Abstract
Purpose
To assess visual function and its effects on vision-targeted, health-related quality of life (QOL) of patients with neovascular age-related macular degeneration (AMD) treated with photodynamic therapy (PDT) or full macular translocation (FMT).
Methods
Fifty patients with predominantly classic subfoveal choroidal neovascularisation (CNV) secondary to AMD were randomised to PDT or FMT. To test the vision-targeted QOL, the 39-item National Eye Institute Visual Function Questionnaire (NEI-VFQ-25 plus supplement) was administered prior to and 1 year after therapy. The change of vision-related QOL at 1 year in comparison to baseline was defined as primary end point.
Results
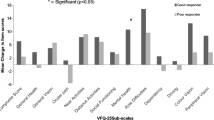
The vision-related subscales showed a stabilisation or even higher mean scores at 1 year in both treatment groups. A significant improvement in the quality of the subject’s vision-related subscales was only observed after FMT correlating with a more frequent increase in visual acuity. Comparing the results of the QOL scores after 1 year, the improvement of the subscale scores general vision (p = 0.03), mental health (p = 0.02) and dependency (p = 0.03) were significantly higher in the FMT arm.
Conclusions
FMT and PDT can achieve a stabilisation in vision-related QOL, in which FMT was superior to the PDT after 1 year. The discrepancy between the amount of patients with an increased visual acuity after FMT and a moderate improvement in QOL might be caused by the onset of complications related to this surgical procedure. Besides visual acuity, the impact of therapy-related complications has to be taken into consideration when evaluating new therapeutic concepts in exudative AMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Age-related macular degeneration (AMD) is one of the most relevant causes of blindness in the elderly segment of the western population [1]. The neovascular form of the disease is characterized by the growth of subfoveal choroidal neovascularisation (CNV) and is associated with a dramatic loss in central vision.
Some therapies were developed to limit the degree of vision loss secondary to CNV, such as photodynamic therapy (PDT) and full macular translocation (FMT) [2–7].
However, in patients who have received PDT treatment, a pronounced improvement in vision-related quality of life (QOL) was not detected [8, 9]. PDT prevents severe vision loss, but a moderate loss in visual function still occurs. Vision-related QOL is directly linked with the severity of visual loss. Therefore, an increase in vision-related QOL cannot be expected if a treatment does not lead to an improvement of visual function.
In contrast, for the FMT, a stabilisation or even an improvement of visual function and consequently an improvement of the QOL have been reported, although the rate of complications due to this therapy is high [5–7, 10].
The success of a treatment in patients with neovascular AMD cannot be estimated only by the outcome of visual acuity (VA) measurement. An additional analysis of the patient’s perception of their vision-related QOL is of utmost importance. To our knowledge there has been no prospective, randomised comparison of QOL between a non-surgical laser therapy (PDT) and a surgical treatment (FMT) to date. We compared the changes of visual acuity and QOL in eyes with subfoveal predominantly classic CNV secondary to AMD.
Materials and methods
The FMT-PDT study was a prospective, randomised, controlled, non-masked, monocenter pilot-trial for comparison of FMT and PDT in patients with classic subfoveal CNV secondary to AMD. The study was completed in compliance with the Declaration of Helsinki and the International Committee on Harmonization guidelines. Institutional review board approval and written informed consent were obtained from patients before their participation in the study. Before entry into the trial, the investigator explained to each patient the trial purpose, procedures, risks, and benefits of participation and alternative treatments available. Patients were explained that failure to enroll would not prejudice their treatment. The patient signed the informed consent statement in the presence of a witness before entry into the trial to secure that all participants were aware of the randomized nature of the allocation procedure and the different character of the treatment options. Demographic characteristics are summarized in Table 1. The inclusion and exclusion criteria of the FMT-PDT pilot trial have been recently published [11].
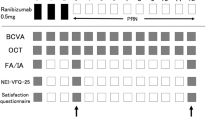
Data of QOL were prospectively gathered from patients, who consented to participate in the study from 2001 through 2005, at the initial interview prior to therapy and one year after treatment. Best corrected visual acuity (BCVA) was measured using standard refraction protocol, standard retro-illuminated Early Treatment Diabetic Retinopathy Study (ETDRS) charts (1 line = 5 letters), by an unmasked examiner.
