Abstract
Background
The pathogenesis of proliferative diabetic retinopathy (PDR) remains poorly understood. Recent studies have implicated that monocyte chemoattractant protein-1 (MCP-1) is associated with diabetic microvascular or macrovascular complications. However, the relationship between single nucleotide polymorphism(SNP)c.2518A/G -rs1024611 in the MCP-1 gene with diabetic retinopathy remains controversial. In the present study, we evaluated the association of SNP in the MCP-1 gene with diabetic retinopathy (DR) and diabetic macular edema (DME) in a Chinese population from Northern China with type 2 diabetes.
Methods
We conducted a case–control study, which enrolled 1,043 subjects with type 2 diabetes (528 with DR, including 277PDR; 515 without DR), and SNP genotyping of c.2518A/G in the MCP-1 gene was performed using the polymerase chain reaction. Genomic DNA was isolated from 3 ml samples of whole blood using a modified conventional DNA extraction method. The genotype and allele frequencies of 2518A/G were studied by using an automated DNA sequencer (ABI PRISM 3730 DNA Sequencer).
Results
The demographic and clinical characteristics did not differ among genotype subgroups. The MCP-1(−2518) GG genotype was significantly associated with DR susceptibility with OR of 1.481 (95 % CI, 1.019-2.153) (P = 0.046). There were no significant differences in the MCP-1(−2518) G allele frequencies in DR compared to non-diabetic retinopathy (DNR) (P > 0.05, OR = 0.841, 95 % CI, 0.705–1.002). The MCP-1(−2518) GG genotype was significantly associated with high-risk PDR susceptibility with OR of 2.656 (95 % CI, 1.222–5.775) (P = 0.014). The MCP-1(−2518) G allele was significantly increased in high-risk PDR patients (P = 0.020, OR = 1.481, 95 % CI, 1.070–2.051) compared with A allele. Genotype and allele frequencies of various DME of the DR patients were compared, but there were no significant associations established (P > 0.05).
Conclusions
It is likely that the MCP-1 c.2518G/G genotype is a susceptibility gene for DR in Chinese type 2 diabetic patients, especially the high-risk PDR. There is no association with DME and c.2518G/G .
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy (DR) remains the leading cause of blindness among working-age individuals in developed countries [1, 2]. Visual loss develops primarily from either increased DME or proliferation of new retinal vessels [3]. Although the pathogenesis of DR has not been fully elucidated, inflammation may play an important role in DR and several cytokines and chemokines have been suggested in the etiology of DR.
Recently, a potent cytokine, monocyte chemoattractant protein-1 (MCP-1), was shown to have the ability to activate monocytes, macrophages, and lymphocytes [4]. Activation of it has been demonstrated for hyperglycemia accelerates MCP-1 production in vascular endothelial cells and retinal pigmented epithelial cells [5]. Moreover, the levels of MCP-1 in aqueous and vitreous conditions were significantly increased in patients with diabetic retinopathy [6–8]. MCP-1 production may lead to neovascularization and permeability of retinal vessels, which is the cause of proliferative diabetic retinopaty (PDR) and DME.
MCP-1 gene located at positions −2518 (G or A) has been reported to affect MCP-1 transcription activity [9], and this polymorphism has been associated with type 2 diabetes, insulin resistance [10], type 1 diabetes [11], and cardiovascular disease [12]. The association between polymorphism of MCP-1 (ID: 6347) c.2518A/G – rs1024611 and DR had been reported in Japan and Korea [13, 14], but their opinion was inconsistent. However, there is no report in China so far. This study was designed to clarify the relationship of polymorphism of MCP-1 c.2518A/G with type 2 diabetes with or without DR. The relationship between MCP-1 c.2518A/G and a different stage of DR has also been studied.
