Abstract
Purpose
To report the treatment outcome of photodynamic therapy with verteporfin (PDT) for exudative retinal detachment associated with diffuse choroidal haemangioma in Sturge–Weber syndrome.
Methods
An interventional case report of a 12-year-old girl with Sturge–Weber syndrome who developed an exudative retinal detachment (visual acuity 20/400) that was treated with PDT under general anaesthesia. PDT was performed according to the standard (macular degeneration) protocol, using three nonoverlapping spots of 4,000 μm.
Results
Subretinal fluid resolved completely over a period of 5 months and visual acuity increased to 20/50. No side effects of the PDT treatment were encountered during 9 months’ follow-up.
Conclusion
In our patient PDT with verteporfin effectively resolved the exudative retinal detachment associated with a diffuse choroidal haemangioma. Resolution of subretinal fluid occurred over several months without retreatment. We noted no side effects of the combination PDT and general anaesthesia, nor did we encounter ocular side effects of the treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Photodynamic therapy (PDT) has recently been described as a therapeutic option for exudative retinal detachment associated with diffuse choroidal haemangioma in Sturge–Weber syndrome [1, 3, 10]. Our case illustrates that disappearance of an exudative retinal detachment after PDT can take several months and it shows that PDT with verteporfin can be applied under general anaesthesia.
Case report
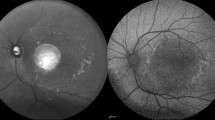
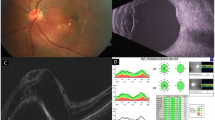
A 12-year-old girl with a history of right-sided Sturge–Weber syndrome, complicated by seizures and a concentration disorder, was monitored for glaucoma in our outpatient department. At age 10, a catsup red appearance with elevation of the retina became apparent superior and nasally in the right fundus (from 10 o’clock to 4 o’clock); centrally the lesion extended just inside the superior vascular arcades but did not include the fovea. In 2003 an exudative retinal detachment developed overlying the haemangioma with extension under the macula (Fig. 1a). Visual acuity decreased from 20/30 to 20/50. By February 2004 Snellen visual acuity had decreased to 20/400. Ultrasonography confirmed the presence of a diffuse choroidal haemangioma with an associated retinal detachment (Fig. 2a) and optical coherence tomography (OCT) showed subretinal fluid extending under the foveal depression (Fig. 3a). Fluorescence angiography could not be obtained because of the behavioural problems.
Ultrasonography showed a mass lesion with high internal reflectivity characteristic of a haemangioma. The haemangioma was associated with an exudative retinal detachment before PDT treatment (a). After treatment, ultrasonography showed a band of residual haemangioma. There was no evidence of remaining subretinal fluid (b)
The resolution of subretinal fluid after PDT with verteporfin for diffuse haemangioma took several months, as shown on OCT images (OCT 3, Zeiss, Jena). All images are taken from the fast macular image and are oriented horizontally (temporal to nasal). Subretinal fluid before treatment (thickness of fluid 125 μm) (a); 2 months after treatment (thickness of fluid 82 μm) (b); 4 months after treatment (no fluid) (c). Central macular thickness is reduced in c, probably due to previous subretinal fluid accumulation
PDT with verteporfin was performed according to the age-related macular degeneration protocol [11]. Our patient had to be treated under general anaesthesia because of her concentration disorder. General anaesthesia was achieved with propofol, remifentanil, rocuronium and endotracheal intubation. Verteporfin was administered via a separate intravenous line. The patient was positioned on her back with her face turned towards the laser. The headrest of the laser was removed to allow access to the eye while the patient was intubated. Laser treatment was performed with a Mainster Standard fundus lens using three separate nonoverlapping spots of 4,000 μm, 83 s each, at 11 o’clock, 1 o’clock and 3 o’clock, guided by ultrasonography and anatomic landmarks. This spot size was chosen to allow for optimal visualisation . The eye was manoeuvred into position by an assistant using a forceps. To prevent pigment epithelial alterations in the macular area, the spots were placed outside the vascular arcades. Four weeks after PDT visual acuity had decreased to counting fingers. Follow-up visits showed a slow resolution of subretinal fluid (Fig. 3b) and an increase in visual acuity. After 5 months visual acuity had increased to 20/50. Ophthalmoscopy showed a complete resolution of the retinal detachment. This was also apparent on ultrasonography (Fig. 2b) and OCT (Fig. 3c). In the area of the laser spots no clinically apparent pigment epithelial alteration occurred compared to the pretreatment state and the elevation caused by the haemangioma decreased(Fig. 1b). However there was still a small band of haemangioma in the area of the superior vascular arcade, which was also detected on ultrasonography (Fig. 2b).
Discussion
Histopathological evidence indicates that diffuse choroidal haemangiomas occur in about 40% of Sturge–Weber patients [5]. Mostly symptoms are mild and the haemangioma remains undetected. Vision-threatening complications are exudative retinal detachment and amblyopia. Three recently published reports indicate that PDT with verteporfin can be used as a therapeutic option for exudative retinal detachment associated with diffuse choroidal haemangioma [1, 3, 10]. Results show an effective resolution of subretinal fluid, and in these case studies no side effects apart from residual pigment epithelium mottling were reported.
