Abstract
Background
To evaluate the efficacy of intravenous erythropoietin (EPO) on improvement of visual function and color vision in patients with recent indirect traumatic optic neuropathy (TON).
Methods
In a case series, 18 eyes of 18 patients with diagnosis of indirect TON with duration of less than 2 weeks underwent 20,000 IU intravenous EPO injections daily for 3 days. Best corrected visual acuity (BCVA) and color vision were checked by Ishihara test before, 1, and 3 months after injections. BCVA and color vision were compared before, 1, and 3 months after injections.
Results
The mean BCVA improved from a baseline of 2.21 ± 0.97 to 1.48 ± 1.29 and 1.31 ± 1.27 log MAR at months 1 and 3, respectively. The differences were statistically significant (P = 0.001, P < 0.001). Color vision was changed from a baseline 2.24 ± 4.29 to 2.94 ± 4.64 and 3.41 ± 5.09 plates at months 1 and 3, respectively. We observed some qualitative improvement that was, however, statistically insignificant at the time of evaluation. (P = 0.063, P = 0.068).
Conclusion
This case series showed noticeable effect of EPO on improvement of visual function in patients with recent indirect TON.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic optic neuropathy (TON) refers to any optic nerve damage secondary to trauma that occurs in approximately 0.5 to 5 % of closed-head injuries, and in 2.5 % patients with maxillofacial trauma and mid-face fracture [1, 2]. TON results in variable degrees of optic atrophy and decreased visual function. It can be classified depending on the site of injury or according to the mode of injury (direct or indirect). Indirect TON results from injury to the optic nerve axons in the bony optic canal induced by shearing forces that are transmitted to the fibers or to the vascular supply of the nerve, and eventually leads to retinal ganglion cell apoptosis. Currently there are different management modalities for these patients that include (1) observation, (2) medical treatment with high-dose steroid, and (3) optic canal decompression. The results of these medical and surgical interventions have shown to be uncertain with possible serious side effects or complications at present [3–6].
There is no proven treatment for TON. It has recently been shown that the cytokine hormone erythropoietin (EPO), which had been long known and used as an agent to promote hematopoiesis, is able to reduce neuronal apoptosis and exert protective effect in experimental models of mechanical trauma, neuronal inflammation, cerebral and retinal ischemia, and oxidative stress, and most notably in an animal model of optic nerve transaction [7, 8].
Recently, there are some reports about beneficial effects of EPO in the treatment of the patients with diagnosis of non arthritic anterior ischemic optic neuropathy [9, 10].
To the best of our knowledge, there is one report of using EPO in TON in humans [11]. Results of recent studies on biologic and pharmacologic effect of EPO encouraged us to assess its effect on patients with indirect TON.
To the best of our knowledge, this is the second and largest case series on the effect of EPO in TON. The aim of this study is to evaluate the effect of EPO in visual function and color vision in recent indirect TON.
Methods
In a pilot study, all patients with diagnosis of indirect TON who were referred to the Emam Hossein Hospital from 2010 to 2013 were included. All patients with decreased vision after closed-head and craniofacial trauma were carefully examined by ophthalmologists. A complete examination including BCVA (best corrected visual acuity), RAPD (rapid afferent papillary defect), color vision, slit-lamp examination. and funduscopy were performed. A high resolution orbital (coronal and axial) and optic canal computed tomography scan were obtained. Patients underwent pupillary assessments with the swinging flashlight test and grading of the RAPD with neutral density filters by an examiner (PJS) as described by Thompson et al. [12]. Color vision, evaluated by Ishihara color plates were tested in each eye separately while the other eye was occluded. Then numbers of the diagnosed plates were considered.
The diagnosis of indirect TON was considered in the presence of decreased visual acuity with an RAPD and defective color vision with no ocular or direct optic nerve damage. The patients were evaluated by a neurosurgeon if there were no indications for decompression surgery; they were included in this study. Patients with the following criteria were included: (1) interval between trauma and admission less than 14 days, (2) eye with normal fundus, and (3) indirect TON . The following patients were excluded: (1) penetrating trauma, (2) other accompanying ocular lesions that cause decreased vision, (3) media haziness, (4) optic nerve avulsion and direct TON, (5) eyes needing optic nerve decompression surgery, (6) TON with blow-out fracture, (7) pregnancy, and (8) history of thromboembolic event.
