Abstract
Background
To investigate the effect of induced arteriolar constriction (AC) on alterations in gene expression of factors implicated in the development of edema in branch retinal vein occlusion (BRVO).
Methods
In Brown-Norway rats, BRVO was induced by laser photocoagulation of the veins in one half of the retina. AC of the afferent arterioles was performed 30 min later. We then determined the expression of Vegfa, Vegfb, Pedf, Kir4.1, Aqp4, Aqp1, Il1ß, and Il6 with real-time polymerase chain reaction (RT-PCR) in the neuroretina and retinal pigment epithelium (RPE) after 1, 3, and 7 days. Immunostaining against GFAP, aquaporin (AQP)-4, and Kir4.1 was performed on days 1 and 3.
Results
BRVO resulted in transient upregulation of Vegfa in the neuroretina on day 1. The expressions of Kir4.1, AQP4, and AQP1 were downregulated, and Il1ß and Il6 were strongly upregulated, on days 1 and 3. The retinal distribution of GFAP and AQP4 proteins remained unaltered, while the Kir4.1 protein displayed redistribution from polarized to uniform retinal distribution. AC accelerated the restoration of downregulated Kir4.1, Aqp4, and Aqp1 in the RPE, of Kir4.1 in the neuroretina, and of upregulated Il6 in the neuroretina. AC did not influence the gliotic alterations of Müller cells and the redistribution of the Kir4.1 protein.
Conclusion
Constriction of the afferent artery in the BRVO region accelerated the restoration of potassium channels and Il6. These alterations may contribute to faster resorption of retinal edema, and may decrease the level of inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of macular edema is the major cause of vision loss in patients with branch retinal vein occlusion (BRVO) [1]. Both systemic and retinal factors contribute to the development of macular edema [2]. Systemic factors cause an excess influx of fluid from the vessels into the retinal parenchyma, e.g., due to an increase in hydrostatic pressure [2]. There are two retinal factors: ischemia-hypoxia and inflammation [3, 4]. Generally, retinal edema develops via vascular leakage (vasogenic edema) and/or impairment in the fluid clearance from the retinal tissue. Cases of retinal edema without angiographic vascular leakage suggest that impaired fluid clearance is an important pathogenic factor of edema [5].
The major vessel-permeabilizing factor induced by retinal hypoxia and inflammation is vascular endothelial growth factor (VEGF)-A [6]. Various other inflammatory factors including interleukin (IL)-1ß and IL-6 were described to be implicated in the development of macular edema [7]. Pro-inflammatory factors like interleukin (IL)-1ß and IL-6 are increased in retinal venous occlusive diseases. These factors increase the permeability of retinal vessels, in part by a stimulatory effect on VEGF expression, and mediate ischemic injury in the retina [7, 8]. The expression of VEGF-A is downregulated by anti-angiogenic factors, such as pigment epithelium-derived factor (PEDF) [9, 10].
The clearance of the retinal tissue from excess fluid is suggested to be mainly mediated by an ion transport-driven water flux through retinal glial cells and the retinal pigment epithelium (RPE) [2, 5]. Müller glial cells mediate the clearance of retinal edema via a transcellular transport of potassium and water, predominantly through the inwardly rectifying potassium (Kir) channel Kir4.1 and the aquaporin-4 (AQP4) water channel [5, 11]. The ion transport through the RPE is facilitated by various channels for sodium, potassium, chloride, and bicarbonate [11]. The water flux across the RPE is facilitated by AQP1 water channels [12]. The experimental BRVO results in rapid downregulation of Kir4.1, Aqp4, and Aqp1 in the retina, a dislocation of Kir4.1 protein, and a decrease in the potassium currents of retinal glial cells [13].
Currently, intravitreal injections of steroids or anti-VEGF drugs are used to treat macular edema due to BRVO [1, 14]. Further, grid laser photocoagulation can be performed in BRVO patients without improvement of edema after intreavitreal injections [15]. Another method, which was reported to be effective in treatment of edema due to BRVO, is laser-induced arteriolar constriction (AC), also called arterial crimping [16]. Even though some studies [17–19] showed visual improvement in BRVO patients treated by AC, the mechanisms of the therapeutic action of this technique have not yet been clarified. AC is supposed to result in a decrease in the arterial pressure and to facilitate the draining of edema [16]. On the other hand, constriction of the arteriole that crosses the occluded area has been described to occur in situ in experimental BRVO [20], likely by a decrease in the production of vasodilating nitric oxide [21, 22]. The constriction, which occurs within minutes and persists for several weeks, may contribute to the development of tissue hypoxia and apoptosis in the inner retina [21].