Materials and methods
Sample collection
A total of 1043 type 2 diabetic patients (with and without retinopathy) were recruited for this study, all patients belonged to the same ethnic group, and they were unrelated Han Chinese. This study was approved by Harbin Medical University Institutional review Board. All patients provided written informed consent for participation in the study and donation of samples. Inclusion criteria were age at diagnosis of diabetes ≥30 years and a known duration of diabetes of ≥5 years. Diabetes was diagnosed according to WHO criteria. All patients underwent biochemical tests and medical history. Diabetic retinopathy was assessed through dilated pupils by trained ophthalmologists. All the patients underwent a complete eye examination, which included a dilated retinal examination and a fundus color photogram. Patients with pathological changes of retina were examined by fundus fluorescein angiography (FFA). FFA was graded for DR severity in a masked fashion by ophthalmologists at the Ophthalmology Department in the First Affiliated Hospital of Harbin Medical University. The modified Early Treatment of Diabetic Retinopathy Study Airlie House classification of DR was used to grade the retinopathy into the following categories: mild nonproliferative diabetic retinopathy (NPDR), moderate NPDR, Severe NPDR and proliferative diabetic retinopathy (PDR) (including high-risk PDR). High-risk PDR: New vessels within 1 disc diameter of the optic nerve head that are larger than 1/3 disc area; vitreous or preretinal hemorrhage associated with less extensive neovascularization of the optic disk (NVD) or with neovascularization elsewhere (NVE) 1/2 disc area or more in size [15]. All the patients with DR were checked for foveal thickness of macula by optical coherence tomography (OCT), according to the thickness of the macular centre divided into three parts (Mild ≤ 250 um; 250 um < Moderate < 350 um; Severe ≥350um). The severity of DR or DME between the two eyes of the same patient was compared, excluding one left eye because of atrophy of the eyeball. Macular thickness was checked by using OCT, and patients with previous laser treatment, eyeball atrophy, epimacular membrane, age-related macular degeneration (ARMD), previous intravitreal injection medicine and vitreous hemorrhage were excluded.
Genotyping
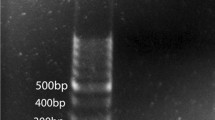
Peripheral leukocytes were isolated from EDTA-treated whole blood obtained from each patient, and genomic DNA was extracted with QIAamp DNA Mini Blood Kit (Qiagen, Hilden, Germany) for polymerase chain reaction (PCR) amplification of MCP-1. DNA samples were collected in a 1.5 ml Eppendorf tubes and stored at −20 °C until use.
This SNP was detected by using an automated DNA sequencer (ABI PRISM 3730 DNA Sequencer). PCR was used to amplify the primer. In the MCP-1(−2518A/G), the forward primer 5′CTGTGGCATGACCACTTGTT 3′ and reverse primer 5′ACTTCT CTCACGCCAGCACT 3′ were used to amplify in a final PCR mixture of 20 μl containing 100 ng of genomic DNA and 12.5 pmol of each primer. The DNA was then subjected to initial denaturation at 95 °C for 2 min, followed by annealing 57 °C for 30 s and elongation at 72 °C for 40 s. After 30 cycles, the reaction was extended for an additional 5 min at 72 °C.
Statistical analysis
All statistical tests were performed with SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Age, sex, blood pressure, duration of diabetes, body mass index, glycosylated hemoglobin, smoking and alcohol use were compared between the study groups (DR and non-DR) using the two-tailed Student t test. The genotype phenotype association was done using a χ2 test, and to test for deviation of genotype distribution from the Hardy-Weinberg equilibrium using Haploview (version 3.32). The odds ratio (OR) and the 95 % confidence interval (95 % CI) were calculated, and p values were evaluated using the same method. The level of statistical significance was set at p < 0.05.
Results
Among the 1,043 recruited type 2 diabetic patients, 515 patients were DNR, and 528 with DR. Among the DR patients, we graded DR and DME according to the right eyes. There were 76 Mild NPDR patients, 79 Moderate NPDR patients, 96 Severe NPDR patients and 277 PDR patients (including 169 high-risk PDR).
The demographics of the study population are summarized in Table 1. There was no significant difference in age, sex, smoking, alcohol use, blood urea, blood pressure, glycemic, and nutritional status among the two study groups.
