Abstract
Background
To clarify the long-term efficacy of photodynamic therapy (PDT) in patients with symptomatic polypoidal choroidal vasculopathy (PCV).
Methods
We retrospectively reviewed 60 naive eyes of 59 patients (45 men, 14 women; mean age, 73.8 years) treated with full-fluence PDT (PDT group) and followed for at least 60 months. Retreatment was either antivascular endothelial growth factor (VEGF) therapy or intravitreal triamcinolone acetonide if PDT alone was ineffective (supplemental retreatment group).
Results
The mean logarithm of the minimum angle of resolution best-corrected visual acuity (BCVA) levels at baseline and 60 months were 0.66 and 0.71, respectively. The mean change at 60 months was a decrease of 0.50 line. In the PDT group (36 eyes), the mean BCVAs at baseline and month 60 were 0.73 and 0.68, respectively (p = 0.60). In the supplemental retreatment group (24 eyes), the mean BCVAs at baseline and month 60 were 0.55 and 0.74, respectively (p = 0.076). The percentage of eyes with decreased BCVA at the time of the additional anti-VEGF treatment was significantly (p = 0.031) higher than at month 60. The risk factors identified by multiple regression analysis with a significant decrease in BCVA at month 60 were a large greatest linear dimension (GLD), classic choroidal neovascularization at baseline, and a hemorrhage over the arcade vessels after PDT.
Conclusions
The efficacy of PDT for PCV depends on the GLD. Twenty-four of the 60 eyes needed additional treatment other than only PDT during 60 months of follow-up. Additional anti-VEGF treatment may help maintain the BCVA of patients with exudative or anatomic recurrence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Polypoidal choroidal vasculopathy (PCV), first identified by Yannuzzi et al. [1] in 1990, is a distinct clinical entity characterized by a branching choroidal vascular network and polypoidal vascular dilations at the border of the network [1]. Indocyanine green angiography (ICGA) clearly shows the abnormal vascular structure, which is important for definitively diagnosing PCV [1–4]. Fluorescein angiography (FA) shows leakage from the polypoidal lesions and branching choroidal vascular network as occult choroidal neovascularization (CNV) or minimally classic CNV. ICGA often shows the branching vascular network vessels as plaques that are considered type 1 CNV [2, 3]. PCV is highly prevalent in Asian patients with age-related macular degeneration (AMD) and also develops in Caucasian patients [4–6].
Major clinical trials first reported the superior efficacy of ranibizumab (Lucentis, Genentech, Inc., South San Francisco, CA, USA) for patients with AMD [7, 8]. Although treatment with intravitreal ranibizumab (IVR) is an evidence-based therapy for AMD worldwide [9], antivascular endothelial growth factor (VEGF) therapy using bevacizumab (Avastin, Genentech, Inc.) or ranibizumab for PCV is less useful for occluding polypoidal lesions [10–12].
Photodynamic therapy (PDT) with verteporfin (Visudyne, Novartis Pharma AG, Basel, Switzerland) is effective for treating patients with PCV [13–15] and occludes most polypoidal lesions. However, few studies have reported the efficacy of PDT in patients with PCV with follow-up periods exceeding 2 years [16–19].
The purpose of the current study was to clarify the long-term efficacy and usefulness of PDT for patients with symptomatic PCV over 60 months.
Methods
We retrospectively reviewed 60 treatment-naive eyes of 59 Japanese patients (45 men, 14 women; age range, 53–88 years; mean ± standard deviation, 73.8 ± 7.7 years) with PCV treated from May 2004 to October 2006. After the potential risks and benefits were explained in detail, all patients provided written informed consent. The 24-month results for six of the 60 eyes were reported previously [15]. All patients were followed for at least 60 months at Fukushima Medical University Hospital. Twenty-five eyes of 25 patients were excluded because of follow-up periods less than 60 months. The institutional review board/ethics committee at Fukushima Medical University approved this observational study of AMD, its similar disorders at treatment and follow-up, and the retrospective comparative analysis performed in this study.
A clinical diagnosis of PCV was established based on the ICGA finding of polypoidal lesions. Patients were excluded who had undergone previous treatment, such as laser photocoagulation, submacular surgery, and transpupillary thermal therapy; and those with glaucoma, retinal pigment epithelial tears, diabetic maculopathy, retinal vascular occlusion, or idiopathic juxtafoveal retinal telangiectasis. We used the best-corrected visual acuity (BCVA) measured with a Japanese standard decimal VA chart and calculated the mean BCVA using the logarithm of the minimum angle of resolution (logMAR) scale.