Using a rat model of BRVO in the present study, we investigated the impact of AC on changes in retinal gene expression of factors and channels implicated in the development/resolution of retinal edema. In addition, we determined the effects of AC on the alterations in the localization of water and potassium channels that may contribute to an impairment of the fluid clearance from the edematous retinal tissue. Alterations in retinal gene expression were determined in the occluded and non-occluded parts of the neuroretina and RPE.
Materials and methods
Experimental BRVO and AC
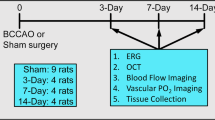
All procedures concerning animals were in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research, and were approved by the local authorities (Faculty of Medicine of the University of Leipzig and Landesdirektion Leipzig). All efforts were made to minimize the number of animals used and their suffering. Adult Brown-Norway rats (above 300 g) were used, along with the rat model of retinal vein occlusion, as previously described [13, 23]. The animals were reared in 12 h (6:00 AM −6:00 PM) light/dark cycles. The following groups were investigated: a BRVO group (32 animals) with half-retinal branch vein occlusion, and a BRVO-AC group (19 animals) with half-retinal branch vein occlusion followed by laser-induced arteriolar constriction.
Animals were anesthetized by intraperitoneal ketamine (100 mg/kg) and xylazine (5 mg/kg). In the right eye of the animals, half of the branch retinal veins near the optic nerve head were photocoagulated 15 min after i.p. injection of 0.2 ml of 10 % sodium fluorescein, using a blue-green argon laser with the aid of a 78-diopter lens (parameters, 1.0 s, 50 μm, 50–100 mW, 5–12 spots per vein). The other half of the veins remained perfused. The contralateral eyes remained untreated and served as controls. One day after laser photocoagulation, the success of BRVO was approved by indirect stereoscopic ophthalmoscopy. In the BRVO-AC group, laser-induced constriction of the afferent arterioles of the treated half of the retina was performed 30 min after BRVO. To verify the stability of BRVO, fluorescein angiography with intravenous injection of 0.2 ml of 10 % sodium fluorescein was performed shortly before the animals were sacrificed with CO2 1, 3, and 7 days after BRVO. The eyes were then enucleated; retina and RPE cells from the occluded and non-occluded half were removed and processed separately. Reflecting the fact that the major changes in the gene expression under ischemic conditions are presented during the acute stage of BRVO [13], the retinas and RPE cells of the experimental group (with AC) were evaluated at days 1 and 3.
Total RNA preparation and Real-time PCR
Total RNA and RT-PCR were performed as previously described [24]. Briefly, total RNA was prepared from neural retinas with Trizol reagent (0.5 ml; Gibco BRL), and from the RPE with the RNeasy Mini Kit (Qiagen, Hilden, Germany). The quality of the RNA was analyzed by agarose gel electrophoresis. After DNase treatment, cDNA was synthesized with 1 μg of total RNA using the RevertAid H Minus First Strand cDNA Synthesis Kit (Fermentas, St. Leon-Roth, Germany). The cDNA was diluted by the addition of 20 μl RNase-free water. Semi-quantitative, real-time PCR was performed with the Single-Color Real-Time PCR Detection System (BioRad, Munich, Germany). The PCR solution contained 1 μl cDNA, specific primer set (0.25 μM each) and 10 μl of QuantiTect SYBR Green PCR Mix (Qiagen) in a final volume of 20 μl.
Immunostaining
Isolated retinas were fixed in 4 % paraformaldehyde for 2 h. After several washing steps in buffered saline, the tissues were embedded in saline containing 3 % agarose (w/v), and 80-μm-thick slices were cut using a vibratome. The slices were incubated in 5 % normal goat serum plus 0.3 % Triton X-100 in saline for 2 h at room temperature and, subsequently, in primary antibodies overnight at 4 °C. After washing in 1 % bovine serum albumin in saline, the secondary antibodies were applied for 2 h at room temperature. The lack of unspecific staining was proven by negative controls, omitting the primary antibodies (not shown). The following antibodies were used: mouse anti-glial fibrillary acidic protein (GFAP; 1:200; GA5 clone; Sigma-Aldrich), rabbit anti-Kir4.1 (1:200; Alomone Labs), rabbit anti-rat AQP4 (1:200; Sigma), Cy3-conjugated goat anti-rabbit IgG (1:400; Dianova), and Cy2-coupled goat anti-mouse IgG (1:200; Dianova). Images were recorded with a confocal laser scanning microscope (LSM 510 META; Zeiss, Oberkochen, Germany) at single planes; excitation and emission settings were held constant for all images acquired.
