Abstract
Background
The pathogenesis of normal tension glaucoma (NTG) might be related to impaired autoregulation of ocular blood flow. The purpose of the study is to evaluate retinal haemodynamics by fluorescein angiography and to correlate arteriovenous passage times (AVP) with ocular perfusion pressure in patients with NTG and controls.
Methods
Thirty-five patients with NTG without any topical treatment (mean age 53 ± 11 years) and 35 age-matched controls (mean age 53 ± 11 years) were included in this study. Retinal AVP was assessed by video fluorescein angiography using a scanning laser ophthalmoscope (Rodenstock, Germany). Dye dilution curves of temporal superior and inferior arterioles and venules were evaluated by digital image analysis. AVP was correlated to mean arterial blood pressure and ocular perfusion pressure.
Results
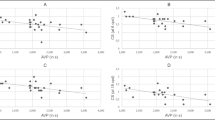
The AVP was significantly prolonged in patients with NTG compared to controls (1.82 ± 0.57 versus 1.42 ± 0.46, p = 0.002). Patients with NTG and controls showed no significant differences in intraocular pressure, mean arterial pressure and mean and diastolic ocular perfusion pressure. The AVP was significantly correlated to mean arterial pressure and mean and diastolic ocular perfusion pressure in patients with NTG (r = −0.54; p = 0.0006, r = −0.51; p = 0.002, r = −0.49, p = 0.002), but not in controls (r = −0.21; p = 0.23, r = −0.19; p = 0.27, r = 0.02, p = 0.93).
Conclusions
Patients with NTG exhibit prolonged retinal AVP compared to controls. A significant correlation of retinal haemodynamics to mean arterial blood pressure and ocular perfusion pressure might reflect impaired autoregulation in NTG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disorders of ocular haemodynamics are a major factor in the pathogenesis of glaucomatous optic neuropathy [1–4]. The arteriovenous passage time (AVP), characterizing retinal haemodynamics, may be determined by fluorescein angiography. The retinal AVP represents the shortest passage time from the first influx of fluorescein dye in retinal arterioles to the first arrival in corresponding retinal venules passing retinal microcirculation [5, 6]. Previous studies have shown that the measurement of AVP is reproducible and prolonged in ischemic retinal disease and glaucoma [1, 7–11]. In asymmetric glaucomatous visual field loss, the AVP is significantly prolonged in the hemifield with the larger visual field defect, suggesting a link between retinal haemodynamics and visual function in glaucoma [12].
In healthy subjects, retinal blood flow is autoregulated to provide a constant blood flow regardless of changes in ocular perfusion pressure [13–18]. Endothelium derived vasoactive agents and pericyte contractility are important actors of local blood flow regulation, as well as smooth muscle cells of blood vessels and vessel anatomy. The mechanisms of blood-flow autoregulation are only effective in a certain range of perfusion pressure [19–21]. Ocular perfusion pressure is determined by systemic blood pressure and intraocular pressure (IOP). Decreased ocular perfusion pressure due to high IOP or low arterial blood pressure might result in decreased ocular haemodynamics if autoregulation is impaired. This could be a risk factor for progression in glaucoma [2].
In 1981, Riva et al. showed that retinal blood flow is autoregulated up to IOP values of 30 mmHg in healthy subjects using the blue field simulation technique [16]. Macular blood flow is maintained down to an IOP low as 7 mmHg [13]. Riva et al. confirmed these findings on retinal autoregulation using the laser Doppler phenomenon in 1986 [15]. However, retinal AVP is significantly prolonged when IOP reaches values of 34 mmHg [22]. Zetlan et al. showed that blue field macular blood flow parallels changes found in visual evoked potentials during increases in IOP. A relationship between retinal haemodynamics and visual pathway activity as measured by visual evoked potentials was suggested, and patients with glaucoma failed to demonstrate these associations [18, 23]. Retinal blood flow determined by laser Doppler velocimetry maintains stable during increases in mean arterial blood pressure of up to 40% [17]. Harris et al. found a constriction of retinal arterioles and an increase in mean dye velocity during dynamic exercise. Calculated retinal blood flow remained unchanged [14].
In contrast, impaired autoregulation might lead to a higher susceptibility of ocular tissues to decreased perfusion pressure in glaucoma [2, 24, 25]. Epidemiological trials found that low perfusion pressures were associated with a higher prevalence of primary open-angle glaucoma [26, 27]. Diastolic perfusion pressures below 30 mmHg were related to a 6-fold higher risk for glaucoma compared to higher perfusion pressures [27].