Ophthalmic examination was repeated at 1, 2, 3, and 7 days and 1, 3 months after treatment. A general physical examination was performed by an internist before and during treatment daily, 1, and 3 months. Blood testing including complete blood cell count, serum urea, creatinine, and electrolytes was done before treatment, and at 3 days, 1, and 3 months after treatment. The study protocol and its complications, safety, and efficacy were explained to all patients before recruitment. Informed consent was obtained from each patient. This pilot study was approved by the review board/ethics committee of the ophthalmic research center of the university.
The patients received EPO 20,000 IU via intravenous infusion line with 300 ml of normal saline over 30 min daily for 3 days under supervision of an internist. Blood pressure was measured on the left arm with the patient maintained in a 30 degree head-up tilt immediately before and 15, 30, 60, and 120 min after starting EPO infusion.
Data including age, sex, type of trauma, interval between trauma and treatment, initial visual acuity, and color vision 1 and 3 months after treatment were recorded. Data were entered with software SPSS (Version 17.0, SPSS Co, Chicago, IL, USA). They were presented using mean ± SD, and frequency (%). Wilcoxon signed rank test was used for statistical analysis. P-values less than 0.05 were considered statistically significant.
Results
In this pilot study, 18 eyes of 18 patients with diagnosis of indirect TON were enrolled to receive intravenous EPO. Mean age of patients was 36 years (SD = 16, range 8–65 years).
Demographic data and clinical characteristics of the patients are shown in Table 1. The interval time between injuries to the treatment ranged from 8 to 240 h (66.66 ± 74.81) Initial visual acuity ranged between no light perception (NLP) to 3/10 with a mean of 2.21 ± 0.97. LogMAR was improved for NLP to 8/10 with a mean of 1.48 ± 1.29 logMAR at 1 month and NLP to 10/10 with a mean of 1.31 ± 1.27 at 3 months. The differences were statistically significant (P = 0.001, P < 0.001, p < 0.001). Color vision was changed from a baseline 2.24 ± 4.29 to 2.94 ± 4.64 and 3.41 ± 5.09 plates at months 1 and 3, respectively. In spite of this objective improvement, the difference was not statistically significant (P = 0.063, P = 0.068) (Table 1). No side-effects related to EPO was observed.
We evaluated the relation between the progression of changes of visual acuity and color vision with other factors like association with age, gender, trauma type, trauma time, baseline BCVA, baseline APD, the interval between trauma and management with EPO, and type of trauma in Table 2, but we didn’t find any statistically significant relation.
Discussion
The pathophysiology of indirect TON is multifactorial and it has been proposed that primary and secondary injury may occur. Retinal ganglion cells (RGCs) are specialized cells within the optic nerve and form part of an intricate chain responsible for transmitting information to the cortex of the brain. Following trauma there is an immediate shearing of a portion of RGCS axons, an irreversible process with subsequent RGC degeneration. It is postulated that there is then an optic nerve swelling secondary to direct mechanical trauma or macular ischemia, thus further impairing the already compromised blood supply to surviving RGCs setting up a downward spiral toward cell death [7, 13].
EPO, a glycoprotein hormone, is synthesized predominantly in the kidney and is secreted by interstitial cells of the adrenal cortex. In response to tissue hypoxia, EPO was first characterized as a hematopoietic growth factor that regulates red blood cell production by promoting survival, proliferation, and differentiation, and differentiation of erythroid progenitors in bone marrow [14]. Recently, EPO has also been shown to exhibit neuroprotective effects of neurons of the central nervous system. Systemic administration of EPO is neuroprotective in animal models of stroke, mechanical trauma, exitotoxic injury, and neuroinflammation [15].
In other studies, long-term, high-dose EPO treatment was found to be safe and well tolerated. They showed that high-dose EPO had neuroprotective and neuroregenerative effects in comparison with low-dose treatment without any side-effects [16, 17].
Tan et al. demonstrated that the RHA/ROCK pathway was involved in the effect of erythropoietin to promote RGCs axonal regeneration in a rat optic nerve crush [18].
In another study that was done by Rong et al., they compared that sustained EPO loaded composite microspheres on injured RGS administrated on the optic nerve crush of rats with multiple doses of EPO solution. They concluded a similar neuroprotective effect between them for the new neuroregenerative disease in the retina and central nervous system [19].
Sullivan et al. obtained an optimal therapeutic dose of EPO to be effective as a neuroprectant in a mouse model of optic nerve crush injury. They found that this optimal therapeutic dose of EPO must be administered at levels higher than is approval for treatment of anemia in human [20].
Peripherally administered EPO can effectively cross the blood–brain barrier [13, 17, 21], stimulate neurognesis, neuronal differentiation, and activate brain neurothropic, antiapoptotic, and anti-oxidant and anti-inflammatory signaling; these mechanisms underlie these tissue protection effects on nervous system disorders [22, 23].