Data analysis
The results of BRVO eyes from both animal groups (BRVO only and BRVO-AC) were compared with the levels of gene expression of the untreated control eyes. Further, the results of the animals from the BRVO-only group were compared with the BRVO-AC group. Data are expressed as mean ± SEM. Statistical analysis was made using Prism (Graphpad Software, San Diego, CA); significance was determined by Mann–Whitney's U test for two groups and the Kruskal-Wallis test followed by Dunn’s comparison for multiple groups.
Results
Time-dependent alterations in the retinal gene expression after BRVO
The previous studies on retinal ischemia showed that the highest levels of gene changes could be observed 24 h after the induction of the ischemia [13, 24]. Therefore, we sought to determine BRVO-induced alterations in the mRNA levels of factors implicated in neuroretina and RPE edema development/resolution after 1, 3, and 7 days of BRVO, both in the occluded and non-occluded parts of the tissues. Representative images of PCR products analyzed by agarose gel electrophoresis for Vegfa, Vegfb, Pedf, Il1ß, Il6, Kir4.1, Aqp1, and Aqp4 are shown in Fig. 1.
Representative images of PCR products analyzed by agarose gel electrophoresis. Amplicons for Vegfa, Vegfb, Pedf, Il1ß, Il6, Kir4.1, Aqp1, and Aqp4 using cDNA from retinas (R1, R2) and RPE-cells (RPE1, RPE2) of untreated rats are shown. The expression was investigated with real-time PCR. The negative controls (NTC) were done by adding double-distilled water instead of cDNA as template. Actb, ß-actin, was used as a housekeeping gene
Vegfa, Vegfb, Pedf
The induction of BRVO resulted in a biphasic regulation of Vegfa in the neuroretina (Fig. 2), with an early increase after 1 day of BRVO followed by a transient decrease after 3 days. The transient upregulation of Vegfa was observed in the occluded, but not in the non-occluded part of the neuroretina. In the RPE, no alteration in the expression level of Vegfa was observed, with the exception of a slight upregulation after 3 days of BRVO (Fig. 2). Vegfb expression remained unchanged after BRVO in the neuroretina (Fig. 2). In the RPE, the expression level of Vegfb significantly decreased after 3 and 7 days of BRVO (Fig. 2). The expression level of Pedf displayed a time-dependent increase in the neuroretina after 3 days of BRVO. In the RPE, a slight downregulation of Pedf was found after 1 day of BRVO (Fig. 2).
Effects of arteriolar constriction (AC) on the BRVO-induced alterations in the relative expression levels of Vegfa, Vegfb, and Pedf in the neural retina (left) and RPE (right). The gene expression levels were determined in the occluded and non-occluded parts of the BRVO retinas (right eyes) with real-time PCR after 1, 3, and 7 days of BRVO; they are expressed in relation to the values obtained in tissues from untreated control (left) eyes, which are displayed as levels of 1 (gray background area). Each bar represents the mean obtained in tissues from 7 to 10 animals; error bars represent S.E.M. Significant difference vs. untreated control: *P < 0.05; **P < 0.01; ***P < 0.001. Significant difference between BRVO and BRVO-AC: ++ P < 0.01. Significant difference between occluded and non-occluded parts of the BRVO retina: ○ P < 0.05; ○○ P < 0.01
Kir4.1, Aqp4, Aqp1
BRVO induced a rapid decrease in the gene expression levels of the potassium channel Kir4.1, and of the water channels AQP4 and AQP1, in both the neuroretina and RPE (Fig. 3). The downregulation of Kir4.1, Aqp4, and Aqp1 was observed in the occluded and non-occluded parts of the retina (Fig. 3). In the neuroretina, the expression of Kir4.1 returned to control levels within 7 days, while the expression of Aqp1and Aqp4 remained decreased as compared to the controls (Fig. 3). In the RPE, there was a conspicuous, transient upregulation of Kir4.1 and Aqp4 after 7 days of BRVO (Fig. 3).