Three genotypes (AA, AG and GG) of MCP-1-2518 A/G polymorphisms were found in Han people in Helongjiang Province. Genotype and allele frequencies are shown in Table 2. The MCP-1(−2518) GG genotype was significantly associated with DR; the odds ratio (OR) for the G/G genotype of MCP-1(−2518) to DR was 1.481 (95 % CI, 1.019–2.153, P < 0.05) (Table 2), while the association of A/G genotype and DR was not so significant with DR with OR of 1.326 (95 % CI, 0.926–1.899, P > 0.05). The MCP-1(−2518) G allele was not related with DR compared with A allele (P > 0.05, OR = 0.841, 95 % CI, 0.705–1.002).
Genotype and allele distribution of MCP-1 gene polymorphisms in different stages of type 2 diabetic patients with retinopathy were also analyzed (Table 3). The MCP-1(−2518) GG genotype was significantly associated with high-risk PDR susceptibility with OR of 2.656 (95 % CI, 1.222–5.775, P = 0.014). While the A/G genotype was not associated with DR susceptibility with OR of 1.993 (95 % CI, 0.926–4.290, P > 0.05). The MCP-1(−2518) G allele was significantly increased in high-risk PDR patients (OR = 1.481, 95 % CI, 0.070–2.051 P < 0.05) compared with the A allele. Genotype and allele frequencies of various DME of the DR patients were compared. No significant associations have been found (P > 0.05) (Table 4).
There was no significant difference (P > 0.05) in the severity of DR or DME between the two eyes of the same patient (Tables 5 and 6). In the multiple logistic regression model, HbA1c was significantly associated with DR after adjustment for conventional risk factors (OR = 1.21, 95% CI, 1.06–1.37, P = 0.025) (Table 7).
Discussion
The present study investigated the association of the MCP-1 c.2518 polymorphism with DR and DNR in a northern Chinese Han population. We found that the MCP-1 c.2518G/G genotype was associated with the increased risk of DR. When comparing NPDR with PDR, severe NPDR and non-high-risk PDR were excluded in order to clarify the relationship between mild and severe DR. The results showed that the G allele was associated with increased risk of high-risk PDR. All DR patients were checked with FFA, so that the diagnose of DR could be accurate and reliable. There was no association between the MCP-1 c.2518 polymorphism and DME.
MCP-1 is widely known as a pro-inflammatory cytokine due to its chemotactic activity. It has been implicated that the pathogenesis of many diseases are characterized by monocytic infiltration, such as psoriasis, rheumatoid arthritis and atherosclerosis. Elevated MCP-1 serum levels have been reported in many diseases including coronary artery disease (CAD), hepatitis, obesity, acute myeloid leukemia and autoimmune diseases (such as rheumatoid arthritis, chronic autoimmune thyroiditis) [16–21]. Recently, it was demonstrated that chemokines play a pivotal role in mediating angiogenesis and fibrosis [22–24]. More important, MCP-1 has been shown to play a possible role as a modulator of PDR due to its ability to regulate arterial smooth muscle cell proliferation and induce retinal neovascularization [25–27]. It has been reported that MCP-1-induced angiogenesis was as potent as that induced by vascular endothelial growth factor (VEGF) in vivo [28, 29], which is implicated strongly in the development of retinal and iris neovascularization in PDR [30]. However, there is no report so far about the relationship of MCP-1 and DME.