A research assistant administered the NEI VFQ-25 with supplement at the initial interview and at the clinical visit 1 year post-treatment.
The NEI VFQ-25 is composed of a base set of 25 vision-targeted questions representing 11 vision-related constructs, plus an additional single-item general health rating question. The NEI VFQ-25 plus supplement includes an appendix of additional items from the 51-item version that can be used to expand the scales up to 39 total items [12–14]. The addition of these items enhances the reliability of various subscales of the NEI VFQ [12]. All items in the NEI VFQ-25 plus supplement are from the 51-item field test version [15]. No new items were developed for the NEI VFQ-25 plus supplement. We used the German version of the NEI VFQ-25 plus supplement, which has been translated and evaluated by Franke [16].
The 12 subscales can be summarized in three categories. The first category includes only the subscale general health (two questions). The second category consists of five subscales which subsume the quality of a subject’s vision including the subscales general vision (two questions), difficulty with distance tasks (six questions), difficulty with near tasks (six questions), peripheral vision (one question) and colour vision (one question).
The last six subscales, dependency (four questions), role difficulties (four questions), mental health (five questions), social function (three questions), driving (three questions), and ocular pain (two questions), are incorporated into a third category, which measure subject’s vision-specific QOL. Answers to each of the NEI VFQ-25 questions plus supplement are converted to a 100-point scale and each subscale represents the average of ≥1 questions.
Statistical analysis
Overall pre-treatment and post-treatment NEI VFQ-39 subscale scores were calculated. Although all 39 items were administered, the three items on driving (questions 15c, 16 and 16a) were eliminated from the final analysis because very few of the patients were legally allowed to drive, and the data were insufficient for analysis. For patients who discontinued the study, the last clinic visit was carried forward in the analysis to avoid selection bias. Completing the analysis of the collected data the results of the subscale scores before treatment were compared with the subscale scores 1 year after undergoing PDT or FMT. Additionally, the subscale scores 1 year post-treatment of the FMT arm were compared with those of the PDT. Data evaluation was conducted in accordance with the scoring algorithm developed by Mangione [17].
Data analysis was made with the statistical software package JMP5.0.1.2 (SAS Institute, Cary, NC, USA). For analysis of score changes, the Wilcoxon signed-rank test was performed. The significance level was set to α = 0.05.The Pearson correlation coefficient and significant probability (obtaining, by chance alone, a correlation with greater absolute value than the computed value if no linear relationship exists) were calculated.
Results
In each arm of the FMT-PDT pilot trial 25 eyes (25 patients) were treated. The mean age of the patients was 79.1 ± 6.47 years (range 65–91) in the FMT and 75.7 ± 5.75 years (range 65–87) in the PDT arm. Five patients could not be examined at the month-12 examination because of illness or death. 90% of the enrolled patients (45/50) completed the final control.
The demographic data (Table 1) did not differ with regard to age and gender. At baseline 60% (15/25) of the fellow eyes in the PDT arm and 36% (9/25) in the FMT arm had dry AMD, which was recorded more frequently in the PDT arm without statistical significance (p = 0.16). At the month-12 examination, 25 patients in the PDT group had an average number of 2.8 applications of PDT treatment (without the treatment at month-12 examination).
Moderate vision loss (3–5 ETDRS lines) was equal in both treatment groups (three eyes) (Table 2). However, more patients had severe vision loss (6 or more ETDRS lines) in the PDT group (six eyes) than in the FMT (two eyes). The difference between the two treatment groups was not statistically significant (p = 0.25).
A vision loss less than 3 ETDRS lines occurred in 16 eyes (64%) in the PDT group and 20 eyes (80%) in the FMT group at 12 months from the baseline. However, the difference between both treatment groups remained not statistically significant (p = 0.35).
At the month-12 examination, ten of the 25 eyes (40%) in the FMT group and no eyes in the PDT group gained 3 or more ETDRS lines of visual acuity from baseline. Although four of the 25 eyes (16%) of patients treated with PDT improved by at least 1 line, an increase of visual acuity by a similar degree was found at 12 month examination in 14 eyes (56%) in the FMT group. The difference between PDT and FMT arms was statistically significant favouring the FMT (p < 0.01).