Effects of arteriolar constriction (AC) on the BRVO-induced alterations in the relative expression levels of Kir4.1, Aqp4, and Aqp1 in the neural retina (left) and RPE (right). The gene expression levels were determined in the occluded and non-occluded parts of the BRVO retinas (right eyes) with real-time PCR after 1, 3, and 7 days of BRVO, and are expressed in relation to the values obtained in tissues from untreated control (left) eyes, which are displayed as levels of 1 (gray background area). Each bar represents the mean obtained in tissues from 7 to 10 animals; error bars represent S.E.M. Significant difference vs. untreated control: *P < 0.05; **P < 0.01; ***P < 0.001. Significant difference between BRVO and BRVO-AC: + P < 0.05; ++ P < 0.01. Significant difference between occluded and non-occluded parts of the BRVO retina: ○ P < 0.05
Il1ß, Il6
Experimental BRVO was associated with increases in the relative expression levels of Il1ß and Il6 in the neuroretina (Fig. 4). Within 1 day of BRVO, the expression of Il1ß and Il6 increased to levels 40- and 80-times higher than controls, respectively. In the RPE, Il6 was upregulated immediately after the induction of BRVO, and both Il1ß and Il6 were significantly downregulated after 7 days of BRVO (Fig. 4).
Effects of arteriolar constriction (AC) on the BRVO-induced alterations in the relative expression levels of Il1ß and Il6 in the neural retina (left) and RPE (right). The gene expression levels were determined in the occluded and non-occluded parts of the BRVO retinas (right eyes) with real-time PCR after 1, 3, and 7 days of BRVO, and are expressed in relation to the values obtained in tissues from untreated control (left) eyes, which are displayed as levels of 1 (gray background area). Each bar represents the mean obtained in tissues from 7 to 10 animals; error bars represent S.E.M. Significant difference vs. untreated control: *P < 0.05; **P < 0.01; ***P < 0.001. Significant difference between BRVO and BRVO-AC: + P < 0.05
Effect of AC on BRVO-induced alterations in retinal gene expression
AC, carried out 30 min after BRVO, prevented the downregulation of Vegfb (Fig. 2), and accelerated the restoration of downregulated Kir4.1, Aqp4, and Aqp1 in the RPE, and of Kir4.1 in the neuroretina, after 3 days of BRVO (Fig. 3). In addition, AC was associated with a faster decrease in the upregulated level of Il6 in the neuroretina after 3 days of BRVO (Fig. 4).
GFAP immunoreactivity
Retinal gliosis is characterized by an increase in the immunoreactivity of GFAP in Müller cells [25]. However, as described recently [13], BRVO is not accompanied by a broad increase in GFAP in Müller cells. This fact was confirmed in the present study. In control retinal slices, GFAP immunoreactivity was localized to astrocytes in the nerve fiber layer (Fig. 5). In retinal slices obtained 3 days after BRVO, the distribution of GFAP immunoreactivity remained largely unaltered, with the exception of some vessels, which traverse the inner plexiform layer, and which were surrounded by GFAP-expressing cell structures (Fig. 5). This pattern of GFAP distribution was observed in slices of BRVO and BRVO-AC retinas, both in the occluded (Fig. 5) and non-occluded (not shown) areas of the retinas, and also in retinal slices obtained after 1 day of BRVO (not shown).
Immunolocalization of the glial intermediate filament GFAP (green) and the glial water channel AQP4 (red) in slices of a control retina and of retinas obtained after 3 days of BRVO and BRVO-AC, respectively. Double labeling yielded a yellow staining. The BRVO tissues were obtained from the occluded parts of the retinas. Cell nuclei were labeled with Hoechst 33258 (blue). Arrowheads, blood vessels. Asterisks, cystoid spaces. GCL, ganglion cell layer; INL, inner nuclear layer; IPL, inner plexiform layer; NFL, nerve fiber layer; ONL, outer nuclear layer; OPL, outer plexiform layer. Bars, 20 μm
AQP4 immunoreactivity
The glial water channel AQP4 is predominantly localized to the inner retina and outer plexiform layer (Fig. 5). In addition to the perisynaptic localization in both plexiform layers, AQP4 immunoreactivity is enriched in perivascular spaces (Fig. 5). The overall retinal distribution of AQP4 labeling remained largely unaltered after BRVO and BRVO-AC, with the exception of sites of cystoid tissue degeneration that disrupted the regular structure of the inner nuclear and outer plexiform layers (asterisks in Fig. 5). Cystoid degeneration of the tissue, which reflects sites of retinal edema, was found in many but not all slices of BRVO and BRVO-AC retinas.
