Abstract
Purpose
To investigate factors influencing exudation recurrence following cataract surgery in patients already treated with anti-vascular endothelial growth factor (VEGF) agents for exudative age-related macular degeneration (AMD).
Methods
A retrospective review of medical records was performed for patients who underwent cataract surgery and had been previously treated with anti-VEGF for exudative AMD. Visual acuity was examined before surgery and 1 and 6 months after surgery. The time between diagnosis and surgery, and the exudation-free period before surgery were examined and compared between patients who had exudation recurrence and those that did not.
Results
Thirty-nine eyes of 39 patients were included in analyses. The logarithm of the minimum angle of resolution visual acuity was 1.02 ± 0.58 and had significantly improved 1 month (0.81 ± 0.62, P < 0.001) and 6 months (0.85 ± 0.64, P = 0.001) following surgery. Both the diagnosis-to-surgery period (P = 0.001) and the preoperative exudation-free period (P < 0.001) were significantly longer in patients without recurrence than in patients with recurrence.
Conclusions
Cataract surgery was beneficial in patients previously treated with anti-VEGF for exudative AMD. Our data suggests that cataract surgery should be performed after a sufficiently long exudation-free period to minimize exudation recurrence. But larger prospective studies are required to draw definitive clinical guidelines.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The recent advances in anti-vascular endothelial growth factor (VEGF) therapy have improved the chances for maintenance of, and even improvement in, visual acuity in eyes with exudative age-related macular degeneration (AMD) [1–5]. In the era of anti-VEGF agents, it has been generally accepted that uncomplicated modern cataract surgery improves visual acuity without severe adverse events in eyes treated with anti-VEGF for exudative AMD [6–8]. Overall, an improved visual acuity was maintained without an increased need for anti-VEGF intravitreal injections to keep the macula dry [6–8]. However, previous studies have mainly focused on visual outcomes and the need for additional anti-VEGF treatments. Although exudation recurrence is generally a concern of performing cataract surgery on patients with exudative AMD, factors influencing exudation recurrence have not yet been elucidated. Knowing these factors would be valuable because they could provide useful information in determining and establishing follow-up strategies following cataract surgery. This information may also be helpful in patient discussions regarding treatment policy and visual prognosis.
The purpose of the present study was to investigate factors influencing exudation recurrence following cataract surgery in patients already treated with intravitreal anti-VEGF agents for exudative AMD. Additionally, an appropriate postoperative treatment plan for patients with high risk of exudation is discussed.
Materials and methods
This retrospective, observational case series was performed at a single center, and the study conduct adhered to the tenets of the Declaration of Helsinki. The study was approved by the institutional review board (IRB No. A-2013-016). We conducted a computerized search for patients who were diagnosed with exudative AMD, treated with intravitreal anti-VEGF agents (ranibizumab or bevacizumab) prior to cataract surgery, underwent cataract surgery between July 2010 and June 2013, and were followed up for at least 6 months after surgery. Exclusion criteria included severe media opacity before cataract surgery that impeded accurate evaluation of retinal status, previous vitreoretinal surgery or photodynamic therapy, evidence of end-stage AMD (i.e., central geographic atrophy, disciform scar) evidence of intraocular inflammation, proliferative diabetic retinopathy, retinal vascular occlusion, and other vitreoretinal disorders that may have influenced visual acuity and/or macular microstructures (e.g., macular hole, thick epiretinal membrane). If both eyes of the same patient met the eligibility criteria, only one eye with prior surgery was included in the analyses.
To be included in this study, subjects were required to have had a comprehensive ophthalmologic examination, including measurement of best-corrected visual acuity (BCVA), 90-diopter lens slit-lamp biomicroscopy, fundus photography, fundus fluorescein angiography, and spectral-domain optical coherence tomography (OCT) examination (Spectral OCT/SLO®; OTI Ophthalmic Technologies Inc. Miami, FL, USA). The horizontal and vertical cross-hair OCT scans centered at the center of the fovea were performed. Indocyanine green angiography with a confocal laser-scanning system (HRA-2; Heidelberg Engineering, Dossenheim, Germany) had also been performed on some patients, at the discretion of the treating physician.