Thus, EPO could potentially address many aspects of pathophysiologic cascade in TON. First, EPO has significant antiapoptotic activity on RGCs that can help maintain survival and possibly regain function following axonal damage [15, 24–26]. Second, EPO can counteract the secondary mechanism of nerve damage following TON, including antioxidant and anti-inflammatory properties thus decreasing edema and possibility incidence and/or severity of compartment syndrome. Third, EPO may promote axonal regeneration following TON [15, 26–28].
In a study that conducted by Modarres et al., they showed a beneficial effect of intravitreal injection of erythropoietin in patients with diagnosis of non-arthritic anterior ischemic optic neuropathy [10].
In our study, initial BCVA improved dramatically after 1 and 3 months of systemic EPO; the differences were statistically significant. In a pilot study by Kashkouli et al., they compared seven cases of indirect TON in eight patients who had not received any prior specific treatment, given three intravenous injections of 10,000 IU of EPO on three successive days. They found increased BCVA in all patients except one after treatment with intravenous EPO [11].
Therefore, we assumed that EPO can reduce the secondary mechanism of optic nerve damage from apoptosis while preserving RGCs and also improve the neuoregneration in the damaged axon, and ultimately improve visual function following TON.
In our study, BCVA improvement occurred in 13 of 18 cases. There was an initial visual acuity of NLP in seven cases in this series, that only two of them improved whereas, Kashkouli et al. reported that three cases with NLP in the EPO group showed improvement [11].
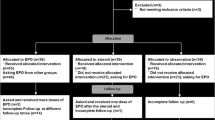
This pilot study is a preliminary report of one branch of a multicenter randomized clinical trial of different treatment modalities in TON (EPO, high dose steroid and placebo) that is going on and will be reported in the future.
References
Goldberg RA SKF, Goldberg RA (1994) Traumatic optic neuropathy 38:487–518
al-Qurainy Ia Fau - Stassen LF, Stassen Lf Fau - Dutton GN, Dutton Gn Fau - Moos KF, Moos Kf Fau - el-Attar A, el-Attar A (1991) The characteristics of midfacial fractures and the association with ocular injury: a prospective study Br J Oral Maxillofac Surg. 29:291–301
Entezari M, Rajavi Z, Sedighi N, Daftarian N, Sanagoo M (2007) High-dose intravenous methylprednisolone in recent traumatic optic neuropathy; a randomized double-masked placebo-controlled clinical trial. Graefes Arch Clin Exp Ophthalmol 245:1267–1271
Steinsapir KD, Seiff SR, Goldberg RA (2002) Traumatic optic neuropathy: where do we stand? Ophthal Plast Reconstr Surg 18:232–234
Chan JW (2007) Optic nerve disorders. Diagnosis and management. Springer, Berlin Heidelberg, pp 130–144
Steinsapir KD, Goldberg RA, Sinha S, Hovda DA (2000) Methylprednisolone exacerbates axonal loss following optic nerve trauma in rats. Restor Neurol Neurosci 17:157–163
Miller NR, Newman NJ, Biousse V (2008) Walsh and Hoyt’s clinical neuro-ophthalmology: the essentials. Lippincott and william &Wilkins. Lippincott and William &Wilkins, Philadelphia
Shepard MJ, Bracken MB (1994) The effect of methylprednisolone, naloxone, and spinal cord trauma on four liver enzymes: observations from NASCIS 2. National Acute Spinal Cord Injury Study Paraplegia 32:236–245
Falavarjani KG, Modarres M (2011) Erythropoietin; a novel neuroprotective agent for ocular disorders. Journal of ophthalmic & vision research 6:76–77
Modarres M, Falavarjani KG, Nazari H, Sanjari MS, Aghamohammadi F, Homaii M, Samiy N (2011) Intravitreal erythropoietin injection for the treatment of non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol 95:992–995
Kashkouli MB, Pakdel F, Sanjari MS, Haghighi A, Nojomi M, Homaee MH, Heirati A (2011) Erythropoietin: a novel treatment for traumatic optic neuropathy-a pilot study. Graefes Arch Clin Exp Ophthalmol 249:731–736
Thompson HS, Corbett JJ, Cox TA (1981) How to measure the relative afferent pupillary defect. Surv Ophthalmol 26:39–42