Kir4.1 immunoreactivity
Kir4.1 is the major potassium channel of Müller cells [26]. It has been shown that experimental BRVO leads to a redistribution of the Kir4.1 protein in the retinal tissue within 3 days [13]. This fact was confirmed in the present study. In control retinal tissues, immunoreactive Kir4.1 protein displayed a polarized distribution with prominent localization in the innermost retinal layers (nerve fiber and ganglion cell layers) and around the blood vessels, whereas the staining of the remaining tissue was faint (Fig. 6). This polarized distribution was lost within 3 days of BRVO, and the Kir4.1 immunoreactivity displayed a rather uniform distribution within the retinal tissue (Fig. 6). A similar redistribution of Kir4.1 immunolabeling was observed in BRVO retinas treated with AC (Fig. 6). The redistribution of the Kir4.1 protein was a time-dependent process; the disappearance of perivascular Kir4.1 occurred between 1 and 3 days of BRVO (Fig. 6). Apparently, the redistribution of the Kir4.1 protein proceeded from the innermost to the more outer parts of the retina. In contrast to the occluded parts of the BRVO retinas, a distinct degree of perivascular Kir4.1 staining remained apparent for up to 3 days in the non-occluded parts of BRVO retinas, both in AC-treated and non-treated tissues (Fig. 6).
Immunolocalization of the glial potassium channel Kir4.1 (red) in slices of a control retina and of retinas obtained after 1 and 3 days, respectively, of BRVO and BRVO-AC. The BRVO tissues were obtained from the occluded and non-occluded parts of the retinas. Cell nuclei were labeled with Hoechst 33258 (blue). In the control tissue, the Kir4.1 protein is concentrated in the innermost retinal layer and around the blood vessels (arrowheads). This polarized localization was lost within 3 days of BRVO. In the tissues from the non-occluded parts of the retina, some perivascular staining remained apparent up to 3 days of BRVO (arrowheads). GCL, ganglion cell layer; INL, inner nuclear layer; IPL, inner plexiform layer; ONL, outer nuclear layer; OPL, outer plexiform layer. Bars, 20 μm
Discussion
In a rat model of BRVO, we investigated the effects of AC on the alterations in the gene expression of factors implicated in the development and resolution of retinal edema. We found that BRVO-induced alterations in gene expression were rather complex, and differed depending on the tissue investigated (neuroretina and RPE), and on the duration of BRVO-induced retinal ischemia. Distinct alterations in gene expression were restricted to the occluded part of the neuroretina (e.g., the upregulation of Vegfa after 1 day of BRVO; Fig. 2) whereas other alterations were observed in both the occluded and non-occluded parts of the neuroretina (e.g., the downregulation of Kir4.1, Aqp4, and Aqp1; Fig. 3). Other alterations were found only in the neuroretina (e.g., the upregulation of Il1ß; Fig. 4) or RPE (e.g., the downregulation of Vegfb; Fig. 2).
There are some conspicuous alterations in the retinal gene expression in response to BRVO, including: (1) a biphasic regulation of Vegfa in the occluded part of the neuroretina, with upregulation after 1 day and downregulation after 3 days of BRVO (Fig. 2); (2) a time-dependent upregulation of Pedf in the neuroretina (Fig. 2); (3) a transient downregulation of the potassium and water channels Kir4.1, Aqp4, and Aqp1 in the neuroretina and RPE (Fig. 3); and (4) strong, time-dependent upregulation of Il1ß and Il6 in the neuroretina (Fig. 4). The rapid upregulation of Vegfa in the occluded retina (Fig. 2) suggests that BRVO results in tissue hypoxia selectively in the neuroretina of the treated half of the retinal tissue. Thus, the alterations in retinal gene expression observed in the RPE and in the non-occluded part of the retina are likely a response to the laser-induced hypoxia within the occluded part of the neuroretina.