The present study investigates the correlation of systemic blood pressure and ocular perfusion pressure with the retinal AVP in patients with normal tension glaucoma (NTG) and controls.
Materials and methods
Methods
All patients with NTG and control subjects had a detailed ophthalmological examination and visual field testing. Visual field examinations were performed with the Humphrey Field Analyzer (Model 750, Humphrey-Zeiss, San Leandro, CA, USA: 24-2 full-threshold or SITA program). One eye was randomly selected for the study in patients with bilateral NTG (coin toss). In patients with unilateral NTG, the diseased eye was included in the study. Adherence to the Declaration of Helsinki for research involving human subjects is confirmed. Informed consent was obtained from all subjects. Data accumulation was carried out with Institutional Review Board approval.
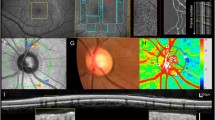
Video fluorescein angiograms were obtained with a scanning laser ophthalmoscope (Rodenstock, Ottobrunn, Germany). The methods are described in detail elsewhere [1, 5, 6]. The 40-degree observation mode was used with the optic nerve head centred. To start the angiography, 10% sodium-fluorescein dye (2.5 cc) was injected into an antecubital vein. The image acquisition parameters (video gain and laser intensity) were kept constant until the maximum intensity levels in the retinal venules were passed over to avoid artefacts. Dynamic sequences were acquired with a frequency of 25 images per second. The angiograms were analysed off-line by means of digital image analysis (Matrox Inspector, Matrox Inc., Quebec, Canada) in a masked manner. The retinal AVP was determined using dye dilution curve analysis. The intensity level for each image was determined at a fixed region of interest (ROI) located on the arterioles respective venules. The extent of the ROI (circle) was chosen to correspond to the vessel diameter. Measurements were performed in the superotemporal and inferotemporal arterioles and venules. The mean retinal AVP was used for analysis.
Before fluorescein angiography, intraocular pressure was measured in a sitting position using Goldmann applanation tonometry. Systolic and diastolic blood pressure and heart rate were measured after a rest of 5 minutes (Dinamap, Criticare Systems Inc., USA). Mean ocular perfusion pressure (PP) was calculated as: PP = 2/3 (MAP) -IOP, where mean arterial pressure (MAP) is defined as: diastolic blood pressure +1/3 (systolic blood pressure - diastolic blood pressure). Diastolic ocular perfusion pressure (dPP) was calculated as: dPP = 2/3 (diastolic blood pressure) - IOP.
Patients
Thirty-five patients with NTG and 35 age-matched controls were included in the study. All patients with NTG had glaucomatous optic nerve head cupping and glaucomatous visual field defects as defined by the European Glaucoma Society in absence of retinal or neurological disease affecting the visual field [28]. Visual field loss was considered significant when: (a) the glaucoma hemifield test was abnormal, (b) three points were confirmed with p < 0.05 probability of being normal, not contiguous with the blind spot, or (c) corrected pattern standard deviation (CPSD) was abnormal with p < 0.05. All parameters were confirmed on two consecutive visual fields performed with the Humphrey Visual Field Analyzer (full threshold program 24-2) within 6 weeks. Patients with NTG never had IOP values above 21 mmHg, confirmed with IOP measurements at 8 a.m., 12 a.m., 4 p.m, 8 p.m., 12 p.m. (1 day IOP profile) without any IOP-lowering medication. Visual acuity was 20/40 or better, and no previous laser or surgical treatment had been performed. Patients with refractive aberrations of more than ±8 diopters, or with diabetes mellitus were excluded from this study. The control subjects did not have any ophthalmologic disease, presented with IOP values below 22 mmHg and normal visual field examinations.
No patient with NTG received topical IOP-lowering treatment. Patients were either newly diagnosed NTG patients or had a washout period of 3 weeks without any IOP-lowering medication. No control subject received any topical treatment. The clinical and demographic data of all individuals included in the study are presented in Table 1.
Statistical analysis
An unpaired t-test was applied for comparisons between patients with NTG and controls. Correlations were tested using the Fisher’s r to z test. In all analyses, p < 0.05 was regarded as statistically significant.
Results
The retinal AVP was significantly prolonged in patients with NTG compared to controls. Intraocular pressure, systolic, diastolic, mean arterial pressure and calculated mean and diastolic ocular perfusion pressure were not significantly different between groups (Table 1).