All patients underwent a standardized examination including slit-lamp biomicroscopy with a contact lens, fundus color or red-free photography, FA, ICGA with a fundus camera (TRC-50 FA/IA/IMAGEnet H1024 system, Topcon, Tokyo, Japan), and/or confocal scanning laser ophthalmoscopy (Heidelberg Retina Angiograph 2, Heidelberg Engineering, Heidelberg, Germany). All optical coherence tomography (OCT) examinations were performed using time-domain OCT (OCT 3000, Carl Zeiss Meditec or OCT-Ophthalmoscope, Nidek-OTI, Gamagori, Japan) or spectral-domain OCT (3D-OCT, Topcon, Tokyo, Japan, Cirrus OCT, Carl Zeiss, or Heidelberg Spectralis OCT, Heidelberg Engineering). FA was performed to determine the lesion type, location, CNV activity, and the greatest linear dimension (GLD). ICGA was performed to determine the presence and location of polypoidal lesions and branching vascular network vessels, and the GLD.
All patients had documented visual loss at baseline. PDT with the standard dose (6 mg/m2) of verteporfin was administered according to the protocol of the Treatment of Age-Related Macular Degeneration with Photodynamic Therapy study [20]. A 689-nm laser system (Carl Zeiss, Dublin, CA, USA) delivered 50 J/cm2 of energy with an 83-s exposure time. The GLD was measured based on FA findings in all eyes. The diameter of the laser spot size was calculated by the GLD plus 1 mm in all eyes. After the initial application of PDT, follow-up examinations included evaluation of the OCT images that were performed at least every 3 months until month 60. FA and ICGA were performed every 3 months until the polypoidal lesions regressed completely. After achieving complete regression of the polypoidal lesions, FA and ICGA were performed when new exudative changes or subretinal hemorrhages were seen during a fundus examination or on OCT images. If ICGA showed the presence of polypoidal lesions, we readministered PDT. If PDT monotherapy was ineffective, i.e., patients had persistent exudation despite complete regression of the polypoidal lesions by ICGA, retreatment with an anti-VEGF drug or intravitreal triamcinolone acetonide (IVTA) was administered as we reported [21]. We administered retreatment using combined therapy of IVTA and PDT, intravitreal bevacizumab injection (IVB) monotherapy, or IVR monotherapy based on the time period (Table 1).
The PDT group included patients treated with PDT monotherapy, and the supplemental retreatment group included patients who needed supplemental retreatment except for PDT. In the supplemental retreatment group, the missing data were imputed using the last-observation-carried-forward method and compared for consistency with those obtained using observed data.
Statistical analysis was performed using the Student’s paired t-test for visual outcomes in each group. The Mann–Whitney U test or Chi-square test was used to compare outcomes between the PDT group and the supplemental retreatment group. A p value <0.05 was considered statistically significant. We used logMAR VA scores for statistical analysis.
Results
Table 2 shows the characteristics and clinical data of the 59 patients (60 eyes). All patients were observed for 60 months. The lesions were classified on FA as minimally classic CNV in eight eyes and occult with no classic CNV in 52 eyes. The mean GLD of all lesions was 4,993 μm.
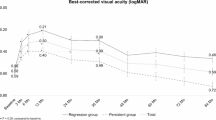
The mean logMAR BCVA levels at baseline and months 3, 6, 12, 24, 36, 48, and 60 were 0.66, 0.51, 0.47, 0.52, 0.61, 0.69, 0.59, and 0.71, respectively (Fig. 1). Significant (p < 0.001, p < 0.0001, p = 0.0097, respectively, by the paired t test) improvements in the mean BCVA were seen at months 3, 6, and 12 compared with baseline. The mean changes in the BCVA were improvements of 1.50, 1.89, 1.42, and 0.50 lines at months 3, 6, 12, and 24, and declines of 0.30, 0.19, and 0.50 lines at months 36, 48, and 60, respectively. Figure 2 shows the distribution of the mean annual BCVA changes during follow-up. Twenty (33.3 %) of the 60 eyes GA gained three lines of more of BCVA, 33 eyes (55 %) had stable VA (loss of less than 3 lines of vision), and seven (11.7 %) eyes had a decrease of three lines or more of BCVA at month 12. At 60 months, 18 (30 %) eyes had an increase of three lines or more, 23 eyes (38.3 %) had stable VA, and 19 (31.7 %) eyes had a decrease of three or more lines of BCVA (Fig. 2). Significantly (p = 0.014, Chi-square test) more eyes had decreased BCVA at month 60 compared with month 12. The mean number of PDT treatments at month 60 including combined therapy was 2.8. The polypoidal lesions did not recur in 30 (50 %) of the 60 eyes during the 60-month follow-up. In the remaining 30 (50 %) eyes, polypoidal lesions recurred a mean of 22.4 (range, 5.1-46.0) months after the initial PDT.