Gene expression alterations in both the occluded and non-occluded retinal areas of eyes with BRVO may underlie the Müller cell gliosis observed in both parts of the retina. With respect to AQP4, we found a downregulation of Aqp4 (Fig. 3) but no apparent dislocation of the AQP4 protein in the retina (Fig. 5). Similar results (dislocation of Kir4.1 protein but not of AQP4 protein) were previously described in a rat model of high intraocular pressure-induced retinal ischemia-reperfusion [27]. In our previous experiments, we described that BRVO is associated with Müller cell swelling under hypoosmotic stress, which is not observed in Müller cells from control tissues, [13] suggesting that BRVO induces a disturbance of the osmotically-induced, transglial water flux. The downregulation of Kir4.1 and aquaporins, and the dislocation of the Kir4.1 protein may contribute to the development of tissue edema, and (via disturbance of the retinal potassium homeostasis) to neuronal degeneration.
Gene expression of Kir4.1 and aquaporin-4 and the membrane anchoring of Kir4.1 are sensitive to retinal ischemia, whereas the membrane anchoring of aquaporin-4 is insensitive to ischemia. Based on observations in knockout mice, it has been suggested that α-syntrophin (a protein of the dystrophin-associated protein complex) is implicated in the membrane anchoring of aquaporin-4 but not of Kir4.1 [28]. Similar mislocation of the Kir4.1 protein and unaltered retinal distribution of the aquaporin-4 protein were described in animal models of retinal ischemia-reperfusion, retinal detachment, and diabetic retinopathy [29, 30]. The mechanism of the ischemia-sensitive membrane anchoring of Kir4.1 remains to be determined.
We found a rapid upregulation of the proinflammatory factors VEGF-A (Fig. 2), IL-1ß, and IL-6 (Fig. 4) after induction of BRVO. Though these factors may induce a response cascade in the retina that finally results in inflammatory tissue degeneration and edema development, all of these factors were described to have also protective effects in the neural tissue, including the retina. IL-6 is a cytokine with pleiotropic functions. It is a mediating protein during inflammation processes and the maturation of B cells. The protein is primarily produced at sites of inflammation and induces a transcriptional inflammatory response through IL-6 receptor-alpha, which is associated with VEGF expression [31]. VEGF-A supports the survival of endothelial cells and retinal neurons. IL-6 is protective for retinal ganglion cells and photoreceptors [27, 32], and IL-1 promotes the glutamate uptake into Müller cells and the survival of retinal ganglion cells and photoreceptors [33]. It cannot be ruled out that the decrease in the upregulation of these factors observed after 3 and 7 days of BRVO might contribute to ischemic tissue degeneration.
The aim of the present study was to investigate the effect of laser-induced AC on BRVO-induced alterations in the retinal gene expression and the retinal localization of glial potassium and water channels. AC was first described by L’Esperance [16] in 1975. Several clinical studies [17–19] reported the resolution of macular edema and improvement of visual acuity in patients with BRVO treated with AC, but the mechanisms of the therapeutic action remain unclear. It was suggested that AC results in a decrease in the hydrostatic pressure within the arterioles and capillaries of the occluded vascular bed [16]. A decrease in the hydrostatic pressure will lower the water flux from the vessels into the tissue and, thus, may inhibit the development of vasogenic edema [2]. It has been described that an increase in hydrostatic pressure (hypertension) aggravates retinal inflammation [34]. Thus, through a decrease in hydrostatic pressure, AC might be also protective against retinal inflammation. On the other hand, constriction of the afferent artery was described to occur in experimental BRVO [20]. Some authors suggest that this constriction contributes to the development of tissue hypoxia [21, 22]. Therefore, laser-induced AC has not been generally accepted as a technique for the treatment of macular edema in patients with BRVO.
In our experiments, we found that AC did not prevent the redistribution of the Kir4.1 protein in the retina (Fig. 6). On the other hand, our results did not show any worsening of retinal ischemia after AC. Distinct effects of AC on the retinal gene expression might be protective against the development of retinal edema. The acceleration of the restoration of downregulated Kir4.1, Aqp4, and Aqp1 in the RPE (Fig. 3), and of Kir4.1 in the neuroretina (Fig. 3), may contribute to a faster resolution of retinal edema, while accelerated restoration of the upregulated level of Il6 in the neuroretina (Fig. 4) may limit retinal inflammation and, thus, the extent of vessel permeabilization. All effects of AC on the retinal gene expression were observed after 3 days, but not after 1 day of BRVO. It is concluded that AC has delayed effects on retinal gene expression and Müller cell properties. It remains to be determined whether a decrease in hydrostatic pressure is a causative factor of the AC-induced acceleration in the decrease of upregulated Il6 (Fig. 4).