A polymorphism at position −2518 in the 5′-flanking region of the MCP-1 gene was identified and the G allele of this polymorphism was associated with increased MCP-1 expression [31, 32]. Katakami, et al. [13] reported that the G allele in the 2518A/G polymorphism was a susceptibility allele for diabetic retinopathy in a Japanese population of diabetic patients. Hyun Jeong, et al. [14] reported that the 2518A/A genotype in MCP-1 could be used as a susceptibility gene to predispose Koreans exhibiting type 2 diabetes for the development of PDR. Their conclusions were not consistent. Our conclusion was similar with Katakami’s but different from Hyun Jeong’s. We found that MCP-1 c.2518G/G was a susceptibility gene to predict DR, especially high-risk PDR in type 2 diabetes patients in the northern Han population of China. G allele in the 2518A/G polymorphism was associatied with the severity of DR . There was no significant relation for G allele and DR, and further study is necessary. There are several reasons for the difference of our findings compared with previous reports: First, ethnic differences might play a role. Gene SNPs have a different influence in type 2 diabetes for ethnic variation. Palmer proved several candidate loci have been identified, which are nominally associated with insulin resistance in Hispanic Americans. So we speculate ethnic variation may play an important role in DR [33]. Second, there were different sample sizes (there were 3,802 subjects in the Japanese paper, 590 in the Korean paper, and 1,043 in our paper). Different examiners can also cause bias. Laslyt and the mostly, when we compared NPDR with PDR, we used different methods from theirs. We excluded severe NPDR and non-high-risk PDR, because their disease stages were similar [34]. In order to eliminate interference with the difference of the left and right eye, the severity of DR and DME of both eyes of the same patient were compared, and there was no statistical difference (p > 0.05). Thus right eyes were selected to analyze the severity of DR and DME.
Although the most severe vision loss is a consequence of tractional retinal detachment,vitreous hemorrhage or neovascular glaucoma, the major cause of moderate vision loss is DME, which is a complication of DR that can occur at any stage of the disease [35]. For the first time, we showed that there was no association between the MCP-1-(2518) polymorphism and the severity of DME (p > 0.05). In this study, we excluded eyes after laser treatment, atrophy of eyeball, epimacular membrane, ARMD, intravitreal injection medicine and vitreous hemorrhage, as these conditions could either cause macula thickness change or affect the measurement.
Our study also indicates that the MCP-1 c.2518G/G genotype may increase the risk to the development of proliferative diabetic retinopathy in patients with long-standing diabetes. The MCP-1 c.2518G/G genotype was related to neovascularization, but not to the blood vessel leakaging. We do not know the underlying mechanisms. The patients enrolled in this study were recruited from north Chinese Han individuals, and the results presented here need to be confirmed by using different ethnic populations, larger groups and other related genes. A long-term follow-up study would be necessary to confirm the association between this polymorphism and DR. We expect to learn of more reports about the MCP-1 A-2518G polymorphism from other countries, which can help to prevent and cure DR patients.
In conclusion, it is likely that the MCP-1 c.2518G/G genotype is a susceptibility for DR in Chinese type 2 diabetic patients, and it is related to the high-risk PDR as well, but it has no association with DME.
References
Congdon NG, Friedman DS, Lietman T (2003) Important causes of visual impairment in the world today. JAMA 290:2057–2060
Lightman S, Towler HM (2003) Diabetic retinopathy. Clin Cornerstone 5:12–21
