Abstract
Background
Accompanying the patient recruitment within the “Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment multicentre trial (SPR)”, all patients with primary rhegmatogenous retinal detachment (RRD) had to be documented in a detailed recruitment list. The main goal of this analysis was to estimate the prevalence of “medium-severe” RRD (SPR Study eligible) as defined by the SPR Study inclusion criteria. In addition, the detailed anatomical situation of medium-severe RRD is investigated.
Methods
SPR Study recruitment was evaluated via a standardised questionnaire, which contained a coloured fundus drawing and information regarding possible reasons for exclusion from the SPR Study in each case. A team of three experienced vitreoretinal surgeons evaluated all fundus drawings from a 1-year period. The review led to a decision on SPR Study eligibility on the pure basis of anatomical assessment. The main outcome measures were assessment of feasible inclusion into the SPR Study by the evaluation team based on the fundus drawing and anatomical details.
Results
A total of 1,115 patients with RRD from 13 European centres were prospectively enrolled in the year 2000. The quality of the drawings sufficed for assessment in 1,107 cases (99.3%). Three hundred and twelve fundus drawings (28.2%) met the anatomic inclusion criteria of the SPR Study. RRD of medium severity is characterised by an average number of 2.6 (SD 2.4) retinal breaks, 5.8 (SD 2.8) clock hours of detached retina, unclear hole situation in 15.1% of cases (n=47), attached macula in 42.9% (n=134), bullous detachment in 15.1% (n=47) and vitreous haemorrhage/opacity in 7.7% (n=24).
Conclusions
In the recruitment lists of the SPR Study of the year 2000, RRD of medium severity was present in nearly one third of the patients with primary RRD. These findings emphasise the clinical relevance of the SPR Study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The treatment of patients with primary rhegmatogenous retinal detachment (RRD) has undergone considerable change over recent decades. In Europe, there is a definite trend towards primary pars plana vitrectomy (PPPV) as the method of first choice [4, 7, 16, 20–23, 29]. However, in most European centres, scleral buckling surgery (SBS) remains the method of choice in uncomplicated retinal situations, i.e. single breaks and/or a limited retinal detachment. In contrast, PPPV is indicated in complicated situations, i.e. vitreous haemorrhage/opacity, proliferative vitreoretinopathy (PVR), or breaks at the posterior pole [3, 5, 8–11, 25, 28, 31, 35].
Despite these clear indications, there is a large group of RRDs with “medium severity” where the choice of treatment method is not clear-cut. The “Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR Study)”, a prospective, randomised multicentre clinical trial [12], addresses the question of whether SBS or PPPV are associated with a better functional and anatomical outcome in treating such medium-severe RRDs.
As part of the SPR Study, recruitment lists were employed to evaluate the strength of the eligibility criteria and to record epidemiological data. In this study, we analysed the data of the recruitment lists from a 1-year period. The goals of this evaluation are to estimate the prevalence of medium-severe RRDs as defined by the SPR Study inclusion criteria and to characterise the medium-severe RRDs in terms of anatomical details.
Methods
The SPR Study inclusion criteria
Medium-severe RRD as defined by the SPR Study inclusion criteria [12] is characterised as primary RRD not treatable with a single 7.5×2.75 mm Silastic sponge. This includes aphakic/pseudophakic patients with an unclear hole situation.
Basic data provided by study centres (from questionnaire)
All patients suffering from primary RRD had to be documented prospectively by the actively participating study centres using a standardised questionnaire. The recruitment lists of a 1-year period, the year 2000, were evaluated in this analysis (termed “SPR recruitment study”). The forms contained a coloured fundus drawing and retrieved information regarding possible reasons for exclusion from the SPR Study, the choice of the surgical procedure “(to be) performed” and the hole situation. Details are given in Table 1. Patients suffering from RRD following previous intraocular surgery (except uncomplicated cataract surgery), angioproliferative retinal diseases, re-detachment or penetrating injury were excluded from this analysis.
Reviewers’ evaluation (from the drawing)
Potential inclusion into the SPR Study was evaluated by review of the fundus drawings. Lens status was taken into account regarding the eligibility of pseudo-/aphakic patients with unclear hole situation (Fig. 1).
