Abstract
Purpose
To investigate the clinical presentation, isolated organism, treatment, and morbidity of contact lens–associated microbial keratitis needing hospitalization.
Methods
This retrospective study included all consecutive patients with contact lens–associated microbial keratitis hospitalized in the Rotterdam Eye Hospital from January 1, 2005, to December 31, 2009. All data regarding epidemiological characteristics, clinical presentation, isolated organism, and treatment were collected from medical records.
Results
There were 109 cases (108 patients) of contact lens–associated microbial keratitis hospitalized during the study period. Mean age was 33.3 ± 15.4 (SD) years. Pseudomonas aeruginosa was the most frequently isolated microorganism (68.8 %), with minor resistance to gentamicin (2.7 %) and ofloxacin (1.3 %). At time of presentation, best corrected visual acuity (BCVA) was very poor, with the largest proportion of patients (65.1 %) seeing worse than 0.05 Snellen. After intensive treatment, the visual outcome improved considerably, with the largest proportion (67.0 %) achieving a BCVA ≥ 0.7 Snellen. Low BCVA at admission was significantly associated with a worse final BCVA. A total of 22 patients (20.2 %) required corneal transplantation (three emergency cases). Larger size of stromal infiltrate was significantly associated with the need for corneal transplantation.
Conclusion
Microbial keratitis is a serious complication of contact lens wear, with approximately one out of five hospitalized cases requiring corneal transplantation. Ofloxacin, or a combination of gentamicin and cephazolin, still appear to be excellent first-choice therapies in the Netherlands, as little resistance has developed to these antibiotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microbial keratitis (MK) is the most severe and the only sight-threatening complication of contact lens (CL) wear [1]. Affected individuals can experience significant pain and discomfort and may require hospitalization with intensive treatment and even keratoplasty in severe cases. Visual outcome is frequently permanently impaired.
The estimated annual incidence of MK per 10,000 contact lens wearers, depending on lens type and wearing schedule, ranges between 1.2 (95 % CI, 1.1-1.5) for daily wear rigid gas permeable (RGP) lenses and 25.4 (95 % CI, 14.6-29.5) for extended wear of silicone hydrogel lenses [2]. The most recent estimation of incidence of MK in the Netherlands among CL-wearers dates from 1999, reporting an annualized incidence per 10,000 wearers between 1.1 (95 % CI, 0.6-1.7) for daily wear RGP lenses and 20.0 (95 % CI, 10.3-35.0) for extended wear of disposable SCL (soft contact lenses) [3].
With an estimated 1.9 million contact lens wearers in the Netherlands [4], this implies a huge burden, both medically and financially [5]. The economic consequences are compounded by the fact that CL-associated MK typically affects healthy people of working age.
Severe cases are mostly due to gram-negative bacteria [6–8]. In most cases, Pseudomonas aeruginosa appears to be the primary pathogen. Determination of the prevalence of microorganisms is essential so that the correct empiric antibiotic treatment may be initiated as soon as possible.
Whether a CL-wearer develops MK is multifactorial. Soft lens type [3,9] and especially overnight use [2,9,10] are the most important risk factors. Further, it has been hypothesized that lens wearers are more susceptible to MK than non-wearers because lenses cause cornea epithelial lesions, allowing bacteria to adhere [11,12]. In addition, induced corneal hypoxia [13], reduced corneal epithelial cell turnover, ocular surface compartmentalization and tear film stagnation due to contact lens wear are possible additional factors in the pathogenesis of MK [9].
Despite the many recent cohort studies that have evaluated MK in contact lens wearers [9,14–17], only one large study focussed primarily on hospitalized patients [7]. It is for this reason, and because a similar study has not yet been performed in the Netherlands, that we decided to conduct a retrospective study. We studied epidemiological characteristics, clinical features, microbiologically isolated organisms and their resistance to gentamicin, cephazolin, and ofloxacin, treatment, and visual outcome of patients with CL-related MK requiring hospitalization during a 5-year period. In addition, clinical characteristics possibly prognostic for a low best corrected visual acuity (BCVA) and for need of corneal transplantation were analysed.
