to a marked increase of choroidal thickness. Systemic corticosteroid therapy may reverse these adverse effects after inflammation of the choroid resolves. Taken together, the close link between the MBR and CCT during treatment suggests that both factors are critically involved in the pathogenesis of VKH disease and serve as a useful index for evaluating choroiditis activity.
The present study revealed a statistical correlation between changes of MBR and BCVA or the SRD height before treatment, suggesting a close link between the extent of the alteration of choroidal circulation and initial visual function in VKH disease. In contrast, there was no significant correlation between CCT and initial BCVA or the height of SRD at pre-treatment which is consistent with the results of another study [5]. The reason may be that accurate measurements of choroidal thickness in the initial stage of this disease are difficult using available techniques. Therefore, our findings suggest that MBR is more likely than CCT to serve as a sensitive index for evaluating choroiditis activity in VKH disease.
MBR is a relative value of blood flow velocity. However, the MBR within the optic nerve head of rabbits or nonhuman primates directly and linearly correlates with capillary blood flow determined using the hydrogen gas clearance method or the microsphere method that yields an absolute value [23, 24]. MBR would serve as a more useful index for evaluating disease activity if it could evaluate absolute values. However, this will require further advances in LSFG technology. In the present study, there was a statistically significant correlation between pre-treatment MBR values and initial BCVA (data not shown).
The present study has some limitations. First, this study is retrospective and analyzed a small number of cases. Second, the presence of SRD at the macula before treatment may affect the MBR measurements. However, eyes with bullous retinal detachment at the measurement site were not included in this study. LSFG evaluates mainly blood flow in the choroidal deep layers [10], because LSFG employs a wavelength of 830 nm, similar to that of ICGA. In investigation using LSFG in acute CSC, there were similar changes in MBR at the fovea with SRD and the perifoveal area without SRD with regression of CSC [12]. Thus, the effect of SRD on MBR measurements appears to be minimal or negligible in the present study. Further studies are required to establish indices that evaluate choroiditis activity.
In conclusion, our use of EDI-OCT and LSFG to evaluate patients with VKH disease who were treated with systemic corticosteroid shows that blood flow velocity in the choroid negatively correlated with its thickness. Moreover, the BCVA before treatment correlated with choroidal blood flow but not choroidal thickness. These results suggest that circulatory disturbances and increased thickness of the choroid caused by choroiditis in VKH disease are closely linked, and that MBR is useful for noninvasively monitoring the choroiditis activity of VKH disease as well as for determining choroidal thickness.
References
Sugita S, Takase H, Taguchi C, Imai Y, Kamoi K, Kawaguchi T, Sugamoto Y, Futagami Y, Itoh K, Mochizuki M (2006) Ocular infiltrating CD4+ T cells from patients with Vogt–Koyanagi–Harada disease recognize human melanocyte antigens. Invest Ophthalmol Vis Sci 47:2547–2554
Rao NA (2007) Pathology of Vogt–Koyanagi–Harada disease. Int Ophthalmol 27:81–85
Kitaichi N, Horie Y, Ohno S (2008) Prompt therapy reduces the duration of systemic corticosteroids in Vogt–Koyanagi–Harada disease. Graefes Arch Clin Exp Ophthalmol 246:1641–1642
Maruko I, Iida T, Sugano Y, Oyamada H, Sekiryu T, Fujiwara T, Spaide RF (2011) Subfoveal choroidal thickness after treatment of Vogt–Koyanagi–Harada disease. Retina 31:510–517
Hosoda Y, Uji A, Hangai M, Morooka S, Nishijima K, Yoshimura N (2014) Relationship between retinal lesions and inward choroidal bulging in Vogt–Koyanagi–Harada disease. Am J Ophthalmol 157:1056–1063