Examples for retinal break evaluation a Break size: I=smaller than 1/2 clock hour; II=1/2 to 1 clock hour; III=more than 1 clock hour. b Location of retinal break. I=anterior; II=intermediate; III=central; IV=macular hole. c Shape of retinal break: I=round; II=horseshoe; III=cleft; IV=unusual. d Traction on the operculum
Three experienced vitreoretinal surgeons (S.W., H.H., N.F.) independently evaluated all drawings. In cases in which the reviewers’ results differed, a majority vote (2:1) was accepted. Questionable situations and indeterminate cases were discussed and a consensus was reached. None of the additional information on the recruitment questionnaire was used to decide on potential inclusion into or exclusion from the SPR Study. The questions the reviewers had to answer are depicted in Table 2.
Statistics and ethics
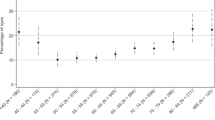
Statistical analysis was performed using SAS (the SAS System, Release 9.1.3 SP 2; SAS Institute, Cary, NC, USA) on Windows® 2000 SP 4 (Microsoft, Redmond, CA, USA). Values are given as frequency and percentage for qualitative, and mean and standard deviation for quantitative parameters respectively. Exact 95%-confidence intervals were calculated using SAS PROC FREQ (exact BINOMIAL) for the rates of medium-severe RRD.
The Ethics Committee approval of each participating centre was obtained.
Results
Basic data
The following 13 centres provided a total of 1115 cases with fundus drawings for the recruitment list in the year 2000 (in alphabetical order): Aachen, Berlin, Bremen, Cologne, Frankfurt, Freiburg, Heidelberg, Homburg, Leipzig, Liverpool, Lübeck, Regensburg, Sulzbach. The number of patients screened per centre ranged from 7 (0.6%) to 258 (23.1%) (mean 85.8, SD 73). Seventy-two of these patients (6.5%) were included in the SPR Study within the year 2000 (Fig. 2).
Five hundred and nine (45.7%) patients were female, 597 (53.6%) were male; no information on gender was provided in 9 cases (0.8%). In 595 (53.4%) of all patients, the retina of the right eye was detached, in 520 cases (46.6%) the left eye was affected. Seven hundred and sixty patients (68.2%) were phakic, while 343 eyes (30.8%) were recorded as aphakic or pseudophakic; the lens status was missing in 12 cases (1.1%).
Myopia of more than − 7.0 dioptres was present in 143 eyes (12.8%), central retinal breaks in 49 (4.4%), PVR B/C in 140 (12.6%), other eye diseases in 248 (22.2%) and severe systemic diseases in 329 (29.5%). Ten patients (0.9%) were younger than 18 years and 2 patients (0.2%) were pregnant. Seventy-two patients (6.5%) were not willing to participate, and in 18 cases (1.6%) no study surgeon was available (multiple items could be stated positive).
Medium-severe RRD: prevalence and evaluation
The quality of the drawings sufficed for assessment in 1,107 cases (99.3%). In 8 drawings, no clear decision on SPR eligibility could be made because of unclear or non-standardised signs.
In assessing whether or not a fundus drawing fulfilled the inclusion criteria, the three reviewers agreed in 818 (73.4%) of all evaluated drawings. Two hundred and sixty-seven cases (24.0%) required 2:1 agreement, and 30 (2.7%) of those controversial cases had to be re-evaluated and put to a joint vote, thus allowing proper evaluation in 1107 patients.
Overall, a total of 312 cases (28.2%; 95% CI 25.6–30.9%) were voted to be eligible for SPR inclusion from the fundus drawing (Fig. 2). 249 (79.8%) of those 312 patients were excluded from SPR Study participation because of additional information given on the questionnaires (SPR Study exclusion criteria).
Anatomical characterisation in medium-severe RRD
Differences between medium-severe and all other RRDs are found in the frequency of PVR stage B/C, bullous RRD and the mean number of retinal breaks (Table 3).