Material and methods
Study population
We retrospectively analysed the clinical records of all patients with CL-related MK admitted to the Rotterdam Eye Hospital (REH), a tertiary ophthalmology referral center, from January 1, 2005, to December 31, 2009. These files were traced using registration ICD-9 codes (37000–37007, 37040–37059, 37090, 37120–37124, 371900, 0068), and each was manually reviewed to ascertain whether or not it involved a hospitalized CL-related MK.
Microbial keratitis was defined as a focal loss of corneal epithelium with underlying stromal infiltration, clinically diagnosed as MK and receiving antibiotic treatment for presumed MK [3,18]. REH criteria for hospital admission are MK with a central localization or MK with a peripheral localization combined with a stromal infiltrate exceeding a diameter of 3 mm in the greatest dimension of the lesion.
Patients with therapeutic, rather than refractive, contact lenses, a history of keratoplasty, presumed herpes simplex keratitis or those with comorbidity, e.g., rheumatoid arthritis or trichiasis, were excluded. A total of 109 cases (108 patients) were identified who fit the inclusion criteria.
Data collection
The data listed in Table 1 were identified for all subjects. We conducted a survey by mail and telephone (for the non-mail responders) among the patients to retrieve missing epidemiological data.
Microbiology
Corneal scrapings were obtained by ophthalmologists using a sterile cotton swab. In addition, samples were taken from the contact lens box or the contact lens itself, when available. Collected specimens were routinely inoculated on 5 % sheep blood agar, chocolate agar and, finally, the swap was placed in thioglycollate broth. Cultures were examined after overnight incubation and again after 24 hours. Sabouraud dextrose agar plate or a Page plate seeded with Escherichia coli were used when yeasts or fungi, or acanthamoeba infection, respectively, was suspected. These cultures were incubated for, respectively, six weeks and seven days. Further microbiological analyses were performed according to standard microbiological procedures. Additionally, PCR-testing was routinely carried out for herpes simplex virus, varicella-zoster virus, adenovirus and Chlamydia trachomatis.
Treatment
The primary treatment for MK patients hospitalized in the Rotterdam Eye Hospital is atropine 1 % t.i.d., plus cephazolin 5 % drops and fortified gentamicin drops hourly, day and night, for the first 48 hours. Tetracycline drops and oral doxycycline were administered in cases of significant loss of corneal stroma. The antimicrobial treatment is subject to modification, as guided by clinical response, clinical likelihood for a specific causative agent and sensitivity results based on microbial analysis. When the causative microorganism was identified and the lesion responded adequately to the antimicrobial therapy, topical steroids were introduced.
Data analysis
Categorical data were examined using chi-square analysis. All tests were two-tailed and a 5 % significance level was used. A mixed model analysis was used to determine the factors that predicted a worse final BCVA and need of corneal transplantation. Factors analysed in this study were presence of hypopyon, localisation (central or peripheral), duration of symptoms, BCVA at admission and size of stromal infiltrate.
For statistical analysis, Snellen BCVA was converted into logarithm of the minimal angle of resolution (LogMar) for the purpose of statistical analysis. In the text, means are followed by the standard deviation.
Results
Epidemiological characteristics
A total of 109 CL-related MK were admitted at the Rotterdam Eye Hospital between January 1, 2005, and December 31, 2009 (patient characteristics, Table 2). The average age of patients was 33.3 years (SD 15.4), ranging between 12 and 72 years (age distribution, Fig. 1) with a predominance of females (57.8 %). Mean CL-wearing experience was 9 years (SD 9.7), including nine inexperienced users with 6 months or less wearing experience. During the successive years of the 5-year study period, 30, 17, 20, 25 and 17 patients were hospitalized annually. Seasonal distribution peaked significantly during the summer season with 37 patients (p < 0.05, compared with 27 patients expected). This peak was still present after exclusion of 12 patients who reported visits abroad. A total of 15 patients reported wearing daily-wear CL while sleeping. Other possible risk factors that may have predisposed for the development of MK swimming while wearing CL (n = 5), recent corneal trauma (n = 6) and sauna visit (n = 1).