The more pronounced improvement in VA in the FMT arm was also associated with an increase in NEI VFQ-39 subscale scores after 1 year post-treatment as given in Table 3. For each subscale of the three categories the mean postoperative QOL score was higher than the mean subscale score at baseline. Especially for the second category, including the important quality of vision subscales like general vision (p < 0.01), difficulty with distance tasks (p = 0.03), difficulty with near tasks (p = 0.02), and peripheral vision (p = 0.04), which showed a significant increase in the scores 1 year after surgery and were significantly correlated with the improvement in VA (general vision p = 0.03, difficulty with distance tasks p = 0.01, difficulty with near tasks p = 0.02, peripheral vision p < 0.01) (Table 4).
A similar change in the scores was also observed for the subject’s vision-specific QOL subscales including dependency, role difficulties, mental health and social function, in which improvement of the scores could be detected for each subscale. However, the improvement was only significant for the subscale mental health despite surgery (p < 0.01) and significantly linked with the increase in VA (p < 0.01). The first category with the subscale general health showed only a slight increase in the score after surgery, which was also significantly correlated with the increase in VA (p = 0.02).
Differing from the FMT arm, QOL scores of the PDT arm did not demonstrate a permanent increase for all subscales after 1 year, similar to the VA outcome.
For the first category, the subscale general health, a small increase in the score could be detected similar to the FMT group. However, for the subscales of the second category (quality of a subject’s vision) only a slight increase in the scores was observed including difficulty with distance tasks, difficulty with near tasks and peripheral vision. The improvement of the subscale general vision was more pronounced. However, for all subscales the differences were not significant as well as for the decrease in the colour vision subscale score after 1 year. These incongruent results bear resemblance to the outcome of the third category, which assesses the subject’s vision-specific QOL. A non-significant increase in the QOL scores was only seen in the PDT group for the subscale mental health. For the other subscales only a slight decrease in the scores could be observed including the subscales dependency, role difficulties, social function and ocular pain. The difference did not admittedly reach the level of significance.
Comparing the results of the QOL scores between the FMT and the PDT after 1 year, the improvement of the subscale scores general vision (p = 0.03, Table 4), mental health (p = 0.02) and dependency (p = 0.03) was significantly higher in the FMT group. However, the higher gain of the QOL scores in the FMT group compared to the PDT is contradictory to the higher frequency of complications after undergoing the FMT. Within the 12-month follow-up period, 16 of the 25 patients (64%) enrolled in the FMT group received two and the remaining nine patients (36%) more than two intraocular interventions due to surgery-related complications. However, an increase in the subscale score ocular pain was not observed after 1 year compared to baseline before surgery (p = 0.37). In the PDT arm only one patient developed a severe complication related to the photodynamic therapy showing a retinal pigment epithelial tear after the first treatment.
In the FMT group diplopia was noted in five patients, in which the diplopia was intermittent and tolerated well in four patients. Eight patients had tilted vision. Two of them were free of the symptom after adoption of prismatic glasses and the remaining five patients felt the tilted vision not disturbing. One patient developed compensatory head position. A summarisation of the treatment related complications have been recently published in detail [11].
Discussion
In our study it was conspicuous that the vision-related QOL at baseline showed low scores for each subscale in both treatment groups. However, these findings are in accordance with the evaluated data of QOL in similar populations affected by severe bilateral AMD or low vision [12, 18].
Vision-related QOL as measured by the NEI VFQ-39 improved particularly in the FMT arm. An increase in the QOL scores was detected in all subscales after 1 year post-treatment. A significant improvement could be verified for the subscales difficulty with distance tasks, difficulty with near tasks, peripheral vision, mental health, and for the important quality of vision subscale general vision. Contrary to the results in the FMT arm, only a stabilisation of the QOL subscale scores could be detected in the PDT arm. Additionally, in the FMT arm the improvement of the subscale scores for general vision, mental health and dependency was significantly superior to the same subscale scores obtained 1 year after undergoing PDT.
The more pronounced increase in the FMT scores was correlated with a more intense improvement of VA than was observed for the PDT. This confirms a previous report that the NEI VFQ-39 QOL survey is sensitive to changes of the visual acuity over a 1 year period [19].