Sairanen T, Karjalainen-Lindsberg ML, Paetau A, Ijas P, Lindsberg PJ (2006) Apoptosis dominant in the periinfarct area of human ischaemic stroke–a possible target of antiapoptotic treatments. Brain: a journal of neurology 129:189–199
Fisher JW (2003) Erythropoietin: physiology and pharmacology update. Experimental biology and medicine 228:1–14, Maywood, NJ
Junk AK, Mammis A, Savitz SI, Singh M, Roth S, Malhotra S, Rosenbaum PS, Cerami A, Brines M, Rosenbaum DM (2002) Erythropoietin administration protects retinal neurons from acute ischemia-reperfusion injury. Proc Natl Acad Sci U S A 99:10659–10664
Ehrenreich H, Fischer B, Norra C, Schellenberger F, Stender N, Stiefel M, Sirén AL, Paulus W, Nave KA, Gold R, Bartels C (2007) Exploring recombinant human erythropoietin in chronic progressive multiple sclerosis. Brain 130:2577–88
Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewczuk P, Stiefel M, Rustenbeck HH, Breiter N, Jacob S, Knerlich F, Bohn M, Poser W, Ruther E, Kochen M, Gefeller O, Gleiter C, Wessel TC, De Ryck M, Itri L, Prange H, Cerami A, Brines M, Siren A, Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewczuk P, Stiefel M, Rustenbeck HH, Breiter N, Jacob S, Knerlich F, Bohn M, Poser W, Ruther E, Kochen M, Gefeller O, Gleiter C, Wessel TC, De Ryck M, Itri L, Prange H, Cerami A, Brines M, Siren AL (2002) Erythropoietin therapy for acute stroke is both safe and beneficial. Mol Med 8:495–505, Cambridge, Mass
Tan H, Zhong Y, Shen X, Cheng Y, Jiao Q, Deng L (2012) Erythropoietin promotes axonal regeneration after optic nerve crush in vivo by inhibition of RhoA/ROCK signaling pathway. Neuropharmacology 63:1182–1190
Rong X, Mo X, Ren T, Yang S, Yuan W, Dong J, Wang Y, Wang X (2011) Neuroprotective effect of erythropoietin-loaded composite microspheres on retinal ganglion cells in rats. European journal of pharmaceutical sciences : official journal of the European Federation for Pharmaceutical Sciences 43:334–342
Sullivan TA, Geisert EE, Templeton JP, Rex TS (2012) Dose-dependent treatment of optic nerve crush by exogenous systemic mutant erythropoietin. Exp Eye Res 96:36–41
Siren AL, Fasshauer T, Bartels C, Ehrenreich H (2009) Therapeutic potential of erythropoietin and its structural or functional variants in the nervous system. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics 6:108–127
Gorio A, Gokmen N, Erbayraktar S, Yilmaz O, Madaschi L, Cichetti C, Di Giulio AM, Vardar E, Cerami A, Brines M (2002) Recombinant human erythropoietin counteracts secondary injury and markedly enhances neurological recovery from experimental spinal cord trauma. Proc Natl Acad Sci U S A 99:9450–9455
King CE, Rodger J, Bartlett C, Esmaili T, Dunlop SA, Beazley LD (2007) Erythropoietin is both neuroprotective and neuroregenerative following optic nerve transection. Exp Neurol 205:48–55
Bartels C, Spate K, Krampe H, Ehrenreich H (2008) Recombinant human erythropoietin: novel strategies for neuroprotective/neuro-regenerative treatment of multiple sclerosis. Ther Adv Neurol Disord 1:193–206
Weishaupt JH, Rohde G, Polking E, Siren AL, Ehrenreich H, Bahr M (2004) Effect of erythropoietin axotomy-induced apoptosis in rat retinal ganglion cells. Invest Ophthalmol Vis Sci 45:1514–1522
Kurimoto T, Miyoshi T, Suzuki A, Yakura T, Watanabe M, Mimura O, Fukuda Y (2003) Apoptotic death of beta cells after optic nerve transection in adult cats. The Journal of neuroscience : the official journal of the Society for Neuroscience 23:4023–4028
Feng Q (2006) Beyond erythropoiesis: the anti-inflammatory effects of erythropoietin. Cardiovasc Res 71:615–617
Katavetin P, Tungsanga K, Eiam-Ong S, Nangaku M (2007) Antioxidative effects of erythropoietin. Kidney international Supplement: S10-15
Conflict of interest
None of the authors has any financial/conflicting interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Entezari, M., Esmaeili, M. & Yaseri, M. A pilot study of the effect of intravenous erythropoetin on improvement of visual function in patients with recent indirect traumatic optic neuropathy. Graefes Arch Clin Exp Ophthalmol 252, 1309–1313 (2014). https://doi.org/10.1007/s00417-014-2691-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2691-6