Microbiology
Cultures were taken from corneal scrapings (all cases), contact lenses (36.7 %) and contact lens boxes (14.7 %). Routine microbial analysis resulted in 86 positive samples (78.9 %). Causative microorganism and the origin of the samples are listed in Table 3. Mixed infections are reported in 31 cases, most frequently serratia (n = 15) and stenotrophomonas maltophilia (n = 8). Table 4 summarizes microbial isolates, the number of mixed infections (polymicrobial) and the sensitivity results for ofloxacine, gentamicin and cephazolin.
Clinical features
At time of presentation, BCVA was very poor, with the largest portion (65.1 %) worse than 0.05 Snellen. The interval between the appearance of subjective symptoms and presentation at the hospital ranged from 1 to 44 days (mean 4.6 ± SD 5.4). Excluding patients with prior treatment elsewhere, this interval ranged from 1 to 7 days (mean 2.6 ± SD 1.3). Clinical features at admission and antimicrobial therapy at time of admission are documented in Table 5. Duration of hospital stay ranged from 1 to 20 days (4.9 ± SD 3.0).
Treatment
Upon hospital admission, almost all patients (n = 106; 97.2 %) were initially treated according to REH protocol, as described in ‘Material and methods’. The three remaining patients had been previously treated with antibiotics elsewhere for several weeks prior to referral to the Rotterdam Eye Hospital, so adjusted therapy based on clinical response was started.
A total of 22 eyes (20.2 %) required corneal transplantation, consisting of 17 perforating keratoplasties, 3 deep anterior lamellar keratoplasties and 2 anterior lamellar corneal transplants. Three perforating keratoplasties were conducted in an emergency setting because of corneal perforation (all scrapings positive for Pseudomonas aeruginosa). There were 19 keratoplasties that were were scheduled because of substantial loss of visual acuity due to scarring. No cases in our study required evisceration or enucleation.
Mixed model analysis revealed that the size of stromal infiltrate was an independent predictor for need of cornea transplantation (p < 0.01, t = 4.685). Neither the presence of hypopyon, lesion localisation (central or peripheral), duration of symptoms nor BCVA at admission reached statistical significance (p > 0.05 for all comparisons).
A total of 47 patients (43.1 %) required RGP in order to achieve optimal vision, while 33 patients (30.3 %) did not require additional therapy (RGP or surgery).
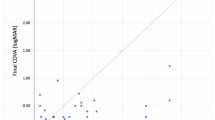
Visual outcome
The mean final visual acuity after treatment was 0.7 Snellen, ranging from 0.1 to 1.0. Figure 2 visualizes the BCVA at presentation with BCVA after treatment. After treatment, the largest proportion (67.0 %) achieved BCVA better than or equal to 0.7 Snellen. The BCVA after treatment for the 109 patients improved in all cases (mean 7.4 ± 3.5 Snellen lines) compared to BCVA at presentation. At last follow-up, only 1 patient had a BCVA of less than 0.1 Snellen.
Mixed model analysis revealed that worse BCVA at admission was an independent predictor of worse final BCVA (p < 0.01; t = 2.862). Presence of hypopyon, localisation (central of peripheral), duration of symptoms and size of stromal infiltrate did not reach statistical significance.