References
Rehak M, Wiedemann P (2010) Retinal vein thrombosis: pathogenesis and management. J Thromb Haemost 8:1886–1894
Bringmann A, Pannicke T, Grosche J, Francke M, Wiedemann P, Skatchkov SN, Osborne NN, Reichenbach A (2006) Müller cells in the healthy and diseased retina. Prog Retin Eye Res 25:397–424
Tso MOM (1982) Pathology of cystoid macular edema. Ophthalmology 89:902–915
Marmor MF (1999) Mechanisms of fluid accumulation in retinal edema. Doc Ophthalmol 97:239–249
Bringmann A, Reichenbach A, Wiedemann P (2004) Pathomechanisms of cystoid macular edema. Ophthalmic Res 36:241–249
Aiello LP, Bursell SE, Clermont A, Duh E, Ishii H, Takagi C, Mori F, Ciulla TA, Ways K, Jirousek M, Smith LE, King GL (1997) Vascular endothelial growth factor-induced retinal permeability is mediated by protein kinase C in vivo and suppressed by an orally effective ß-isoform-selective inhibitor. Diabetes 46:1473–1480
Derevjanik NL, Vinores SA, Xiao WH, Mori K, Turon T, Hudish T, Dong S, Campochiaro PA (2002) Quantitative assessment of the integrity of the blood-retinal barrier in mice. Invest Ophthalmol Vis Sci 43:2462–2467
Bastiaans J, van Meurs JC, van Holten-Neelen C, Nijenhuis MS, Kolijn-Couwenberg MJ, van Hagen PM, Kuijpers RW, Hooijkaas H, Dik WA (2013) Factor Xa and thrombin stimulate proinflammatory and profibrotic mediator production by retinal pigment epithelial cells: a role in vitreoretinal disorders? Graefes Arch Clin Exp Ophthalmol 251:1723–1733
Zhang SX, Wang JJ, Gao G, Parke K, Ma JX (2006) Pigment epithelium-derived factor downregulates vascular endothelial growth factor (VEGF) expression and inhibits VEGF-VEGF receptor 2 binding in diabetic retinopathy. J Mol Endocrinol 37:1–12
Noma H, Funatsu H, Mimura T, Harino S, Eguchi S, Hori S (2010) Pigment epithelium-derived factor and vascular endothelial growth factor in branch retinal vein occlusion with macular edema. Graefes Arch Clin Exp Ophthalmol 248:1559–1565
Wimmers S, Karl MO, Strauss O (2007) Ion channels in the RPE. Prog Retin Eye Res 26:263–301
Stamer WD, Bok D, Hu J, Jaffe GJ, McKay BS (2003) Aquaporin-1 channels in human retinal pigment epithelium: role in transepithelial water movement. Invest Ophthalmol Vis Sci 44:2803–2808
Rehak M, Hollborn M, Iandiev I (2009) Retinal gene expression and Müller cell responses after branch retinal vein occlusion in the rat. Invest Ophthalmol Vis Sci 50:2359–2367
Ramezani A, Esfandiari H, Entezari M, Moradian S, Soheilian M, Dehsarvi B, Yaseri M (2012) Three intravitreal bevacizumab versus two intravitreal triamcinolone injections in recent-onset branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 250:1149–1160
Anon (1984) Branch vein occlusion study group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 98:271–282
L’Esperance F (1975) Ocular Photocoagulation. A Stereoscopic Atlas. St. Louis, CV Mosby, pp 215–222
Jalkh AE, Avila PM, Zakka KA, Trempe CL, Schepens CS (1984) Chronic macular edema in retinal branch vein occlusion: role of laser photocoagulation. Annals Ophthalmol 16:526–533
Rehak J, Dusek L, Sin M, Babkova B, Pracharova Z, Rehak M (2013) Long-term visual outcome after arteriolar constriction in patients with branch retinal vein occlusion. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. doi:10.5507/bp.2013.008. Epub 2013 Feb 18
Erdol H, Akyol N (2000) Arterial crimping in branch retinal vein occlusion with macular edema. Acta Ophthalmol Scand 78:456–459
Kohner EM, Dollery CT, Shakib M, Henkind P, Paterson JW, De Oliveira LN, Bulpitt CJ (1970) Experimental retinal branch vein occlusion. Am J Ophthalmol 69:778–825