Indocyanine green (ICG) angiograms were reviewed and analyzed by two independent examiners (JHK, YSC). Exudative AMD was classified as either typical exudative AMD or polypoidal choroidal vasculopathy (PCV), based on ICG angiographic findings. Eyes with a branching vascular network and/or terminating polypoidal lesion(s) were diagnosed with PCV, with all other cases classified as typical exudative AMD. Classification disagreements between the two examiners were settled by discussion.
All patients received at least two monthly intravitreal anti-VEGF injections as an initial treatment for exudative AMD. Following resolution of intraretinal and/or subretinal fluid and normalization of macular thickness, as confirmed on OCT, follow-up examinations were performed within 1 to 4 months, at the discretion of the treating physician. The OCT examination was generally performed once every 2 to 4 months. Exudation recurrence was diagnosed when macular thickness increased, and was accompanied by macular intraretinal or subretinal fluid re-accumulation or by subretinal hemorrhage development. All the recurred cases were confirmed by OCT examination. However, cases with typical cystoid changes on OCT after cataract surgery that could indicate cystoid macular edema associated with surgery were not included in the study. Recurrent exudative AMD patients were treated with between one and three monthly intravitreal anti-VEGF injections.
Cataract surgery was performed on eyes that were exudation-free following anti-VEGF treatment. The small incision (2.8 mm to 3.0 mm) phacoemulsification and implantation of the foldable IOL was conducted by five experienced surgeons. The stop and chop technique, divide and conquer technique, and phaco chop technique were used in 30, six, and three eyes respectively. The mean duration of surgery was 14.7 ± 3.8 min (range, 10– 25 min). Hyaluronic acid (HealonTM, Advanced Medical Optics, Inc, Santa Ana, CA, USA) was used as a viscoelastic agent. Follow-up examinations were performed 1 day, 1 week, and 1 month after surgery. During all follow-up examinations, visual acuity and intraocular pressure was measured. A dilated fundus examination and OCT imaging were also usually performed 3 to 5 weeks after surgery, at the discretion of each surgeon. The BCVA measured before cataract surgery served as a baseline value, and was compared to BCVA 1 and 6 months after surgery. Snellen visual acuities were converted to the logarithm of the minimum angle of resolution (logMAR) for all analyses. Central foveal thickness (CFT) was defined as the distance between the internal limiting membrane and the retinal pigment epithelium at the fovea, and was measured manually using the calipers provided by an optical coherence tomography software program.
Patients experiencing exudation recurrence within 6 months of cataract surgery were included in the recurrence group. The remaining patients were included in the no-recurrence group. Age, sex, diagnosis, the number of anti-VEGF injections prior to surgery, the period between the exudative AMD diagnosis and surgery, and the exudation-free period before surgery were compared between the two groups. Exudative AMD subtypes (i.e., typical AMD, PCV, or unclassified) were compared only in patients with available ICG angiography results. In the no-recurrence group, BCVA was examined 1 and 6 months after surgery and compared to preoperative values. Postoperative BCVA 12 months after surgery was also collected in the recurrence group to evaluate visual outcomes after additional anti-VEGF therapy. Therefore, in the recurrence group, postoperative BCVA 1, 6, and 12 months after surgery was compared to preoperative values. The relative exudation recurrence risk was also calculated for patients with less than 24 months between exudative AMD diagnosis and surgery and a short (<12 months) exudation-free period before cataract surgery. In the recurrence group, the mean time period between follow-up examinations before and after exudative recurrence was estimated. The CFT changes in the recurrence group before surgery and when the recurrence was noted are presented.
The normality of values was tested using the Shapiro–Wilk test. The following three comparisons were performed using parametric methods; comparison of BCVA according to the follow-up period in all 39 eyes, comparison of BCVA according to the follow-up period in the recurrence group, and comparison of age between the recurrence group and the no-recurrence group. The other comparisons were performed using non-parametric methods. Value comparisons among follow-up visits were performed using repeated-measures analysis of variances or a Friedman test. Comparisons of mean values between groups were performed using an independent samples t-test/Mann–Whitney U test or chi-square test/Fisher’s exact test. Statistical analyses were performed with a commercially available software package (SPSS ver. 12.0 for Windows, SPSS Sciences, Chicago, IL, USA). Statistical significance was defined as a P value <0.05.