Analysis of the hole situation revealed a total of 1864 retinal holes. The majority of those were small (less than 1/2 clock hour; n=1609, 86.3%), showed a horseshoe shape (n=1272, 68.2%) and exerted no significant traction on the flap (n=1840, 98.7%). The holes were mostly located anterior to the equator (n=1501/80.5%) and between 10 and 2 o’clock (n=1126, 60.4%).
Discussion
Since PPPV was established in 1971 by Machemer et al. [19], SBS and PPPV have been competing methods in treating retinal detachment. Numerous studies have been published recommending one of the two methods [1, 4, 13, 14, 20, 24, 26, 27, 29, 30, 32]. We could identify no consensus among several editorial comments on this issue [6, 15–18, 33, 34]. In Europe, SBS still seems to be the first choice in the majority of RRD cases, although there has been a definite trend towards PPPV in recent years [4, 7, 16, 20–23, 29]. Furthermore, there is a wide variety in the choice of operating method in comparable pre-operative situations. The SPR Study was initiated to establish an evidence-based approach to this problem and to investigate whether one of the two methods is superior in more complicated (medium-severe) RRD cases. To judge the value of the SPR Study results, one needs to know the frequency of medium-severe RRD as defined by the SPR inclusion criteria. To answer this question, we evaluated the SPR Study’s recruitment lists from a 1-year period. The main goal of this analysis is to estimate the prevalence of medium-severe RRD (SPR Study eligible) as defined by the SPR Study inclusion criteria. In addition, the detailed anatomical situation of medium-severe RRD is investigated.
Our results correspond well with the findings of other multicentre trials [2] (Table 4).
Evaluation and prevalence of medium-severe RRDs
Medium-severe RRD as defined by the SPR Study criteria is a frequent finding in patients with primary RRD. Nearly one-third (28%) of all drawings of RRD cases matched the inclusion criteria. Eighty per cent of those patients could not be included in the study because of pre-existing ophthalmological (other than primary RRD) or systemic diseases. However, those exclusion criteria would not influence a surgeon’s decision outside the context of a study.
As expected, the three reviewers’ evaluations of the fundus drawings were not always consistent. One-quarter of all drawings required a 2:1 decision on SPR eligibility, and only 2.7% had to be conferred upon together. It is obvious from these data that the surgeons differ in their clinical assessment of retinal detachment. The variation in evaluating the retinal situation and the eligibility of patients may show surgeon-based bias concerning the first method of choice for surgical repair, especially for complex RRD, resulting in the exclusion of eligible patients from the SPR Study.
Characterisation of the medium-severe RRDs
In addition to the clearly defined inclusion criteria for the SPR Study, one goal of the present study was to work out details to characterise the retinal situation of eyes assessed to have medium-severe RRD and to find retinal criteria to differentiate between medium-severe and other RRDs. Overall, the mean area of detached retina we observed was higher than that found in other studies (Table 4). However, the mean area of detached retina in the well-defined retinal situation of medium-severe RRD is only a little greater than in all other eyes of the present study and as such is no valid criterion for differentiating between medium-severe and non-medium-severe RRD. In contrast, the mean number of retinal holes in the SPR-possible group was higher. SPR-possible eyes had a mean number of 2.6 holes (SD 2.4), exceeding the overall mean by more than 1 (mean 1.7, SD 1.7). These findings were not surprising, as more than the half of all eyes not assessed to have an SPR-eligible situation from the drawing were simple RRDs and presented a “single sponge possible” situation with a mean of 1.6 (SD 1.3) retinal holes.
Unclear hole situation, macular attachment and vitreous haemorrhage/opacity were comparable in SPR-eligible patients and all others. Overall, the typical medium-severe RRD has more than 2 retinal holes and a mean area of detached retina of more than 5 clock hours.
In summary, the SPR recruitment study underlines that RRD of medium severity represents a large and therefore clinically relevant subgroup of RRD patients. Additionally, the recruitment list provides a valuable overview of patients with RRD.
We therefore believe that the SPR Study results are necessary to identify the adequate therapy in the routine management of patients with RRD.