The AVP was significantly correlated to mean arterial pressure, mean ocular perfusion pressure, and diastolic ocular perfusion pressure in NTG. Control subjects exhibited no correlation of systemic blood pressure, mean ocular perfusion pressure or diastolic ocular perfusion pressure with AVP. No correlation of AVP to IOP or age was found in patients with NTG or controls. The results are presented in Tables 2 and 3 and Figs. 1 and 2. The comparison of the correlation coefficients revealed a significantly different correlation for the diastolic ocular perfusion pressure and AVP between patients with NTG and controls (p = 0.026).
Discussion
Past studies provide evidence that the retinal vasculature is autoregulated to maintain constant blood flow regardless of changes in ocular perfusion pressure in healthy subjects [13–18]. In contrast, an impaired ocular blood flow regulation is apparent in glaucomatous optic neuropathy. In primary open-angle glaucoma (POAG), a defective autoregulation of macular blood flow compared to controls was shown by Grunwald et al. in 1984 after artificial IOP increase by a suction cup [24]. Pillunat et al. found a different pattern of visually evoked response during IOP increase in patients with NTG. In contrast to healthy controls, patients with NTG exhibit a linear decrease of visual evoked response amplitudes during IOP elevation [25]. Robert et al. suggested that the optic nerve head brightness is an expression of capillary blood volume, and found that during IOP elevation the optic nerve head brightness persisted for a shorter time in patients with POAG than in controls [29]. Retinal vessel diameters tend to show a smaller reaction upon intraocular pressure provocation up to suprasystolic values in patients with POAG than in controls [30].
In our study, a significant prolongation of the retinal AVP was confirmed in patients with NTG compared to controls [1, 11, 31]. The retinal AVP, prolonged in ischemic disease of the retina [7–10], represents the shortest passage of the fluorescein dye through the capillary formation. The retinal AVP might reflect alterations in retinal microcirculation, and is not related to capillary dropout of the posterior pole or retinal vessel diameters in glaucoma [5]. Further, the AVP is correlated to flow velocities and resistive indices of the central retinal artery and short posterior ciliary arteries [32]. Our investigation shows that AVP is correlated to mean and diastolic ocular perfusion pressure and mean arterial pressure in patients with untreated NTG, but not in controls. The direct comparison between patients with NTG and controls showed a significantly different correlation for the diastolic ocular perfusion pressure and AVP. This finding supports the concept of an impaired retinal blood flow regulation in NTG, although we did not measure AVP at baseline and after ocular perfusion pressure change. Most of the previous studies investigated the phenomenon of blood flow regulation related to changes in ocular perfusion pressure in patients with POAG [24, 29, 30, 33, 34]. In POAG, an abnormal association of optic nerve head blood flow [33, 34] and choroidal blood flow [34] with systemic blood pressure or ocular perfusion pressure was shown. This phenomenon is also present in patients with NTG, as shown by our study on retinal haemodynamics. The results emphasise the impact of a deficient blood flow regulation during changes in ocular perfusion pressure and systemic blood pressure. The diastolic ocular perfusion pressure represents the lowest perfusion pressure levels during the heart cycle, and can be interpreted as the steady component of perfusion pressure. The presented data suggest that decreased diastolic perfusion pressure due to low diastolic blood pressure levels is relevant for decreased retinal haemodynamics in NTG. Interestingly, the AVP was not correlated to IOP in the present study. Therefore, the control of systemic blood pressure as the major component of calculated ocular perfusion pressure seems to be highly relevant to maintaining constant ocular blood flow in patients with NTG. In a recent investigation on 24-hour blood pressure monitoring in glaucoma, more profound night-time blood pressure fluctuations could be found in patients with NTG [35]. Such alterations in systemic blood pressure result in ocular perfusion pressure fluctuations. A defective blood flow regulation in glaucoma might then be relevant for recurring ischemic episodes of ocular tissues. The therapeutic lowering of IOP in glaucoma increases the ocular perfusion pressure, and might reduce the risk of an impairment of ocular haemodynamics. However, it is essential to evaluate the systemic blood pressure data in glaucoma patients in order to limit the risk of low diastolic perfusion pressures, e.g. in the case of extensive antihypertensive treatment. In the future, agents that interact with vascular resistance might contribute to diminishing the rate of progression in glaucoma.