Results
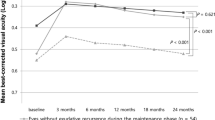
Fifty-two eyes of 52 patients underwent cataract surgery during the aforementioned period. Among them, 13 eyes were excluded from analyses. Ultimately, 39 eyes of 39 patients (21 men and 18 women) were included in analyses (Table 1). All surgeries were successfully performed without any intraoperative or postoperative complications. Mean subject age was 74.6 ± 7.6 years (range: 57–89 years). On fluorescein angiography, ten eyes (25.6 %) and 29 eyes (74.4 %) were classified as showing classic and occult-type choroidal neovascularization respectively. Indocyanine green angiography results were available in 30 of the 39 study eyes (76.9 %). Twenty eyes (51.3 %) were classified as typical exudative AMD, and ten eyes (25.6 %) were classified as PCV. Among the cases showing typical exudative AMD, two cases of retinal angiomatous proliferation were identified. Before cataract surgery, patients has received an average of 5.1 ± 2.9 intravitreal anti-VEGF injections (range: two to 15 injections), with 3.4 ± 1.3 ranibizumab injections and 1.7 ± 2.4 bevacizumab injections. Cataract surgery was performed an average of 23.0 ± 16.2 months following the exudative AMD diagnosis. The mean exudation-free period before cataract surgery was 12.1 ± 8.8 months and mean BCVA before surgery was 1.02 ± 0.58 (Snellen equivalent = 20/209). The BCVA had significantly improved 1 and 6 months after surgery, and was 0.81 ± 0.62 (20/129, P < 0.001) and 0.85 ± 0.64 (20/141, P = 0.001, Fig. 1a). Six months after cataract surgery, 15 eyes (38.5 %) had a BCVA improvement of ≥3 Snellen lines and only three eyes (7.7 %) had a BCVA loss of ≥3 lines. The remaining 21 eyes (53.8 %) had stable BCVA (Table 2).
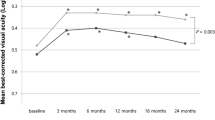
Best-corrected visual acuity (BCVA) before and after cataract surgery in all patients examined (n = 39 patients, a) and in patients with (solid line, n = 13 patients) and without (dashed line, n = 26 patients) exudative recurrence within 6 months of surgery (b). The 12-month postoperative data is only present for eyes requiring additional anti-vascular endothelial growth factor therapy after surgery
Differences between eyes in the recurrence group and eyes in the no-recurrence group are summarized in Table 1. Exudation recurrence within 6 months of cataract surgery was noted in 13 patients (33.3 %), at an average of 3.9 ± 1.4 months (range: 2–6 months) after surgery. Recurrence was noted within 3 months of surgery in six patients and between 3 and 6 months after surgery in the remaining seven patients. Nine male and four female patients were included in the recurrence group, and mean age was 75.9 ± 8.6 years. Of these 13 eyes, six had typical exudative AMD and four had PCV. Indocyanine green angiography was not performed in the remaining three patients. On average, patients in the recurrence group received 4.4 ± 2.5 intravitreal anti-VEGF injections (range: two to nine injections) before cataract surgery. Mean CFT before and after cataract surgery was measured as 178.5 ± 27.6 μm and 313.6 ± 60.8 μm respectively. Twenty-six patients (12 men, 14 women) were included in the no-recurrence group, and their mean age was 73.9 ± 7.1 years. Fourteen and six patients were diagnosed with typical exudative AMD and PCV respectively. Indocyanine green angiography was not performed in the remaining six patients. On average, patients in the no-recurrence group received 5.4 ± 3.1 intravitreal anti-VEGF injections (range: two to 15 injections) before cataract surgery. Subject age (P = 0.470), sex distribution (P = 0.173), diagnosis distribution (P = 0.523), and the number of anti-VEGF injections before surgery (P = 0.294) were not significantly different between groups. The mean time between exudative AMD diagnosis and cataract surgery was 13.3 ± 10.1 months (range: 4 to 34 months) in the recurrence group, significantly shorter than the 27.9 ± 16.6 months (9 to 64 months) in the no-recurrence group (P = 0.001). Similarly, the mean exudation-free period before surgery was 6.5 ± 5.4 months (range: 2 to 22 months) in the recurrence group, significantly shorter than the 15.2 ± 10.2 months (range: 5 to 36 months) in the no-recurrence group (P < 0.001).