Paine SK, Basu A, Mondal LK, Sen A, Choudhuri S, Chowdhury IH, Saha A, Bhadhuri G, Mukherjee A, Bhattacharya B (2012) Association of vascular endothelial growth factor, transforming growth factor beta, and interferon gamma gene polymorphisms with proliferative diabetic retinopathy in patients with type 2 diabetes. Mol Vis 18:2749–2757
Mukaida N, Harada A, Matsushima K (1998) Interleukin-8 (IL-8) and monocyte chemotactic and activating factor (MCAF/MCP-1), chemokines essentially involved in inflammatory and immune reactions. Cytokine Growth Factor Rev 9:9–23
Bian ZM, Elner VM, Yoshida A, Kunkel SL, Elner SG (2001) Elner, Signaling pathways for glycated human serum albumininduced IL-8 and MCP-1 secretion in human RPE cells. Invest Ophthalmol Vis Sci 42:1660–1668
Abu el-Asrar AM, Van Damme J, Put W, Veckeneer M, Dralands L, Billiau A, Missotten L (1997) Monocyte chemotactic protein-1 in proliferative vitretinal disorders. Am J Ophthalmol 123:599–606
Capeans C, De Rojas MV, Lojo S, Salorio MS (1998) C–C chemokines in the vitreous of patients with proliferative vitretinopathy and proliferative diabetic retinopathy. Retina 18:546–550
Tashimo A, Mitamura Y, Nagai S, Nakamura Y, Ohtsuka K, Mizue Y, Nishihira J (2004) Aqueous levels of macrophage migration inhibitory factor and monocyte chemotactic protein-1 in patients with diabetic retinopathy. Diabet Med 1292–1297
Rovin BH, Lu L, Saxena R (1999) A novel polymorphism in the MCP-1 gene regulatory region that influences MCP-1 expression. Biochem Biophys Res Commun 259:344–348
Simeoni E, Hoffmann MM, Winkelmann BR, Ruiz J, Fleury S, Boehm BO, März W, Vassalli G (2004) Association between the A-2518G polymorphism in themonocyte chemoattractant protein-1 gene and insulin resistance and Type 2 diabetes mellitus. Diabetologia 47:1574–1580
Yang B, Houlberg K, Millward A, Demaine A (2004) Polymorphisms of chemokine and chemokine receptor genes in Type 1 diabetes mellitus and its complications. Cytokine 26:114–121
Szalai C, Duba J, Prohászka Z, Kalina A, Szabó T, Nagy B, Horváth L, Császár A (2001) Involvement of polymorphisms in the chemokine system in the susceptibility for coronary artery disease (CAD). Coincidence of elevated Lp(a) and MCP-1–2518 G/G genotype in CAD patients. Atherosclerosis 158:233–239
Katakami N, Matsuhisa M, Kaneto H, Matsuoka TA, Imamura K, Ishibashi F, Kanda T, Kawai K, Osonoi T, Kashiwagi A, Kawamori R, Shimomura I, Yamasaki Y (2010) Monocyte chemoattractant protein-1 (MCP-1) gene polymorphism as a potential risk factor for diabetic retinopathy in Japanese patients with type 2 diabetes. Diabetes Res Clin Pract 89:9–12
Jeon HJ, Choi HJ, Park BH, Lee YH, Oh T (2013) Association of monocyte chemoattractant protein-1 (MCP-1)2518A/G polymorphism with proliferative diabetic retinopathy in Korean type 2 diabetes. Yonsei Med J 54:621–625
Wilkinson CP, Ferris FL 3rd, Klein RE, Lee PP, Agardh CD, Davis M, Dills D, Kampik A, Pararajasegaram R, Verdaguer JT (2003) Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 110:1677–1682
Martinovic I, Abegunewardene N, Seul M, Vosseler M, Horstick G, Buerke M, Darius H, Lindemann S (2005) Elevated monocyte chemoattractant protein-1 serum levels in patients at risk for coronary artery disease. Circ J 69:1484–1489
Antonelli A, Ferri C, Fallahi P, Ferrari SM, Frascerra S, Franzoni F, Galetta F, Zignego AL, Ferrannini E (2009) CXCL10 and CCL2 serum levels in patients with mixed cryoglobulinaemia and hepatitis C. Dig Liver Dis 41:42–48
Antonelli A, Fallahi P, Delle Sedie A, Ferrari SM, Maccheroni M, Bombardieri S, Riente L, Ferrannini E (2009) High values of Th1 (CXCL10) and Th2 (CCL2) chemokines in patients with psoriatic arthtritis. Clin Exp Rheumatol 27:22–27
Antonelli A, Fallahi P, Delle Sedie A, Ferrari SM, Maccheroni M, Bombardieri S, Riente L, Ferrannini E (2008) High values of alpha (CXCL10) and beta (CCL2) circulating chemokines in patients with psoriatic arthritis, in presence or absence of autoimmune thyroiditis. Autoimmunity 41:537–542