Graph showing the changes in the mean logarithm of the minimum angle of resolution best-corrected visual acuity (logMAR BCVA) from baseline to 60 months in all 60 eyes in the photodynamic therapy (PDT) group (36 eyes) and supplemental retreatment group (24 eyes). Significant (p < 0.001, p < 0.0001, p = 0.0097, respectively, by the paired t test) improvements in the mean BCVA are seen at months 3, 6, and 12 in all 60 eyes. In the PDT group, significant (p = 0.0024, p = 0.0022, p = 0.0064, p = 0.0064, respectively, by the paired t test) improvements in the mean BCVA are seen at months 3, 6, 12, and 24 compared with baseline. In the supplemental retreatment group, there is a significant (p = 0.0039, by the paired t test) improvement in the mean BCVA at month 6 compared with baseline. There are no significant differences (p = 0.13, p = 0.27, respectively, Mann–Whitney U test) in the BCVA at baseline and month 60 between the groups
Distribution of the mean best-corrected visual acuity (BCVA) changes from baseline after treatment with photodynamic therapy. Eighteen eyes had an increase in the BCVA of three or more lines, 23 eyes had stable VA, and 19 eyes had a decrease in the BCVA of three or more lines at month 60. Months 3, 6, 9, 12, 24, 36, 48, and 60 indicate 3, 6, 9, 12, 24, 36, 48 and 60 months after treatment
Thirty-six eyes were treated with only PDT (PDT group). The mean GLD of all lesions was 4,835 μm. In the PDT group, the mean logMAR BCVA levels at baseline and months 3, 6, 12, 24, 36, 48, and 60 were 0.73, 0.55, 0.54, 0.54, 0.55, 0.64, 0.64, and 0.68, respectively (Fig. 1). Significant (p = 0.0024, p = 0.0022, p = 0.0064, p = 0.0064, respectively, by the paired t test) improvements in the mean BCVA were seen at months 3, 6, 12, and 24 compared with baseline. The mean changes in the BCVA at months 3, 6, 12, 24, 36, 48, and 60 were improvements of 1.78, 1.94, 1.91, 1.79, 0.94, 0.93, and 0.44 lines, respectively. The mean number of treatments of PDT was 2.31. At month 60, six eyes had polypoidal lesions, nine eyes had recurrent exudation despite complete regression of the polypoidal lesions seen on ICGA, one eye had a subretinal hemorrhage; 20 eyes had no exudation in the PDT group. Figure 3 shows the ocular images obtained from a patient in the PDT group.