Twenty-four patients had <24 months between exudative AMD diagnosis and cataract surgery, and recurrence occurred in ten (41.7 %) of these patients. Fifteen patients had ≥24 months between diagnosis and surgery, and recurrence occurred in only three (20.0 %) of these patients. Therefore, patients with <24 months between diagnosis and surgery were at 2.1 times greater risk of recurrence than patients with ≥24 months between diagnosis and surgery. Twenty-one patients had an exudation-free period of <12 months before cataract surgery, and recurrence was noted in 10 (47.6 %) of these patients. Eighteen patients had an exudation-free period ≥12 months before cataract surgery, and recurrence was noted in only three (16.7 %) of these patients. Therefore, patients with an exudation-free period of <12 months before surgery were at a 2.9 times greater risk of recurrence than patients with longer exudative-free periods. In the recurrence group, the mean period between follow-up examinations before and after the recurrence of exudation was 2.2 ± 0.6 months (range: 1–3 months).
In the no-recurrence group, mean BCVA before cataract surgery was 1.08 ± 0.61 (20/240), and had significantly improved to 0.86 ± 0.65 (20/144) and 0.86 ± 0.67 (20/144) 1 and 6 months after surgery respectively (P < 0.001, Fig. 1b). In the recurrence group, exudation after cataract surgery was treated with additional 2.0 ± 0.7 (range: one to three) intravitreal anti-VEGF injections during the 6 months following surgery. In this group, mean BCVA before cataract surgery was 0.90 ± 0.52 (20/158) and improved to 0.69 ± 0.56 (20/97), 0.77 ± 0.56 (20/117), and 0.71 ± 0.53 (20/102) 1, 6, and 12 months after surgery respectively, although the improvements were not statistically significant (Fig. 1b, P = 0.144). A representative case of exudation recurrence after cataract surgery is shown in Fig. 2.
Optical coherence tomography images obtained before (a) and 2 months (b) and 6 months (c) after cataract surgery in a patient who experienced recurrence of exudation after the surgery. The patient was diagnosed with typical exudative age-related macular degeneration, and received three monthly intravitreal anti-vascular endothelial growth factor injections before the surgery. The exudation-free period before the surgery was 3 months. The best-corrected visual acuity (BCVA) improved from 20/60 to 20/50 at 1 month after cataract surgery. The exudation recurred 2 months after the surgery, and the BCVA deteriorated to 20/60. The patient received two additional monthly intravitreal anti-vascular endothelial growth factor injections, and the BCVA improved to 20/50 at 6 months after the surgery
Discussion
Previous studies have showed the effect of cataract surgery on visual prognosis, and the need for anti-VEGF injections with encouraging outcomes. Rosenfeld and colleagues showed that an improvement of ∼10 letters on the Early Treatment Diabetic Retinopathy Study visual acuity chart was maintained 4 months after surgery [8]. The time between cataract surgery and the next anti-VEGF injection was not shorter in eyes that had undergone surgery than eyes that had not [8]. Additionally, Tabandeh and colleagues showed that 86 % of eyes that were exudation-free (not under current anti-VEGF therapy) had recurrent vessel leakage, requiring anti-VEGF therapy, following surgery [6]. However, significant visual acuity improvements (mean logMAR visual acuity improvement = 0.17) were maintained for the 14.3-month follow-up period. The number of monthly injections required to keep the macula dry before and after cataract surgery was not statistically different [6]. In agreement with this, Muzyka-Wozniak showed that a mean logMAR visual acuity improvement of 3 lines persisted for up to 14 months after cataract surgery. Additionally, the median time interval between anti-VEGF injections before and after the surgery was not different [7].
The recurrence of exudate immediately after the operation is likely to be associated with the surgery itself. However, increased activity of the exudative lesion postoperatively may also contribute to delayed recurrence after surgery. In the present study, patients were only followed for exudation recurrence within 6 months of cataract surgery, because we postulated that recurrence 6 or more months after surgery may be unrelated to the surgery and be more of a natural disease progression.