References
Afrashi F, Erakgun T, Akkin C, Kaskaloglu M, Mentes J (2004) Conventional buckling surgery or primary vitrectomy with silicone oil tamponade in rhegmatogenous retinal detachment with multiple breaks. Graefes Arch Clin Exp Ophthalmol 242:295–300
Algvere PV, Jahnberg P, Textorius O (1999) The Swedish retinal detachment register. I. A database for epidemiological and clinical studies. Graefes Arch Clin Exp Ophthalmol 237:137–144
Ambresin A, Wolfensberger TJ, Bovey EH (2003) Management of giant retinal tears with vitrectomy, internal tamponade, and peripheral 360 degrees retinal photocoagulation. Retina 23:622–628
Barrie T, Kreissig I, Heimann H, Holz ER, Mieler WF (2003) Repair of a primary rhegmatogenous retinal detachment. Br J Ophthalmol 87:782
Bartz-Schmidt KU, Kirchhof B, Heimann K (1996) Primary vitrectomy for pseudophakic retinal detachment. Br J Ophthalmol 80:346–349
Bornfeld N (2001) Ablation surgery. From the inside, from the outside, or both? Ophthalmologe 98:879–880
Comer MB, Newman DK, George ND, Martin KR, Tom BD, Moore AT (2000) Who should manage primary retinal detachments? Eye 14:572–578
Duquesne N, Bonnet M, Adeleine P (1996) Preoperative vitreous hemorrhage associated with rhegmatogenous retinal detachment: a risk factor for postoperative proliferative vitreoretinopathy? [see comments]. Graefes Arch Clin Exp Ophthalmol 234:677–682
el-Asrar AM (1997) Primary vitrectomy for bullous rhegmatogenous retinal detachments due to complex breaks. Eur J Ophthalmol 7:322–326
Ghartey KN, Tolentino FI, Freeman HM, McMeel JW, Schepens CL, Aiello LM (1980) Closed vitreous surgery. XVII. Results and complications of pars plana vitrectomy. Arch Ophthalmol 98:1248–1252
Girard P, Karpouzas I (1995) Pseudophakic retinal detachment: anatomic and visual results. Graefes Arch Clin Exp Ophthalmol 233:324–330
Heimann H, Hellmich M, Bornfeld N, Bartz-Schmidt KU, Hilgers RD, Foerster MH (2001) Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment (SPR Study): design issues and implications. SPR Study report no. 1. Graefes Arch Clin Exp Ophthalmol 239:567–574
Holz ER, Mieler WF (2003) View 3: The case for pneumatic retinopexy. Br J Ophthalmol 87:787–789
Kreissig I (2003) View 1: minimal segmental buckling without drainage. Br J Ophthalmol 87:782–784
Laqua H (1983) Current concepts in the management of complex retinal detachments. Trans Ophthalmol Soc U K 103:133–138
Laqua H, Honnicke K (2001) Is scleral buckling still current? Ophthalmologe 98:881–885
Leaver P (1993) Expanding the role of vitrectomy in retinal reattachment surgery [editorial; comment]. Br J Ophthalmol 77:197
Leaver PK (1999) Trends in vitreoretinal surgery-time to stop and think [editorial; comment]. Br J Ophthalmol 83:385–386
Machemer R, Buettner H, Norton EW, Parel JM (1971) Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol 75:813–820
McLeod D (2004) Is it time to call time on the scleral buckle? Br J Ophthalmol 88:1357–1359
Miki D, Hida T, Hotta K, Shinoda K, Hirakata A (2001) Comparison of scleral buckling and vitrectomy for retinal detachment resulting from flap tears in superior quadrants. Jpn J Ophthalmol 45:187–191
Minihan M, Tanner V, Williamson TH (2001) Primary rhegmatogenous retinal detachment: 20 years of change. Br J Ophthalmol 85:546–548
Oshima Y, Yamanishi S, Sawa M, Motokura M, Harino S, Emi K (2000) Two-year follow-up study comparing primary vitrectomy with scleral buckling for macula-off rhegmatogenous retinal detachment. Jpn J Ophthalmol 44:538–549