Donati G, Pournaras CJ, Pizzolato GP, Tsacopoulos M (1997) Decreased nitric oxide production accounts for secondary arteriolar constriction after retinal branch vein occlusion. Invest Ophthalmol Vis Sci 38:1450–1457
Pournaras CJ, Rungger-Brändle E, Riva CE, Hardarson SH, Stefánsson E (2008) Regulation of retinal blood flow in health and disease. Prog Retin Eye Res 27:284–330
Saito Y, Park L, Skolik SA, Alfaro DV, Chaudhry NA, Barnstable CJ, Liggett PE (1997) Experimental preretinal neovascularization by laser-induced venous thrombosis in rats. Curr Eye Res 16:26–33
Rehak M, Drechsler F, Köferl P, Hollborn M, Wiedemann P, Bringmann A, Kohen L (2011) Effects of intravitreal triamcinolone acetonide on retinal gene expression in a rat model of central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 249:1175–1183
Bringmann A, Iandiev I, Pannicke T, Wurm A, Hollborn M, Wiedemann P, Osborne NN, Reichenbach A (2009) Cellular signaling and factors involved in Müller cell gliosis: neuroprotective and detrimental effects. Prog Retin Eye Res 28:423–451
Kofuji P, Ceelen P, Zahs KR, Surbeck LW, Lester HA, Newman EA (2000) Genetic inactivation of an inwardly rectifying potassium channel (Kir4.1 subunit) in mice: phenotypic impact in retina. J Neurosci 20:5733–5740
Sanchez RN, Chan CK, Garg S, Kwong JM, Wong MJ, Sadun AA, Lam TT (2003) Interleukin-6 in retinal ischemia reperfusion injury in rats. Invest Ophthalmol Vis Sci 44:4006–4011
Puwarawuttipanit W, Bragg AD, Frydenlund DS, Mylonakou MN, Nagelhus EA, Peters MF, Kotchabhakdi N, Adams ME, Froehner SC, Haug FM, Ottersen OP, Amiry-Moghaddam M (2006) Differential effect of alpha-syntrophin knockout on aquaporin-4 and Kir4.1 expression in retinal macroglial cells in mice. Neuroscience 137:165–175
Pannicke T, Iandiev I, Uckermann O, Biedermann B, Kutzera F, Wiedemann P, Wolburg H, Reichenbach A, Bringmann A (2004) A potassium channel-linked mechanism of glial cell swelling in the postischemic retina. Mol Cell Neurosci 26:493–502
Iandiev I, Uckermann O, Pannicke T, Wurm A, Tenckhoff S, Pietsch UC, Reichenbach A, Wiedemann P, Bringmann A, Uhlmann S (2006) Glial cell reactivity in a porcine model of retinal detachment. Invest Ophthalmol Vis Sci 47:2161–2171
Cohen T, Nahari D, Cerem LW, Neufeld G, Levin BZ (1996) Interleukin 6 induces the expression of vascular endothelial growth factor. J Biol Chem 271(2):736–741
Chong DY, Boehlke CS, Zheng QD, Zhang L, Han Y, Zacks DN (2008) Interleukin-6 as a photoreceptor neuroprotectant in an experimental model of retinal detachment. Invest Ophthalmol Vis Sci 49:3193–3200
Namekata K, Harada C, Guo X (2009) Interleukin-1 attenuates normal tension glaucoma-like retinal degeneration in EAAC1-deficient mice. Neurosci Lett 465:160–164
Silva KC, Pinto CC, Biswas SK, de Faria JB, de Faria JM (2007) Hypertension increases retinal inflammation in experimental diabetes: a possible mechanism for aggravation of diabetic retinopathy by hypertension. Curr Eye Res 32:533–541
Acknowledgments
This study was supported by grants from the Deutsche Forschungsgemeinschaft (KO 1547/6-1, GRK 1097/1). The authors wish to thank Ute Weinbrecht and Franziska Rickers for excellent technical assistance.
Conflict of interest
The authors declare that they have no conflict of interests to disclose. The authors have full control of all primary data and they agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Köferl, P., Hollborn, M., Rehak, J. et al. Effects of arteriolar constriction on retinal gene expression and Müller cell responses in a rat model of branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 252, 257–265 (2014). https://doi.org/10.1007/s00417-013-2532-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2532-z