Our results also showed favorable outcomes of cataract surgery in patients previously treated with anti-VEGF for exudative AMD. However, the beneficial effect of cataract surgery was not definite in patients experiencing exudation recurrence following surgery. Approximately 1/3 of patients experienced exudation recurrence within 6 months of surgery, and visual improvements from cataract removal in these patients were not statistically significant. This result suggests that exudation recurrence influences the visual prognosis after cataract surgery. The length of the exudation-free period before surgery was found to be strongly associated with exudation recurrence after cataract surgery. Only 11.1 % of patients with at least 12 months of an exudation-free period experienced recurrence, whereas 52.4 % of patients with shorter exudation-free periods had recurrence. It is well-known that treatment delays for exudative AMD lead to poor visual prognoses [9–12], and as little as 1 month of a treatment delay may significantly influence visual outcome [11]. In the present study, postoperative BCVA in the recurrence group was not significantly different than before surgery, despite additional intravitreal anti-VEGF therapy. We postulate that retinal damage, resulting from treatment delays, is one of the possible explanations for unfavorable visual outcomes in recurrent cases. The mean period between ophthalmic examinations before and after exudation recurrence was 2.2 months, so it is possible that greater than 1 month treatment delays occurred in some cases.
In the present study, disease duration and the exudation-free period in the no-recurrence group was approximately 3 times longer than in the recurrence group. Previous studies have shown that the number of anti-VEGF injections needed to keep the macula dry decreases as the duration of exudative AMD increases [4, 13–15]. Therefore, it is possible that many of our patients with a long disease duration were in remission. The longer exudation-free phase duration may also indicate disease remission or, at least, minimal disease activity. Whether exudation recurrence was influenced by cataract surgery or it was simply the natural disease course is not known. Although cataract surgery is generally thought not to exacerbate vessel leakage [6], the possible influence of blood–retinal barrier breakdown [16, 17], and intraocular pressure fluctuations during and immediately after surgery on the retina, should not be completely neglected. We postulate that these possible effects of cataract surgery do not exacerbate exudative AMD in cases with minimal disease activity.
Our results suggest that care should be taken when planning cataract surgery in patients recently diagnosed with and/or treated for exudative AMD. If possible, cataract surgery should not be performed in patients with fewer than 12 months without treatment. Considering the large standard deviation of the exudation-free period in both the recurrence and the no-recurrence groups, we recommend waiting even longer before surgery to minimize the risk of recurrent exudation after surgery. In cases where patients are within 1 year of treatments and immediate cataract surgery is needed to accurately evaluate the macula, the higher risk of exudation recurrence should be communicated to the patient. Additionally, these patients should be monitored closely after surgery, with at least monthly follow-up examinations, and additional anti-VEGF treatments should be considered at the time of surgery or within a short-period after surgery.
In addition to its retrospective nature and small sample size, there were limitations in this study. First, OCT evaluation was not routinely performed after cataract surgery. Thus, it is possible that mild exudative recurrence, not detectable with ophthalmoscopy, may have been missed. Second, as we discussed above, it was difficult to accurately determine if fluid recurrence was influenced by cataract surgery or, rather, represented the natural history of exudative AMD. Third, the grading of cataract severity was not standardized and the ultrasound time was not recorded. Fourth, fluorescein angiography was not routinely performed to differentiate the true recurrence of exudative AMD from cystoid macular edema associated with cataract surgery. Although we believe that OCT analysis may be sufficient to verify a true recurrence of exudative AMD, the possibility that several cases with cystoid macular edema were included cannot be neglected. Lastly, two different anti-VEGF agents, ranibizumab and bevacizumab, were used for treatment. Although recent studies have shown comparable efficacy of the two agents [18, 19], it is possible that lumping patients together, regardless of anti-VEGF therapy agent, influenced our results.
In conclusion, cataract surgery was found to be beneficial in patients previously treated with intravitreal anti-VEGF injections for exudative AMD. However, the effect of the surgery on visual outcome was limited in patients with exudation recurrence following surgery. Shorter periods between exudative AMD diagnosis and cataract surgery, as well as shorter exudation-free periods before surgery were found to be risk factors for exudation recurrence after surgery. These results suggest that frequent follow-up and/or preventive anti-VEGF injections after cataract surgery may be needed in high-risk cases. Further studies with larger study populations and longer follow-up periods will be required to confirm our findings.