A 64-year-old man was treated with photodynamic therapy (PDT) for polypoidal choroidal vasculopathy (PDT group). (a, b, c, d) At baseline, the best-corrected visual acuity (VA) is 0.3 decimal VA in the right eye with PCV. a Red-free photograph showing a protruding orange-red elevated structure, subretinal hemorrhages, a serous retinal detachment (SRD), and lipid at the macular area. b Fluorescein angiography showing occult choroidal neovascularization. c Indocyanine green angiography (ICGA) clearly shows polypoidal lesions and branching vascular network vessels. d Horizontal optical coherence tomography (OCT) image showing an SRD and anterior protrusion of a highly reflective layer corresponding to the polypoidal lesions. PDT was applied (laser spot size, 4,200 μm) as the initial treatment. e, f, g, h Three months after the initial PDT (month 3), the BCVA improved to 1.0 decimal VA. e Red-free photograph showing absorption of the hemorrhage. f FA showing decreased leakage at the macular area. g ICGA showing complete regression of the polypoidal lesions. h Vertical OCT image showing that the SRD has resolved. No additional treatment is needed. i, j, k, l At month 30, the BCVA remains 1.0 decimal VA. No recurrence is documented by (i) a red-free photograph, (j) FA, (k) ICGA, and (l) horizontal OCT. m, n At month 56, the BCVA remains 1.2 decimal VA. m A red-free photograph and (n) a horizontal OCT show no exudation. o, p, q, r One application of PDT was administered until month 60. p FA showing increased leakage at the macular area. q ICGA showing branching vascular network vessels and complete regression of the polypoidal lesions. r Vertical OCT image showing that the SRD has increased in size
Retreatments were performed in 24 eyes except for PDT monotherapy (supplemental retreatment group) a mean of 26.9 months after baseline; using combined therapy of IVTA and PDT (seven eyes), IVB (12 eyes), IVB plus PDT (one eye), and IVR (four eyes). The mean GLD of all lesions at baseline was 5,230 μm. In the supplemental retreatment group, the mean logMAR BCVA levels at baseline and months 3, 6, 12, 24, 36, 48, and 60 were 0.55, 0.45, 0.37, 0.48, 0.70, 0.77, 0.74, and 0.74, respectively (Fig. 1). A significant (p = 0.0039, by the paired t test) improvement in the mean BCVA was seen at month 6 compared with baseline. The mean changes in BCVA were improvements of 1.07, 1.81, and 0.69 lines at months 3, 6, and 12, declines of 1.43, 2.15, 1.88, and 1.69 lines at months 24, 36, 48, and 60, respectively. There were no significant (p = 0.13, p = 0.23, p = 0.061, respectively, Mann–Whitney U test) differences in the baseline BCVA, GLD, and the mean changes at month 60 between the groups (Table 3). The mean number of treatments of PDT at month 60 including combined therapy was 3.79, which was significantly (p < 0.001, Mann–Whitney U test) different compared with the PDT group.
Anti-VEGF supplementary treatment was performed in 23 (95.8 %) of the 24 retreated eyes during follow-up. In these 23 eyes, the mean number of injections at month 60 was 5.6. After additional retreatment with anti-VEGF supplementation, the mean logMAR BCVA improved from 0.72 at the time of the additional treatment to 0.70 at month 60. Six (25 %) of the 24 retreated eyes had an increased BCVA of three lines or more, six eyes (25 %) had stable VA, and 12 (50 %) eyes had a decrease in the BCVA of three lines or more at the time of the additional treatment. At 60 months, five (20.8 %) eyes had an increase in the BCVA of three or more lines, 15 eyes (62.5 %) had stable VA, and four (16.7 %) eyes had a decrease in the BCVA of three or more lines. The percentage of eyes with a decrease in the BCVA at the time of the additional treatment was significantly (p = 0.031, Chi-square test) higher than that at month 60. Table 3 shows status at month 60 in both groups. Figure 4 shows ocular images obtained from a patient in the supplemental retreatment group.
A 76-year-old man was treated with photodynamic therapy (PDT) for polypoidal choroidal vasculopathy (supplemental retreatment group). (A, B, C, D) At baseline, the best-corrected visual acuity (VA) is 0.5 decimal VA in the right eye with PCV. a Red-free photograph showing subretinal hemorrhages, a pigment epithelial detachment (PED), and lipid at the macular area. b Fluorescein angiography (FA) showing occult choroidal neovascularization (CNV) and a PED. c Indocyanine green angiography (ICGA) clearly shows polypoidal lesions and branching vascular network vessels. d A horizontal optical coherence tomography (OCT) image showing a PED and anterior protrusion of a highly reflective layer corresponding to the polypoidal lesions. PDT was applied (laser spot size, 3,250 μm) as the initial treatment. e, f, g, h Three months after the initial PDT (month 3), the BCVA has improved to 0.6 decimal VA. e Red-free photograph showing absorption of the hemorrhage. f FA showing new leakage from classic CNV at the macular area. g ICGA showing complete regression of the polypoidal lesions. (H) Vertical OCT image showing decreased PED. An additional PDT was needed to treat classic CNV. i, j, k, l At month 18, the BCVA has decreased to 0.3 decimal VA. i A red-free photograph showing a large subretinal hemorrhage and increased hard exudation. j FA showing blockage due to large subretinal hemorrhage. k ICGA showing recurrent polypoidal lesions. l Vertical OCT image showing that the PED has increased