Pournaras CJ, Kapetanios AD (2003) Primary vitrectomy for pseudophakic retinal detachment: a prospective non-randomised study. Eur J Ophthalmol 13:298–306
Richardson EC, Verma S, Green WT, Woon H, Chignell AH (2000) Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of failure. Eur J Ophthalmol 10:160–166
Schmidt JC, Rodrigues EB, Hoerle S, Meyer CH, Kroll P (2003) Primary vitrectomy in complicated rhegmatogenous retinal detachment—a survey of 205 eyes. Ophthalmologica 217:387–392
Schwartz SG, Kuhl DP, McPherson AR, Holz ER, Mieler WF (2002) Twenty-year follow-up for scleral buckling. Arch Ophthalmol 120:325–329
Spiegel D, Nasemann J, Nawrocki J, Gabel VP (1997) Severe ocular trauma managed with primary pars plana vitrectomy and silicone oil [see comments]. Retina 17:275–285
SPR Study goup (2003) View 2: the case for primary vitrectomy. Br J Ophthalmol 87:784–787
Tewari HK, Kedar S, Kumar A, Garg SP, Verma LK (2003) Comparison of scleral buckling with combined scleral buckling and pars plana vitrectomy in the management of rhegmatogenous retinal detachment with unseen retinal breaks. Clin Exp Ophthalmol 31:403–407
Wang JZ (1993) Vitreo-retinal surgery for complicated retinal detachment. Chung Hua Yen Ko Tsa Chih 29:205–207
Wickham L, Connor M, Aylward GW (2004) Vitrectomy and gas for inferior break retinal detachments: are the results comparable to vitrectomy, gas, and scleral buckle? Br J Ophthalmol 88:1376–1379
Wilkinson CP (1998) Wanted: optimal data regarding surgery for retinal detachment [editorial]. Retina 18:199–201
Wilkinson CP (1999) Discussion to “Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachment”. Ophthalmology 106:1816
Wong D, Billington BM, Chignell AH (1987) Pars plana vitrectomy for retinal detachment with unseen retinal holes. Graefes Arch Clin Exp Ophthalmol 225:269–271
Acknowledgements
The SPR Study was supported by - Deutsche Forschungsgesellschaft (DFG Number Fo 165/ 2–1 – 2–4; Le 842/ 3–1/2; Hi 541/ 2–1/2) - Stifterverband für die Deutsche Wissenschaft (Friedrich Spicker-Stiftung) Number S 050– 10.003/004–Retinologische Gesellschaft.
Participants
Principal clinical investigator: M.H. Foerster
Principal investigator medical statistics: D.-H. Hilgers
Study co-ordinator: C. Weiss
Surgeons and coworkers (alphabetical order): K.-U. Bartz-Schmidt, Binder, S. Bopp, N. Bornfeld, C. Dahlke, F. Faude, M.H. Foerster, W. Friedrichs, V.P. Gabel, J. Garweg, A. Gaudric, W. Göbel, S. Grisanti, C. Groenewald, L.L. Hansen, L. Hattenbach, K. Hille, H. Hoerauf, F. Holz, P. Janknecht, J. Jonas, U. Kellner, B. Kirchhof, F. Koch, F. Körner, H. Laqua, Y. LeMer, M. Loew, A. Lommatzsch, K. Lucke, P. Meier, E. Messmer, U. Mester, M. Partsch, D. Pauleikhoff, I. Pearce, J. Roider, H. Schilling, W. Schrader, N. Schrage, U. Stolba, P. Walter, B. Wiechens, S. Wolf, D. Wong.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This work was in part presented at the annual meeting of the Association for Research in Vision and Ophthalmology (ARVO), Fort Lauderdale, May 2005; at the Deutsche Retinologische Gesellschaft, Bern, June 2005; and at the Deutsche Ophthalmologische Gesellschaft /Societas Ophthalmologica Europaea, Berlin, September 2005.
Rights and permissions
About this article
Cite this article
Feltgen, N., Weiss, C., Wolf, S. et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR Study): recruitment list evaluation. Study report no. 2. Graefe's Arch Clin Exp Ophthalmol 245, 803–809 (2007). https://doi.org/10.1007/s00417-006-0399-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-006-0399-y