However, after 1 year post-treatment the increase in the QOL scores did not show the distinct extent, which would be assumed to result from the intriguing results of VA after FMT, and higher QOL scores have to be expected. Although VA is an objective measurement of visual function, the NEI VFQ-39 is a subjective assessment by patient’s perception of visual function. Other factors potentially influence the results of the QOL scores and the lower scores as expected could originate from the more frequent onset of complications after undergoing the FMT compared to the number of complications after PDT.
It is known that the FMT procedure can cause strabismus and torsion of the eye, and the subsequent muscle surgery, though relieving torsion, leads to some limitations in eye movement. In contrast to the adverse events described after FMT, subscale ocular pain showed only a slight increase. The absence of significant changes in the ocular pain subscale score 1 year after surgery reflects that FMT is not associated with sustained ocular disturbances.
Although the onset of adverse events was much lower after PDT, the patients in our study had only a small benefit after PDT, similar to recently published studies [8, 9]. An improvement was observed for the subscales general vision, difficulty with distance tasks, difficulty with near tasks and peripheral vision. However, the increase in the QOL scores was not as distinctive as it was seen in the FMT arm.
Therefore, according to our results, PDT exhibits to be a therapy which on the one hand induces a stabilisation of VA resulting in a limited improvement of patient’s QOL, but on the other hand has a low number of complications.
The FMT seems to be a therapeutic approach which can lead to an increase in VA resulting in a more pronounced improvement of patient’s QOL compared to the PDT, but exhibits a higher number of severe complications. The postoperative absence of binocular function and residual tilted vision may partially explain why the QOL scores are lower than expected. However, it could be shown that the improvement in vision-related QOL was not associated with an improvement in general health, but rather associated with an increase in VA. The results are in accordance with another study showing that FMT can significantly improve the QOL of patients with severe wet AMD [10]. FMT is associated with an improvement in vision-related QOL and the amount was greatest in patients with postoperative benefit of visual function.
Therefore, FMT seems to be an effective alternative treatment for patients with severe vision loss resulting from neovascular AMD, although an intraocular anti-vascular endothelial growth factor therapy with pegaptanib, avastin and ranibizumab is now available. The anti-vascular endothelial growth factor therapy for neovascular AMD provided promising results. Currently, the anti-vascular growth factor application seems to be the primary choice in the treatment of neovascular AMD [20]. FMT and PDT can be considered as effective alternative treatments for patients who did not respond to the anti-vascular growth factor therapy or developed complications thereafter. The information of the quality of life after FMT and PDT will help ophthalmologists and patients in decision making of alternative therapies in neovascular AMD.
However, at the moment it is not clear whether the improvement in VA after an anti-vascular endothelial growth factor therapy is inevitably associated with an amelioration of vision-related QOL. It is also supposable that the essential repetitive intraocular application will not be accepted by all of the patients. A negative influence on vision-related QOL linked to the surgical procedure and its complications seems reasonable.
The present study showed that FMT and PDT can prevent functional impairment and achieve at least a stabilisation of vision-related QOL in patients with neovascular AMD. The FMT seems to be more than an equitable alternative in the treatment of neovascular AMD. However, the discrepancy between the amount of patients with increased VA and simultaneous observation of a moderate improvement in QOL might be caused by the onset of complications following FMT.