in size and macular edema. Combined therapy of intravitreal triamcinolone acetonide (IVTA) and PDT was administered. m, n, o, p At month 21 (3 months after the combined therapy of IVTA and PDT), the BCVA has decreased to 0.2 decimal VA. m A red-free photograph showing that the subretinal hemorrhage has decreased in size. n FA showing decreased leakage at the macular area. o ICGA showing complete regression of the polypoidal lesions. p Vertical OCT image showing that the PED has decreased in size and absorption of the macular edema. No additional treatment was needed. q, r, s, t At month 45, the BCVA decreased to 0.06 decimal VA. q New subretinal hemorrhage and vitreous hemorrhage are seen in a red-free photograph. r FA showing increased leakage at the macular area. s ICGA showing no polypoidal lesions. t Vertical OCT image showing recurrent macular edema. Intravitreal bevacizumab injection (IVB) was administered as additional retreatment. u, v At month 60, after two PDTs, one combined therapy IVTA and PDT, and one IVB, the BCVA decreased to 0.01 decimal VA from baseline. u Red-free photograph showing no subretinal hemorrhage or residual vitreous hemorrhage. v Vertical OCT image showing no exudation
Multiple linear regression analysis showed that the mean changes in the BCVA at month 60 were significantly related to the classic component (p = 0.026) and GLD (p = 0.0076) (Table 4). Sixteen eyes had a GLD of 3,600 μm or less, 20 eyes had a GLD over 3,600 to 5,400 μm, and 24 eyes had a GLD exceeding 5,400 μm (Table 5). Figure 5 shows the mean changes in the BCVA from baseline to month 60 by lesion size. The mean logMAR BCVA improved significantly (p < 0.001) from 0.75 at baseline to 0.45 at month 60 in eyes with GLD of 3,600 μm or less, was maintained in eyes with GLD from 3,600 to 5,400 μm (0.66 at baseline to 0.63 at month 60), and declined significantly (p = 0.0032) in eyes with a GLD of exceeding 5,400 μm (0.60 at baseline to 0.95 at month 60).
Graph showing changes in the mean logarithm of the minimum angle of resolution best-corrected visual acuity (logMAR BCVA) from baseline to 60 months according to the greatest linear dimension (GLD). The mean BCVA significantly (p < 0.001) improved at month 60 in eyes with a GLD of ≤ 3,600 μm, is maintained in eyes with GLD over 3,600 to 5,400 μm, and significantly (p = 0.0032) declined in eyes with a GLD exceeding 5,400 μm
Unexpected subretinal hemorrhages were seen in 17 (28.3 %) of the 60 eyes a mean of 2.4 months after the initial treatment in 13 eyes, a mean of 9.1 months after the second PDT in two eyes and a mean of 1.9 months after the third PDT in two eyes during 60 months of follow-up. The size of the subretinal hemorrhage was 1 disc diameter or less in two eyes, over 1 disc diameter and within the arcade vessels in 12 eyes, and beyond the arcade vessels in three eyes. Five of the 17 eyes had recurrent subretinal hemorrhages. A vitreous hemorrhage developed in one (1.7 %) eye 35 months after the initial PDT in a patient with a BCVA that improved 4.77 lines at month 60. No other complications developed, such as inflammation, increased intraocular pressure over 21 mmHg, severe visual loss, endophthalmitis, or systemic adverse events.
Discussion
The current study showed the long-term efficacy and usefulness associated with PDT for PCV. Twenty-four of the 60 eyes needed additional treatment other than PDT monotherapy during 60 months of follow-up. The mean change in the BCVA was a decrease of 0.50 line at month 60. The efficacy of PDT for PCV was correlated significantly with the GLD.
PDT with verteporfin maintained or improved the VA and resolved the polypoidal lesions in eyes with PCV [13–15]. The Japanese Guidelines for PDT highly recommended PDT for patients with PCV [13]. However, the follow-up was less than 24 months in most reports. The studies with longer follow-up periods, i.e., PDT studies with 2 [15, 16] or 3 years of follow-up [17, 18], reported a decrease in VA at the final visit. Recently, a PDT study with a 5-year follow-up reported that 88.1 % of patients with PCV had stable or improved BCVA and recurrences were seen in 78.6 % of eyes during follow-up [19]. In the current study, the logMAR BCVA declined from 0.66 at baseline to 0.71 at month 60. However, multiple linear regression analysis showed that the mean change in the BCVA at month 60 was correlated significantly with the classic component (p = 0.026) and GLD (p = 0.0076). Therefore, when we evaluated the GLD by size, i.e., 3,600 μm or less, over 3,600 to 5,400 μm, and over 5,400 μm, according to the Japanese Guidelines for PDT [13], we found that the mean BCVA improved significantly in eyes with a GLD of 3,600 μm or less, maintained in eyes with a GLD of over 3,600 to 5,400 μm, and significantly decreased in eyes with a GLD exceeding 5,400 μm. Based on these results, PDT for patients with PCV was highly recommended in eyes with a GLD of 3,600 μm or less. However, the vision in eyes with untreated lesions may decrease to a greater degree than those with PDT treatment, and, therefore, it still may be worthwhile to treat larger lesions. Moreover, ICGA-guided PDT can reduce the size of laser exposure in eyes with a large GLD measured by FA, which may result in fewer decreases in VA or adverse events. Caution should be taken when considering any treatments for patients with PCV especially with a GLD over 5,400 μm because of the risk of decreasing VA.