Antonelli A, Ferri C, Fallahi P, Colaci M, Giuggioli D, Ferrari SM, Frascerra S, Franzoni F, Galetta F, Ferrannini E (2008) Th1 and Th2 chemokine serum levels insystemic sclerosis in the presence or absence of autoimmune thyroiditis. J Rheumatol 35:1809–1811
Kim CS, Park HS, Kawada T, Kim JH, Lim D, Hubbard NE, Kwon BS, Erickson KL, Yu R (2006) Circulating levels of MCP-1 and IL-8 are elevated in human obese subjects and associated with obesity-related parameters. Int J Obes 30:1347–1355
Salcedo R, Oppenheim JJ (2003) Role of chemokines in angiogenesis: CXCL12/SDF-1 and CXCR4 interaction, a key regulator of endothelial cell responses. Microcirculation 10:359–370
Agostini C, Gurrieri C (2006) Chemokine/cytokine cocktail in idiopathic pulmonary fibrosis. Proc Am Thorac Soc 3:357–363
Evans OVH, La SX, Fisher IB, Rajkumar V, Abraham DJ, Black CM, Denton CP (2003) Monocyte chemoattractant protein 3 as a mediator of fibrosis: overexpression in systemic sclerosis and the type 1 tight –skin mouse. Arthritis Rheum 48:1979–1991
Niu J, Kolattukudy PE (2009) Role of MCP-1 in cardiovascular disease: molecular mechanisms and clinical implications. Clin Sci 117:95–109
Kolattukudy PE, Niu J (2012) Inflammation, endoplasmic reticulum stress, autophagy, and the monocyte chemoattractant protein-1/CCR2 pathway. Circ Res 110:174–189
Deshmane SL, Kremlev S, Amini S, Sawaya BE (2009) Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res 29:313–326
Hong KH, Ryu J, Han KH (2005) Monocyte chemoattractant protein-1-induced angiogenesis is mediated by vascular endothelial growth factor-A. Blood 105:1405–1407
Salcedo R, Ponce ML, Young HA, Wasserman K, Ward JM, Kleinman HK, Oppenheim JJ, Murphy WJ (2000) Human endothelial cells express CCR2 and respond to MCP-1: direct role of MCP-1 in angiogenesis and tumor progression. Blood 96:34–40
Miller JW, Adamis AP, Aiello LP (1997) Vascular endothelial growth factor inocular neovascularization and proliferative retinopathy. Diabetes Metab Rev 13:37–50
Rovin BH, Lu L, Saxena R (1999) A novel polymorphism in the MCP-1 gene regulatory region that influences MCP-1 expression. Biochem Biophys Res Commun 259:344–348
Fenoglio C, Galimberti D, Lovati C, Guidi I, Gatti A, Fogliarino S, Tiriticco M, Mariani C, Forloni G, Pettenati C, Baron P, Conti G, Bresolin N, Scarpini E (2004) MCP-1 in Alzheimer’s disease patients: A-2518G polymorphism and serum levels. Neurobiol Aging 25:1169–1173
Palmer ND, Langefeld CD, Ziegler JT, Hsu F, Haffner SM, Fingerlin T, Norris JM, Chen YI, Rich SS, Haritunians T, Taylor KD, Bergman RN, Rotter JI, Bowden DW (2010) Candidate loci for insulin sensitivity and disposition index from a genome Wide Association Analysis of Hispanics in the IRAS family study. Diabetologia 53(2):281–289
No authors listed (1991) Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 98:766–785
Gardner TW, Antonetti DA (2008) Novel potential mechanisms for diabetic macular edema:leveraging new investigational approaches. Curr Diabet Rep 8:263–269
Acknowledgments
Li Dong, Xiao Ying lv, Bin Jie Wang carried out the experiment, data analysis and manuscript preparation. Ye Qing Wang, Hua Mu, Zhuo Lei Feng and Ping Liu were involved in the experimental design, sample collection, and grant and ethics applications. This work was supported by a grant from Heilongjiang Provincial Department of Education Science and Technology Research. (12531414)
Competing interests
None.
Patient consent
Obtained.
Ethics approval was obtained from the institute ethics committee, Harbin Medical University
Provenance and peer review
Not commissioned; externally peer reviewed
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dong, L., lv, X.Y., Wang, B.J. et al. Association of monocyte chemoattractant protein-1 (MCP-1)2518A/G polymorphism with proliferative diabetic retinopathy in northern Chinese type 2 diabetes. Graefes Arch Clin Exp Ophthalmol 252, 1921–1926 (2014). https://doi.org/10.1007/s00417-014-2651-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2651-1