References
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, Kim RY (2006) Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 355:1419–1431
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, Sy JP, Schneider S (2006) Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 355:1432–1444
Spaide RF, Laud K, Fine HF, Klancnik JM Jr, Meyerle CB, Yannuzzi LA, Sorenson J, Slakter J, Fisher YL, Cooney MJ (2006) Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina 26:383–390
Fung AE, Lalwani GA, Rosenfeld PJ, Dubovy SR, Michels S, Feuer WJ, Puliafito CA, Davis JL, Flynn HW Jr, Esquiabro M (2007) An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol 143:566–583
Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ (2011) Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 364:1897–1908
Tabandeh H, Chaudhry NA, Boyer DS, Kon-Jara VA, Flynn HW Jr (2012) Outcomes of cataract surgery in patients with neovascular age-related macular degeneration in the era of anti-vascular endothelial growth factor therapy. J Cataract Refract Surg 38:677–682
Muzyka-Wozniak M (2011) Phacoemulsification in eyes with neovascular AMD treated with anti-VEGF injections. Eur J Ophthalmol 21:766–770
Rosenfeld PJ, Shapiro H, Ehrlich JS, Wong P (2011) Cataract surgery in ranibizumab-treated patients with neovascular age-related macular degeneration from the phase 3 ANCHOR and MARINA trials. Am J Ophthalmol 152:793–798
Arias L, Armada F, Donate J, Garcia-Arumi J, Giralt J, Pazos B, Pinero A, Martinez F, Mondejar JJ, Ortega I, Zlateva G, Buggage R (2009) Delay in treating age-related macular degeneration in Spain is associated with progressive vision loss. Eye (Lond) 23:326–333
Oliver-Fernandez A, Bakal J, Segal S, Shah GK, Dugar A, Sharma S (2005) Progression of visual loss and time between initial assessment and treatment of wet age-related macular degeneration. Can J Ophthalmol 40:313–319
Rauch R, Weingessel B, Maca SM, Vecsei-Marlovits PV (2012) Time to first treatment: the significance of early treatment of exudative age-related macular degeneration. Retina 32:1260–1264
Muether PS, Hoerster R, Hermann MM, Kirchhof B, Fauser S (2013) Long-term effects of ranibizumab treatment delay in neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 251:453–458
Saleh M, Kheliouen M, Tebeanu E, Ballonzoli L, Bourcier T, Speeg-Schatz C, Gaucher D (2013) Retreatment by series of three intravitreal injections of ranibizumab in neovascular age-related macular degeneration: long-term outcomes. Graefes Arch Clin Exp Ophthalmol 251:1901–1907
Muniraju R, Ramu J, Sivaprasad S (2013) Three-year visual outcome and injection frequency of intravitreal ranibizumab therapy for neovascular age-related macular degeneration. Ophthalmologica 230:27–33
Lalwani GA, Rosenfeld PJ, Fung AE, Dubovy SR, Michels S, Feuer W, Davis JL, Flynn HW Jr, Esquiabro M (2009) A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol 148:43–58
Ersoy L, Caramoy A, Ristau T, Kirchhof B, Fauser S (2013) Aqueous flare is increased in patients with clinically significant cystoid macular oedema after cataract surgery. Br J Ophthalmol 97:862–865
Alio JL, Sayans JA, Chipont E (1997) Flare-cell meter measurement of inflammation after uneventful cataract surgery with intraocular lens implantation. J Cataract Refract Surg 23:935–939
Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Wordsworth S, Reeves BC (2012) Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology 119:1399–1411
Martin DF, Maguire MG, Fine SL, Ying GS, Jaffe GJ, Grunwald JE, Toth C, Redford M, Ferris FL 3rd (2012) Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 119:1388–1398
Conflict of interest
None
Meeting presentation
None
Financial support
This study is supported by Kim’s Eye Hospital Research Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, T.G., Kim, J.H., Chang, Y.S. et al. Factors influencing the exudation recurrence after cataract surgery in patients previously treated with anti-vascular endothelial growth factor for exudative age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 252, 1573–1579 (2014). https://doi.org/10.1007/s00417-014-2624-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2624-4