The EVEREST study was the first double-masked, randomized, controlled trial to evaluate if PDT plus ranibizumab or PDT monotherapy was superior to ranibizumab monotherapy for achieving complete regression of polypoidal lesions (primary outcome) with a 6-month follow-up [22]. Recently, this study also showed the superior efficacy of PDT for achieving complete regression of polyps in patients with PCV.
PDT cannot resolve the branching vascular network vessels, which may cause recurrent or new polypoidal lesions or both [23]. We reported that additional PDT applications were less effective for patients with completely regressed polypoidal lesions after combined therapy but recurrent or residual exudation from branching vascular network vessels [21]. In addition, patients with PCV with classic CNV may need more applications of PDT. In the current study, we changed the retreatment based on the time period with combined therapy of IVTA and PDT, IVB, IVB plus PDT, and IVR from PDT for patients with recurrent exudation from branching vascular network vessels or classic CNV in the supplemental retreatment group. After additional treatment, except for PDT monotherapy, the mean logMAR BCVA improved from 0.72 at the time of the additional treatment to 0.70 at month 60, which may prevent VA decreases. Moreover, the percentage of eyes with a decrease in BCVA at the time of the additional treatment (50 %) was significantly (p = 0.031, Chi-square test) higher than at month 60 (16.7 %). This retreatment strategy may be important to safely avoid VA decreases.
The mean number of PDT applications at month 60 in all eyes was 2.88. Leal et al. [18], who reported the 3-year results of PDT for patients with PCV, found that the mean number of treatments of PDT at 36 months was 3.19, which exceeded that of the current study at month 60. In the current study, the change in retreatment to combined therapy of IVTA and PDT, IVB, IVB plus PDT, or IVR from PDT monotherapy may reduce the number of PDT applications during a long follow-up period.
An unexpected increase in the number of subretinal hemorrhages and severe vision loss without recurrence are well-known complications of PDT monotherapy in patients with PCV with incidence rates ranging from 18 to 30 % [14, 15, 20, 23]. In the current study, unexpected subretinal hemorrhages developed in 17 (28.3 %) of the 60 eyes during the 60 months of follow-up, which was similar to previous reports. A vitreous hemorrhage developed in one eye (1.7 %) 35 months after the initial PDT. Although the BCVA improved by 4.77 lines at month 60, caution should be taken when subretinal hemorrhages develop. Moreover, anti-VEGF therapy may be a better treatment for patients with increasing subretinal hemorrhages to avoid enlargement of the subretinal hemorrhage compared with PDT monotherapy.
In conclusion, the current study showed that the efficacy of PDT for PCV significantly depended on the GLD, i.e., the BCVA significantly improved in eyes with a GLD of 3,600 μm or less, was maintained in eyes with GLD of from over 3,600 to 5,400 μm, and significantly declined in eyes with GLD of over 5,400 μm at month 60. Because this study was a retrospective review of results with highly variable retreatment methods and no control group, large, long-term, prospective randomized studies are needed to determine the efficacy and safety profiles of PDT for patients with PCV.