Nakai K, Gomi F, Ikuno Y, Yasuno Y, Nouchi T, Ohguro N, Nishida K (2012) Choroidal observations in Vogt–Koyanagi–Harada disease using high-penetration optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 250:1089–1095
Hashizume K, Imamura Y, Fujiwara T, Machida S, Ishida M, Kurosaka D (2014) Choroidal thickness in eyes with posterior recurrence of Vogt–Koyanagi–Harada disease after high-dose steroid therapy. Acta Ophthalmol 92:e490–e491
Tamaki Y, Araie M, Kawamoto E, Eguchi S, Fujii H (1994) Noncontact, two-dimensional measurement of retinal microcirculation using laser speckle phenomenon. Invest Ophthalmol Vis Sci 35:3825–3834
Sugiyama T, Araie M, Riva CE, Schmetterer L, Orgul S (2010) Use of laser speckle flowgraphy in ocular blood flow research. Acta Ophthalmol 88:723–729
Isono H, Kishi S, Kimura Y, Hagiwara N, Konishi N, Fujii H (2003) Observation of choroidal circulation using index of erythrocytic velocity. Arch Ophthalmol 121:225–231
Hirose S, Saito W, Yoshida K, Saito M, Dong Z, Namba K, Satoh H, Ohno S (2008) Elevated choroidal blood flow velocity during systemic corticosteroid therapy in Vogt–Koyanagi–Harada disease. Acta Ophthalmol 86:902–907
Saito M, Saito W, Hashimoto Y, Yoshizawa C, Fujiya A, Noda K, Ishida S (2013) Macular choroidal blood flow velocity decreases with regression of acute central serous chorioretinopathy. Br J Ophthalmol 97:775–780
Saito M, Saito W, Hashimoto Y, Yoshizawa C, Shinmei Y, Noda K, Ishida S (2014) Correlation between decreased choroidal blood flow velocity and the pathogenesis of acute zonal occult outer retinopathy. Clin Exp Ophthalmol 42:139–150
Hirooka K, Saito W, Hashimoto Y, Saito M, Ishida S (2014) Increased macular choroidal blood flow velocity and decreased choroidal thickness with regression of punctate inner choroidopathy. BMC Ophthalmol 14:73
Takahashi A, Saito W, Hashimoto Y, Saito M, Ishida S (2014) Impaired circulation in the thickened choroid of a patient with serpiginous choroiditis. Ocul Immunol Inflamm 22:409–413
Hashimoto Y, Saito W, Saito M, Hirooka K, Mori S, Noda K, Ishida S (2014) Decreased choroidal blood flow velocity in the pathogenesis of multiple evanescent white dot syndrome. Graefes Arch Clin Exp Ophthalmol. doi:10.1007/s00417-014-2831-z
Aizawa N, Yokoyama Y, Chiba N, Omodaka K, Yasuda M, Otomo T, Nakamura M, Fuse N, Nakazawa T (2011) Reproducibility of retinal circulation measurements obtained using laser speckle flowgraphy-NAVI in patients with glaucoma. Clin Ophthalmol 5:1171–1176
Saito M, Saito W, Ishida S (2013) Authors’ response to ‘Choroidal blood flow measurement with laser speckle flowgraphy in macular disease’. Br J Ophthalmol 97:1083–1084
Sugiura S (1978) Vogt–Koyanagi–Harada disease. Jpn J Ophthalmol 22:9–35
Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, Arellanes-Garcia L, Pivetti-Pezzi P, Tessler HH, Usui M (2001) Revised diagnostic criteria for Vogt–Koyanagi–Harada disease: report of an international committee on nomenclature. Am J Ophthalmol 131:647–652
Riva CE, Titze P, Hero M, Petrig BL (1997) Effect of acute decreases of perfusion pressure on choroidal blood flow in humans. Invest Ophthalmol Vis Sci 38:1752–1760
Okuno T, Sugiyama T, Kohyama M, Kojima S, Oku H, Ikeda T (2006) Ocular blood flow changes after dynamic exercise in humans. Eye 20:796–800
Takahashi H, Sugiyama T, Tokushige H, Maeno T, Nakazawa T, Ikeda T, Araie M (2013) Comparison of CCD-equipped laser speckle flowgraphy with hydrogen gas clearance method in the measurement of optic nerve head microcirculation in rabbits. Exp Eye Res 108:10–15
Wang L, Cull GA, Piper C, Burgoyne CF, Fortune B (2012) Anterior and posterior optic nerve head blood flow in nonhuman primate experimental glaucoma model measured by laser speckle imaging technique and microsphere method. Invest Ophthalmol Vis Sci 53:8303–8309
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirooka, K., Saito, W., Namba, K. et al. Relationship between choroidal blood flow velocity and choroidal thickness during systemic corticosteroid therapy for Vogt–Koyanagi–Harada disease. Graefes Arch Clin Exp Ophthalmol 253, 609–617 (2015). https://doi.org/10.1007/s00417-014-2927-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2927-5