Abstract
Purpose
We describe a case of high myopia who developed paravascular retinal rarefaction generated by vitreoretinal adhesion on retinal vessels detected using optical coherence tomography (OCT).
Methods
A 31-year-old man received a regular ophthalmologic examination for high myopia including detailed fundus examination and OCT.
Results
Detailed fundus examination revealed retinal rarefaction and fissure-like findings alongside the superior temporal retinal artery and vein in the right eye. OCT images revealed vitreoretinal adhesions on the retinal artery and a paravascular cystoid space in the inner retina. There was no retinal detachment. The axial length had increased by 1.50 mm over 15 years.
Conclusion
Paravascular retinal rarefaction as well as pseudohole formation caused by vitreoretinal adhesion on retinal vessels was detected in this patient using OCT. OCT might be useful to detect early-stage retinal pathologies caused by paravascular vitreoretinal traction in highly myopic patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In eyes with high myopia, the posterior retina can be damaged by traction induced by residual focal vitreoretinal adhesions, in combination with the presence of posterior staphyloma and progressive global scleral stretching. This unique combination of vitreoretinal traction mixed with the complex anatomy of degenerative myopia is considered to be closely related to the pathogenesis of vitreoretinal diseases specific to myopia, such as paravascular microhole formation [8]. In a previous study of autopsy eyes, Spencer et al. [7]. stated that paravascular vitreoretinal attachments were manifest as paravascular retinal rarefaction before posterior vitreous detachment, and that retinal rarefaction was the precursor of paravascular full-thickness retinal tears. This study, however, was performed only on autopsy eyes [7], and we are unaware of any reports demonstrating asymptomatic retinal rarefaction along retinal vessels in human patients. Here, we demonstrate a case of high myopia that developed a paravascular retinal rarefaction generated by vitreoretinal adhesion on retinal vessels using optical coherence tomography (OCT) during a long-term periodic examination.
Case report
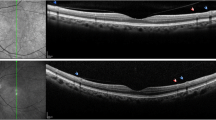
A 31-year-old man visited the Tokyo Medical and Dental University for a regular check-up of high myopia in both eyes on December 10, 2004. His visual acuity was 1.0 in both eyes. The refractive errors were −12.0 D (diopters) in the right eye and −10.75 D in the left, and the axial length measurements were 27.55 mm in the right eye and 27.51 mm in the left. He had no complaints of visual symptoms; however, a detailed fundus examination of the right eye revealed retinal rarefaction and fissure-like findings alongside the superior temporal retinal artery and vein (Fig. 1a,b). OCT images along the superior temporal retinal artery demonstrated vitreoretinal adhesions on the retinal artery and a paravascular cystoid space in the inner retina (Fig. 1c). There was no retinal detachment.
Ophthalmoscopy of the right eye. (a) Photograph at a 50° angle, (b) Photograph at a 35° angle. These photographs demonstrate retinal rarefaction and findings of multiple retinal fissures along the superior temporal retinal artery and vein. (c) Optical coherence tomography across the scan indicated as a black bar in Fig. 1b demonstrates vitreoretinal adhesion on the retinal artery and a paravascular retinal cyst in the inner retina
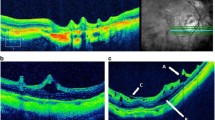
The follow-up time was 15 years since 1989 in our high myopia clinic. The review of the clinical records of this patient revealed that retinal rarefaction was not evident in a fundus photograph in 1989 (Fig. 2). The axial length of the right eye at that time was 26.05 mm, 1.50 mm less than that in 2004. Comparison of the fundus photographs from 1989 and 2004 (Figs 1, 2) indicated that in 2004 the superior temporal retinal vein had become tortuous and the superior temporal retinal artery and vein had separated. In his left fundus in 2004, the inferior temporal retinal vein became a little tortuous compared with the photograph in 1989; however, there was no retinal rarefaction in his left fundus throughout the follow-up period (figure not shown).
Discussion
Paravascular vitreoretinal traction occurs in highly myopic eyes and may cause paravascular retinal tears [4, 5, 7, 8]. Although autopsy studies have shown that paravascular retinal rarefaction is a precursor of paravascular retinal tears, we are unaware of any previous studies demonstrating this precursor lesion in human patients. OCT with cross-sectional images of retinal structure greatly facilitates the study of the posterior vitreoretinal anatomy in eyes with high myopia [1–3, 6]. In our patient, we observed the vitreous connected to the retinal vessel in OCT images, which indicates that the retinal cyst was caused by tight adherence to the vitreous. The cystic space adjacent to the blood vessel appeared to be situated in the inner retina on OCT analysis, supporting the previous histologic findings in autopsy eyes [7]. Vitreoretinal adhesion on the retinal vessels combined with progressive global scleral stretching appeared to contribute to the retinal rarefaction in this patient. During the 15-year follow-up period, the axial length increased by 1.50 mm, and the course of the retinal vein became tortuous, possibly due to increased vitreoretinal traction on the retinal vessels over 15 years. It is not yet clear whether the progressive vitreoretinal traction could eventually cause the development of full-thickness hole formation and retinal detachment in this patient, because these findings have never been reported.
Recently, Sayanagi and Ikuno [6] reported retinal microfold formation coincided with the location of retinal vessels in some highly myopic eyes using OCT. Taken together with our findings, retinal vascular or paravascular traction might not be uncommon in highly myopic patients. OCT examination is a useful tool to delineate such early-stage pathologies caused by paravascular vitreoretinal traction in highly myopic eyes.
References
Coppe AM, Ripandelli G (2003) Optical coherence tomography in the evaluation of vitreoretinal disorders of the macula in highly myopic eyes. Semin Ophthalmol 18:85–88
Ikuno Y, Gomi F, Tano Y (2005) Potent retinal arteriolar traction as a possible cause of myopic foveoschisis. Am J Ophthalmol 139:462–467
Panozzo G, Mercanti A (2004) Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol 122:1455–1460
Phillips CI, Dobbie JG (1963) Posterior staphyloma and retinal detachment. Am J Ophthalmol 55:332–335
Regenbogen L, Stein R (1968) Retinal detachments due to juxtapapillary microholes. Arch Ophthalmol 80:155–160
Sayanagi K, Ikuno Y, Gomi F, Tano Y (2005) Retinal vascular microfolds in highly myopic eyes. Am J Ophthalmol 139:658–663
Spencer LM, Foos RY (1970) Paravascular vitreoretinal attachments. Arch Ophthalmol 84:557–564
Stirpe M, Heimann K (1996) Vitreous changes and retinal detachment in highly myopic eyes. Eur J Ophthalmol 6:50–58
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohno-Matsui, K., Hayashi, K., Tokoro, T. et al. Detection of paravascular retinal cysts before using OCT in a highly myopic patient. Graefe's Arch Clin Exp Ophthalmo 244, 642–644 (2006). https://doi.org/10.1007/s00417-005-0112-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0112-6