The considerable overlap of AVP times between the patients with NTG and controls limits the interpretation of our results with regard to an individual patient. Prospective longitudinal studies are required to investigate the individual risk of progression when prolonged AVP times are present. Another limitation is the possible influence of systemic vascular disease in the patients with NTG, which might confound the results of our study. However, large-scale studies are necessary to investigate the potential role of systemic disease and medications in the relation between blood pressure and retinal haemodynamics. A certain selection bias of the patients with NTG sent to our clinic cannot be excluded.
In conclusion, our study showed that retinal AVP is prolonged in patients with NTG, suggesting decreased retinal haemodynamics. In addition, retinal AVP was correlated with ocular perfusion pressure and systemic blood pressure in NTG. A defective blood flow regulation may account for this association, which is not present in healthy subjects. A higher susceptibility of ocular tissues in glaucoma to fluctuations in ocular perfusion pressure may be related to recurring ischemic episodes [2,20]. This may be a relevant factor in the pathogenesis of glaucomatous optic neuropathy.
References
Arend O, Plange N, Sponsel WE, Remky A (2004) Pathogenetic aspects of the glaucomatous optic neuropathy: fluorescein angiographic findings in patients with primary open-angle glaucoma. Brain Res Bull 62:517–524
Flammer J, Orgül S (1998) Optic nerve blood-flow abnormalities in glaucoma. Prog Retin Eye Res 17(2):267–289
Hayreh SS (1995) The 1994 Von Sallman lecture: the optic nerve circulation in health and disease. Exp Eye Res 61:259–272
Plange N, Kaup M, Huber K, Remky A, Arend O (2006) Fluorescein filling defects of the optic nerve head in normal tension glaucoma, primary open-angle glaucoma, ocular hypertension and healthy controls. Ophthal Physiol Opt 26:26–32
Arend O, Remky A, Plange N, Martin BJ, Harris A (2002) Capillary density and retinal diameter measurements and their impact on altered retinal circulation in glaucoma: a digital fluorescein angiographic study. Br J Opthalmol 86:429–433
Wolf S, Arend O, Reim M (1994) Measurement of retinal hemodynamics with scanning laser ophthalmoscopy: reference values and variation. Surv Ophthalmol 38:S95–S100
Bertram B, Wolf S, Fiehofer S, Schulte K, Arend O, Reim M (1991) Retinal circulation times in diabetes mellitus type 1. Br J Ophthalmol 75:462–465
Bertram B, Hoberg A, Wolf S, Schulte K, Reim M (1991) Video fluorescein angiography studies in acute anterior ischemic optic neuropathy. Klin Monatsbl Augenheilk 199:419–423
Remky A, Wolf S, Hamid M, Bertram B, Schulte K, Arend O, Reim M (1994) Effect of hemodilution on retinal hemodynamics in retinal branch vein occlusion. Ophthalmologe 91:288–292
Wolf S, Arend O, Bertram B, Remky A, Schulte K, Wald KJ, Reim M (1994) Hemodilution therapy in central retinal vein occlusion. One-year results of a prospective randomized study. Graefes Arch Clin Exp Ophthalmol 232:33–39
Wolf S, Arend O, Sponsel WE, Schulte K, Cantor LB, Reim M (1993) Retinal hemodynamics using scanning laser ophthalmoscopy and hemorheology in chronic open-angle glaucoma. Ophthalmology 100:1561–1566
Arend O, Remky A, Cantor LB, Harris A (2000) Altitudinal visual field asymmetry is coupled with altered retinal circulation in patients with normal pressure glaucoma. Br J Ophthalmol 84:1008–1012
Grunwald JE, Sinclair SH, Riva CE (1982) Autoregulation of the retinal circulation in response to decrease of intraocular pressure below normal. Invest Ophthalmol Vis Sci 23:124–127
Harris A, Arend O, Bohnke K, Kroepfl E, Danis R, Martin B (1996) Retinal blood flow during dynamic exercise. Graefes Arch Clin Exp Ophthalmol 234:440–444
Riva CA, Grunwald JE, Petrig BL (1986) Autoregulation of human retinal blood flow. An investigation with laser Doppler velocimetry. Invest Ophthalmol Vis Sci 27:1706–1712