Discussion
This is the first report of contact lens–related MK in the Netherlands that included only hospitalized patients. Similar studies have been carried out in Belgium, Greece and Sweden [7,8,19]. However, in other countries (like the United States) ophthalmic care has become even more of an outpatient endeavour and the hospitalized cases in this study would probably be treated in an outpatient setting. By selecting only hospitalized patients, this study focuses only on the most severe cases, although on a case-by-case basis; the social factors of each patient and general health status might also have played a role in the decision whether that patient was treated on inpatient or outpatient basis.
MK was defined using a clinical case definition and not a microbiological definition because failure to culture an organism does not exclude a microbial cause. Confirmation of microbial origin by microbial analysis was found in 86 cases (78.9 %) but false-positive and false-negative cultures impose difficulties in interpretation. The percentage of positive cultures found in our study (78.9 %) is relatively high [7,8,19]. Other potential limitations of the present study are its retrospective design, overlooked cases and lack of follow-up. The Rotterdam Eye Hospital is a specialised referral hospital, so many patients had received antibiotic treatment prior to referral, which might have introduced a selection bias towards more severe and more therapy-resistant MK. However, referrals are sometimes made on a practical basis (e.g., access to hospitalization facilities) as well.
Despite innovations in contact lens material, such as silicone hydrogel lenses, the incidence of CL-related MK has not decreased in recent years, according to prospective epidemiological studies [2,20]. Predisposing factors have been studied extensively. Among others, soft lens type and overnight use are considered the major risk factors [2,3,9,10]. It has been hypothesized that the risk of corneal infection increases with soft lens type because of induced corneal hypoxia. This effect is even more pronounced when the eyes are closed, and the combination with reduced nightly tear exchange increases the risk further.
A prospective study from Morgan and colleagues [21] supports this hypothesis by showing that risk of severe MK decreased five times with the more oxygen-permeable silicone hydrogel lenses as compared with regular hydrogel lenses when worn on an extended wear basis. However, a recent prospective case–control study from Dart and colleagues [9] found no significant effect of silicone hydrogel lenses on the risk of microbial keratitis. This study concluded that factors other than corneal hypoxia play a more significant role. Other possible risk factors include lens brand [9], poor storage case hygiene [2], tobacco use [9,22], internet purchase [2], older age [9], male gender [9,21], late winter months [21], lower socioeconomic class [23], higher socioeconomic class [2] and less than 6 months of wearing experience [2].
In this study, seasonal distribution peaked in summer. The weather of the Netherlands is characterized by a maritime climate with a yearly average temperature of 10 º C. July and August are the warmest (mean temperature of 17.5 º C) and wettest months. Climatic conditions are known to affect disease severity in contact lens-related MK [24]. Severe cases are more likely to occur in warmer and humid conditions. Other possible explanations for the increased incidence are more frequent swimming during summer, unintended sleeping while wearing the contact lenses during travelling, and visits abroad to tropical regions during the holiday period. However, when excluding patients with reported visits abroad, the summer peak is still eminent.
Some isolated microorganisms are solely cultured from contact lenses or storage cases and not found in corneal isolates (Table 3). Interpretation of these results is difficult because 10 % of contact lenses harbor gram-negative and highly pathogenic species, even in asymptomatic cases [25]. Moreover, the incidence of bacterial contamination in lens cases is more than 50 % in asymptomatic subjects [25]. Thus, because of its low specificity, it may be concluded that contact lens or storage case cultures are primarily helpful in causative diagnosis when the corneal scraping is culture negative.
Several studies have shown emerging resistance to second-generation fluorquinolones, like ofloxacin, mainly among Staphylococcus species [26–27] especially in populations with high levels of antibiotic use for both human and veterinary medicine. In the current study, resistance to ofloxacin was found in only one case, in which Serratia species were determined to be the primary causative agent.
Our findings demonstrate that the use of ofloxacin, or a combination of gentamicin and cephazolin, as initial therapy, is highly effective against the majority of the cultured microorganisms. Possibly even lower resistance can be obtained by using vancomycin combined with ceftazidime or ciprofloxacin, as documented by Saeed and colleagues [6] and Fong and colleagues [28].