References
Yannuzzi LA, Sorenson J, Spaide RF, Lipson B (1990) Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina 10:1–8
Spaide RF, Yannuzzi LA, Slakter JS, Sorenson J, Orlach DA (1995) Indocyanine green videoangiography of idiopathic polypoidal choroidal vasculopathy. Retina 15:100–110
Yannuzzi LA, Ciardella A, Spaide RF, Rabb M, Freund KB, Orlock DA (1997) The expanding clinical spectrum of idiopathic polypoidal choroidal vasculopathy. Arch Ophthalmol 115:478–485
Imamura Y, Engelbert M, Iida T, Freund KB, Yannuzzi LA (2010) Polypoidal choroidal vasculopathy: a review. Surv Ophthalmol 55:501–515
Maruko I, Iida T, Saito M, Nagayama D, Saito K (2007) Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol 144:15–22
Lafaut BA, Leys AM, Snyers B, Rasquin F, De Laey JJ (2000) Polypoidal choroidal vasculopathy in Caucasians. Graefes Arch Clin Exp Ophthalmol 238:752–759
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, Kim RY, MARINA Study Group (2006) Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 355:1419–1431
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, Sy JP, Schneider S, ANCHOR Study Group (2006) Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 355:1432–1444
Mitchell P, Korobelnik JF, Lanzetta P, Holz FG, Prünte C, Schmidt-Erfurth U, Tano Y, Wolf S (2010) Ranibizumab (Lucentis) in neovascular age-related macular degeneration: evidence from clinical trials. Br J Ophthalmol 94:2–13
Gomi F, Sawa M, Sakaguchi H, Tsujikawa M, Oshima Y, Kamei M, Tano Y (2008) Efficacy of intravitreal bevacizumab for polypoidal choroidal vasculopathy. Br J Ophthalmol 92:70–73
Kokame GT, Yeung L, Lai JC (2010) Continuous anti-VEGF treatment with ranibizumab for polypoidal choroidal vasculopathy: an interim 6-month report. Br J Ophthalmol 94:297–301
Hikichi T, Higuchi M, Matsushita T, Kosaka S, Matsushita R, Takami K, Ohtsuka H, Ariga H (2012) One-year results of three monthly ranibizumab injections and as-needed reinjections for polypoidal choroidal vasculopathy in Japanese patients. Am J Ophthalmol 154:117–124
Tano Y, Ophthalmic PDT Study Group (2008) Guidelines for PDT in Japan. Ophthalmology 115:585
Gomi F, Ohji M, Sayanagi K, Sawa M, Sakaguchi H, Oshima Y, Ikuno Y, Tano Y (2008) One-year outcomes of photodynamic therapy in age-related macular degeneration and polypoidal choroidal vasculopathy in Japanese patients. Ophthalmology 115:141–146
Saito M, Iida T, Nagayama D (2008) Photodynamic therapy with verteporfin for age-related macular degeneration or polypoidal choroidal vasculopathy: comparison of the presence of serous retinal pigment epithelial detachment. Br J Ophthalmol 92:1642–1647
Kurashige Y, Otani A, Sasahara M, Yodoi Y, Tamura H, Tsujikawa A, Yoshimura N (2008) Two-year results of photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol 146:513–519
Akaza E, Yuzawa M, Mori R (2011) Three-year follow-up results of photodynamic therapy for polypoidal choroidal vasculopathy. Jpn J Ophthalmol 55:39–44
Leal S, Silva R, Figueira J, Cachulo ML, Pires I, de Abreu JR, Cunha-Vaz JG (2010) Photodynamic therapy with verteporfin in polypoidal choroidal vasculopathy: results after 3 years of follow-up. Retina 30:1197–1205
Kang HM, Kim YM, Koh HJ (2012) Five-year follow-up results of photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. doi:10.1016/j.ajo.2012.09.020
Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group (1999) Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials—TAP Report 1. Arch Ophthalmol 117:1329–1345
Saito M, Iida T, Kano M (2011) Intravitreal ranibizumab for polypoidal choroidal vasculopathy with recurrent or residual exudation. Retina 31:1589–1597
Koh A, Lee WK, Chen LJ, Chen SJ, Hashad Y, Kim H, Lai TY, Pilz S, Ruamviboonsuk P, Tokaji E, Weisberger A, Lim TH (2012) EVEREST STUDY: efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina 32:1453–1464
Akaza E, Mori R, Yuzawa M (2008) Long-term results of photodynamic therapy of polypoidal choroidal vasculopathy. Retina 28:717–722
Conlict of interest
The authors have no proprietary interest in any aspect of this study and received no government funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saito, M., Iida, T., Kano, M. et al. Five-year results of photodynamic therapy with and without supplementary antivascular endothelial growth factor treatment for polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol 252, 227–235 (2014). https://doi.org/10.1007/s00417-013-2433-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2433-1