Riva CE, Sinclair SH, Grunwald JE (1981) Autoregulation in retinal circulation in response to decrease of perfusion pressure. Invest Ophthalmol Vis Sci 21:34–38
Robinson F, Riva CE, Grunwald JE, Petrig BL, Sinclair SH (1986) Retinal blood flow autoregulation in response to an acute increase in blood pressure. Invest Ophthalmol Vis Sci 27:722–726
Zetlan SR, Sponsel WE, Stodtmeister R (1992) Retinal capillary hemodynamics, visual-evoked potentials, and pressure tolerance in normal human eyes. Invest Ophthalmol Vis Sci 33:1857–1863
Anderson DR (1996) Glaucoma, capillaries and pericytes, 1. Blood flow regulation. Ophthalmologica 210:257–262
Hayreh SS (1997) Factors influencing blood flow in the optic nerve head. J Glaucoma 6:412–425
Orgül S, Gugleta K, Flammer J (1999) Physiology of perfusion as it relates to the optic nerve head. Surv Ophthalmol 43:S17–S26
Schulte K, Wolf S, Arend O, Harris A, Henle C, Reim M (1996) Retinal hemodynamics during increased intraocular pressure. German J Ophthalmol 5:1–5
Sponsel WE, Zetlan SR, Stodtmeister R, Kaufman P (1997) Retinal capillary hemodynamics and VEP/pressure tolerance: evidence of retinal microcirculatory compromise in treated glaucomatous eyes. Ophthalmologica 211:172–177
Grunwald JE, Riva CE, Stone RA, Keates EU, Petrig BE (1984) Retinal autoregulation in open-angle glaucoma. Ophthalmology 91:1690–1694
Pillunat LE, Stodtmeister R, Wilmanns I (1987) Pressure compliance of the optic nerve head in low tension glaucoma. Br J Ophthalmol 71:181–187
Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A (2000) Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt study. Ophthalmology 107:1287–93
Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt JC (1995) Hypertension, perfusion pressure, and primary open-angle glaucoma. A population-based assessment. Arch Ophthalmol 113:216–221
European Glaucoma Society (2003) In: Traverso CE, Grehn F, Hollo G, Lachkar Y, Migdal C, Thygesen J (eds) Terminology and guidelines for glaucoma. 2nd edn. Editrice DOGMA S.r.l., Savona Italy, pp 24–32
Robert Y, Steiner D, Hendrickson P (1989) Papillary circulation dynamics in glaucoma. Graefes Arch Clin Exp Ophthalmol 227:436–439
Nagel E, Vilser W, Lanzl IM (2001) Retinal vessel reaction to short-term IOP elevation in ocular hypertensive and glaucoma patients. Eur J Ophthalmol 11:338–344
Arend O, Remky A, Redbrake C, Arend S, Wenzel M, Harris A (1999) Retinale Hämodynamik bei Patienten mit Normaldruckglaukom. Ophthalmologe 96:24–29
Huber K, Plange N, Remky A, Arend O (2004) Comparison of colour Doppler imaging and retinal scanning laser fluorescein angiography in healthy volunteers and normal pressure glaucoma patients. Acta Ophthalmol Scand 82(4):426–431
Grunwald JE, Piltz J, Hariprasad SM, Dupont J, Maguire MG (1999) Optic nerve blood flow in glaucoma: effect of systemic hypertension. Am J Ophthalmol 127:516–522
Fuchsjäger-Mayrl G, Wally B, Georgopoulos M, Rainer G, Kircher K, Buehl W, Amoako-Mensah T, Eichler H-G, Vass C, Schmetterer L (2004) Ocular blood flow and systemic blood pressure in patients with primary open-angle glaucoma and ocular hypertension. Invest Ophthalmol Vis Sci 45:834–839
Plange N, Kaup M, Daneljan L, Predel HG, Remky A, Arend O (2006) 24-hour blood pressure monitoring in normal tension glaucoma: night time blood pressure variability. J Hum Hypertens 20:137–142
Funding/Support
none
Financial disclosures
none
Contributions of authors
Design and conduct of the study (NP, MK, AR, OA), collection, management, analysis and interpretation of the data (NP, MK, AR, OA), preparation and approval of the manuscript (NP, MK, AR, OA).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Plange, N., Kaup, M., Remky, A. et al. Prolonged retinal arteriovenous passage time is correlated to ocular perfusion pressure in normal tension glaucoma. Graefes Arch Clin Exp Ophthalmol 246, 1147–1152 (2008). https://doi.org/10.1007/s00417-008-0807-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-008-0807-6