References
Klein R, Klein BE, Linton KL (1992) Prevalence of age-related maculopathy. The beaver dam eye study. Ophthalmology 99:933–943
Treatment of Age-related Macular Degeneration with Photodynamic Therapy Study Group (1999) Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials—TAP report 1. Arch Ophthalmol 117:1329–1345
Treatment of Age-related Macular Degeneration with Photodynamic Therapy Study Group (2001) Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: two-year results of 2 randomized clinical trials—TAP report 2. Arch Ophthalmol 119:198–207
Treatment of Age-related Macular Degeneration with Photodynamic Therapy Study Group (2002) Verteporfin therapy for subfoveal choroidal neovascularization in age-related macular degeneration: three-year results of an open-label extension of 2 randomized clinical trials—TAP report no. 5. Arch Ophthalmol 120:1307–1314
American Academy of Ophthalmology (2000) Macular translocation. Ophthalmology 107:1015–1018
Abdel-Meguid A, Lappas A, Hartmann K, Auer F, Schrage N, Thumann G, Kirchhof B (2003) One year follow up of macular translocation with 360 degree retinotomy in patients with age related macular degeneration. Br J Ophthalmol 87:615–621
Mruthyunjaya P, Stinnett SS, Toth CA (2004) Change in visual function after macular translocation with 360° retinectomy for neovascular age-related macular degeneration. Ophthalmology 111:1715–1724
Hewitt AW, Jeganathan SV, Kidd JE, Pesudovs K, Verma N (2006) Influence of photodynamic therapy for age related macular degeneration upon subjective vision related quality of life. Graefes Arch Clin Exp Ophthalmol 244(8):972–977
Armbrecht AM, Aspinall PA, Dhillon B (2004) A prospective study of visual function and quality of life following PDT in patients with wet age related macular degeneration. Br J Ophthalmol 88:1270–1273
Cahill MT, Stinnett SS, Banks AD, Freedman SF, Toth CA (2005) Quality of life after macular translocation with 360° peripheral retinectomy for age-related macular degeneration. Ophthalmology 112:144–151
Gelisken F, Voelker M, Schwabe R, Besch D, Aisenbrey S, Szurman P, Grisanti S, Herzau V, Bartz-Schmidt KU (2007) Full macular translocation versus photodynamic therapy with verteporfin in treatment of neovascular age-related macular degeneration: 1 year results of a prospective, controlled, randomised pilot- trial (FMT-PDT). Graefes Arch Clin Exp Ophthalmol [OnlineFirst 12 January 2007]
Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD, National Eye Visual Function Questionnaire Field Test Investigators (2001) Development of the 25-item national eye institute visual function questionnaire. Arch Ophthalmol 119:1050–1058
Stelmack JA, Stelmack TR, Massof RW (2002) Measuring low-vision rehabilitation outcomes with the NEI VFQ-25. Invest Ophthalmol Vis Sci 43:2859–2868
Clemons TE, Chew EY, Bressler SB, McBee W for the AREDS Research Group (2003) National eye institute visual function questionnaire in the age-related eye disease study (AREDS). Arch Ophthalmol 121:211–217
Mangione CM, Berry S, Spritzer K (1998) Identifying the content area for the 51-item national eye institute visual function questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol 116:227–233
Franke GH, Esser J, Voigtländer A, Mähner N (1998) Der National Eye Institute Visual Function Questionnaire (NEI-VFQ) — Erste Ergebnisse zur psychometrischen Überprüfung eines Verfahrens zur Erfassung der Lebensqualität bei Sehbeein- trächtigten. Z Med Psychol 7:178–184
Mangione CM (2000) The NEI VFQ-25 scoring algorithm. http://catalog.nei.nih.gov/productcart/pc/viewPrd.asp?idcategory=50&idproduct=60#). Cited 26 February 2007
Cahill MT, Banks AD, Stinnett SS, Toth CA (2005) Vision-related quality of life in patients with bilateral severe age-related macular degeneration. Ophthalmology 112(1):152–158
The Submacular Surgery Trials Research Group (2003) Responsiveness of the national eye institute visual function questionnaire to changes in visual acuity. Findings in patients with subfoveal choroidal neovascularization — SST report no. 1. Arch Ophthalmol 121:531–539
Michels S, Schmidt-Erfurth U, Rosenfeld PJ (2006) Promising new treatments for neovascular age-related macular degeneration. Expert Opin Investig Drugs 15(7):779–793
Author information
Authors and Affiliations
Corresponding author
Additional information
Matthias Lüke and Focke Ziemssen contributed equally to the manuscript. The authors have no competing interests related to the manuscript.
Rights and permissions
About this article
Cite this article
Lüke, M., Ziemssen, F., Bartz-Schmidt, K.U. et al. Quality of life in a prospective, randomised pilot-trial of photodynamic therapy versus full macular translocation in treatment of neovascular age-related macular degeneration — a report of 1 year results. Graefes Arch Clin Exp Ophthalmol 245, 1831–1836 (2007). https://doi.org/10.1007/s00417-007-0558-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-007-0558-9