Our study demonstrates that relatively good visual acuity can be achieved after intensive antibiotic treatment followed by RGP use or cornea transplantation, in indicated cases. The final BCVA after treatment (mean 0.7 Snellen; range 0.1-1.0) is in accordance with previous studies that investigated contact lens-related MK needing hospital admission (Table 6). The proportion of patients undergoing keratoplasty in our study is higher (Table 6). However, different criteria for hospitalization and different length of follow-up imposes difficulties in comparing these studies adequately. The reported BCVA at last follow-up is probably an underestimation of the final BCVA because improvement after the study period is likely because some patients were referred back to their primary ophthalmologist after hospital admission (7 patients) or did not show up at their last appointment (13 patients).
Conclusion
Our study underlines that MK is a serious complication of contact lens wear, with approximately one out of five hospital admissions leading to corneal transplantation. Social and economic consequences of this pathology are significant, considering this condition often occurs in working-age people (70.4 % aged between 20 and 65 years). At time of presentation BCVA is very poor, with the BCVA of the largest proportion (65.1 %) worse than 0.05 Snellen. However, intensive treatment can considerably improve the final BCVA, with the largest proportion (67.0 %) achieving a visual acuity 0.7 Snellen or better. Ofloxacin or a combination of gentamicin and cephazolin still appear to be an excellent first choice of therapy in the Netherlands, with low levels of antimicrobial resistance.
References
Dart JK (1988) Predisposing factors in microbial keratitis: the significance of contact lens wear. Br J Ophthalmol 72:926–930
Stapleton F, Keay L, Edwards K, Naduvilath T, Dart JK, Brian G, Holden BA (2008) The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology 115:1655–1662
Cheng KH, Leung SL, Hoekman HW, Beekhuis WH, Mulder PG, Geerards AJ, Kijlstra A (1999) Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet 354:181–185
Nederlandse Associatie Contactlensleveranciers, march (2009) (Dutch Association of Contact Lens Manufacturers, report march 2009)
Smith AF, Orsborn G (2012) Estimating the annual economic burden of illness caused by contact lens-associated corneal infiltrative events in the United States. Eye Contact Lens 38:164–170
Saeed A, D'Arcy F, Stack J, Collum LM, Power W, Beatty S (2009) Risk factors, microbiological findings, and clinical outcomes in cases of microbial keratitis admitted to a tertiary referral center in ireland. Cornea 28:285–292
Verhelst D, Koppen C, Van Looveren J, Meheus A, Tassignon MJ (2006) Contact lens-related corneal ulcers requiring hospitalization: a 7-year retrospective study in Belgium. Acta Ophthalmol Scand 84:522–526
Mela EK, Giannelou IP, Koliopoulos JX, Gartaganis SP (2003) Ulcerative keratitis in contact lens wearers. Eye Contact Lens 29:207–209
Dart JK, Radford CF, Minassian D, Verma S, Stapleton F (2008) Risk factors for microbial keratitis with contemporary contact lenses: a case–control study. Ophthalmology 115:1647–1654, 1654 e1641-1643
Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, Stapleton F (2006) Microbial keratitis predisposing factors and morbidity. Ophthalmology 113:109–116
Fleiszig SM, Efron N, Pier GB (1992) Extended contact lens wear enhances Pseudomonas aeruginosa adherence to human corneal epithelium. Investig Ophthalmol Vis Sci 33:2908–2916
Cavanagh HD, Ladage P, Yamamoto K, Li SL, Petroll WM, Jester JV (2003) Effects of daily and overnight wear of hyper-oxygen transmissible rigid and silicone hydrogel lenses on bacterial binding to the corneal epithelium: 13-month clinical trials. Eye Contact Lens 29:S14–S16, discussion S26-19, S192-194
Ladage PM, Ren DH, Petroll WM, Jester JV, Bergmanson JP, Cavanagh HD (2003) Effects of eyelid closure and disposable and silicone hydrogel extended contact lens wear on rabbit corneal epithelial proliferation. Investig Ophthalmol Vis Sci 44:1843–1849
Inoue N, Toshida H, Mamada N, Kogure N, Murakami A (2007) Contact lens-induced infectious keratitis in Japan. Eye Contact Lens 33:65–69
Sharma S, Gopalakrishnan S, Aasuri MK, Garq P, Rao GN (2003) Trends in contact lens-associated microbial keratitis in Southern India. Ophthalmology 110:138–143
Moriyama AS, Hofling-Lima AL (2008) Contact lens-associated microbial keratitis. Arq Bras Oftalmol 71:32–36
Mah-Sadorra JH, Yavuz SG, Najjar DM, Laibson PR, Rapuano CJ, Cohen EJ (2005) Trends in contact lens-related corneal ulcers. Cornea 24:51–58
Poggio EC, Glynn RJ, Schein OD, Seddon JM, Shannon MJ, Scardino VA, Kenyon KR (1989) The incidence of ulcerative keratitis among users of daily-wear and extended-wear soft contact lenses. N Engl J Med 321:779–783
Nilsson SE, Montan PG (1994) The hospitalized cases of contact lens induced keratitis in Sweden and their relation to lens type and wear schedule: results of a three-year retrospective study. CLAO J 20:97–101
Morgan PB, Efron N, Hill EA, Raynor MK, Whiting MA, Tullo AB (2005) Incidence of keratitis of varying severity among contact lens wearers. Br J Ophthalmol 89:430–436
Morgan PB, Efron N, Brennan NA, Hill EA, Raynor MK, Tullo AB (2005) Risk factors for the development of corneal infiltrative events associated with contact lens wear. Invest Ophthalmol Vis Sci 46:3136–3143
Lam DS, Houang E, Fan DS, Lyon D, Seal D, Wong E (2002) Incidence and risk factors for microbial keratitis in Hong Kong: comparison with Europe and North America. Eye (Lond) 16:608–618
Stapleton F (2003) Contact lens-related microbial keratitis: what can epidemiologic studies tell us? Eye Contact Lens 29(1 Suppl):S85–S89, discussion S115-118, S192-114
Stapleton F, Keay LJ, Sanfilippo PG, Katiyar S, Edwards KP, Naduvilath T (2007) Relationship between climate, disease severity, and causative organism for contact lens-associated microbial keratitis in Australia. Am J Ophthalmol 144:690–698
Szczotka-Flynn LB, Pearlman E, Ghannoum M (2010) Microbial contamination of contact lenses, lens care solutions, and their accessories: a literature review. Eye Contact Lens 36:116–129
Alexandrakis G, Alfonso EC, Miller D (2000) Shifting trends in bacterial keratitis in south Florida and emerging resistance to fluoroquinolones. Ophthalmology 107:1497–1502
Zhang C, Liang Y, Deng S, Wang Z, Li R, Sun X (2008) Distribution of bacterial keratitis and emerging resistance to antibiotics in China from 2001 to 2004. Clin Ophthalmol 2:575–579
Fong CF, Hu FR, Tseng CH, Wang IJ, Chen WL, Hou YC (2007) Antibiotic susceptibility of bacterial isolates from bacterial keratitis cases in a university hospital in Taiwan. Am J Ophthalmol 144:682–689
Acknowledgments
The authors would like to thank Leigh Spielberg, MD, for his scientific writing and editorial assistance.
Conflict of interest: None declared
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoddenbach, J.G., Boekhoorn, S.S., Wubbels, R. et al. Clinical presentation and morbidity of contact lens–associated microbial keratitis: a retrospective study. Graefes Arch Clin Exp Ophthalmol 252, 299–306 (2014). https://doi.org/10.1007/s00417-013-2514-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2514-1