Other therapeutic options for choroidal haemangioma include argon laser photocoagulation, transpupillary thermotherapy (TTT), ruthenium plaque therapy, external beam irradiation and proton-beam irradiation [2, 6–8]. Argon laser photocoagulation applied in a grid-like pattern does not reduce tumour size, and as a consequence there are frequent recurrences of subretinal fluid [2]. TTT has been shown to reduce haemangioma size; however, retreatments are often needed [6, 7]. Ruthenium plaque therapy and external beam irradiation are frequently complicated by scarring in the posterior pole and cataract formation [8]. Proton-beam irradiation applied at a high dose entails the risk of radiation retinopathy, radiation optic neuropathy and cataract. Lowering the dosage to 16.4–18.2 Gy minimises these complications; however, in an earlier study it was shown that at these dosages regression of the haemangioma takes up to 2 years [12].
As initial published results of PDT therapy in Sturge–Weber syndrome were favourable and PDT is associated with few systemic or ocular complications compared to the other treatment options, PDT was chosen as a first-line therapy [11]. At this moment no recurring accumulation of subretinal fluid associated with haemangioma in Sturge–Weber syndrome has been reported; however, the follow-up period remains short. Therefore the possibility of retreatment has to be taken into account. Although we did not encounter any side effects of the PDT treatment in our case, macular pigment alterations after PDT have been described. This means that especially in a young patient, who may need retreatment in the future, these possible PDT side effects should be taken into account [3, 4, 9]. We have tried to avoid damage to the pigment epithelium in the macula by placing the treatment spots outside the vascular arcade. As a consequence a small remaining band of haemangioma is still present in the area of the superior vascular arcade (Fig. 2b). In the treated area we have not detected any clinically apparent alteration in pigmentation compared to the pretreatment situation (Fig. 1a, b).
The cost of a single PDT treatment is significantly higher than either argon laser photocoagulation or TTT. The costs of PDT treatment will depend largely on the number of treatments that are required in each patient. Reports with long-term follow-up must show whether and how frequent PDT retreatments are required. Longer-term follow-up studies will provide a better insight to the difference in cost–benefit ratios between various treatments.
Our patient could not be treated without general anaesthesia because of her concentration disorder. Therefore PDT was performed under general anaesthesia. To our knowledge this is the first report of a PDT treatment with verteporfin under general anaesthesia. Several preclinical animal studies warned of a severe hypotensive reaction when administering verteporfin in high doses under general anaesthesia. Treatment options were discussed with the patient and her parents and they gave their informed consent for the treatment.
Apart from darkening of the operating room and recovery, general anaesthesia was given in a standard protocol. No problems occurred with either PDT or anaesthesia, which indicates that general anaesthesia is not a contraindication for PDT with verteporfin.
Like the earlier cases, our patient shows a resolution of subretinal fluid and increase in visual acuity occurring gradually over a 4- to 5-month period. No retreatment was applied in any of these published reports, which shows that early retreatment is not necessary if subretinal fluid does not disappear promptly.
Our experience in this case confirms that PDT with verteporfin is a therapeutic option for exudative retinal detachment associated with diffuse choroidal haemangioma. Retreatment should not be performed too early as resolution of subretinal fluid can take several months. Furthermore, we did not encounter any side effects of the combination of PDT with verteporfin and general anaesthesia.
References
Anand R (2003) Photodynamic therapy for diffuse choroidal haemangioma associated with Sturge Weber syndrome. Am J Ophthalmol 136:758–760
Anand R, Augsburger JJ, Shields JA (1989) Circumscribed choroidal hemangiomas. Arch Ophthalmol 1107:1338–1342
Bains HS, Cirino AC, Ticho BH, Jampol LM (2004) Photodynamic therapy using verteporfin for a diffuse choroidal haemangioma in Sturge–Weber syndrome. Retina 24:152–155
Farah ME, Costa RA, Muccioli C, Guia TA, Belfort R Jr (2002) Photodynamic therapy with verteporfin for subfoveal choroidal neovascularization in Vogt–Koyanagi–Harada syndrome. Am J Ophthalmol 134:137–139
Ferry AP (2001) Other phakomatoses. In: Schachat AP (ed) Retina, vol 1, 3rd edn. St. Louis, Mosby, pp 596–600
Fuchs AV, Mueller AJ, Grueterich M, Ulbig MW (2002) Transpupillary thermotherapy (TTT) in circumscribed choroidal hemangioma. Graefes Arch Clin Exp Ophthalmol 240:7–11
García-Arumí J, Ramsay LS, Guraya BC (2000) Transpupillary thermotherapy for circumscribed choroidal hemangiomas. Ophthalmology 107:351–357
Gragoudas ES, Li W, Lane AM, Munzenrider J, Egan KM (1999) Risk factors for radiation maculopathy and papillopathy after ocular irradiation. Ophthalmology 106:1571–1578
Postelmans L, Pasteels B, Coquelet P, El Ouardighi H, Verougstraete C, Schmidt-Erfurth U (2004) Severe pigment epithelial alterations in the treatment area following photodynamic therapy for classic choroidal neovascularization in young females. Am J Ophthalmol 138:803–808
Singh AD, Rundle PA, Vardy SJ, Rennie IG (2004) Photodynamic therapy of choroidal haemangioma associated with Sturge–Weber syndrome. Eye DOI:10.1038/sj.eye.6701474
Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group (1999) Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials—TAP Report. Arch Ophthalmol 117:1329–1345
Zografos L, Egger E, Bercher L, Chamot L, Munkel G (1998) Proton beam irradiation of choroidal hemangiomas. Am J Ophthalmol 126:261–268
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huiskamp, E.A., Müskens, R.P.H.M., Ballast, A. et al. Diffuse choroidal haemangioma in Sturge–Weber syndrome treated with photodynamic therapy under general anaesthesia. Graefe's Arch Clin Exp Ophthalmol 243, 727–730 (2005). https://doi.org/10.1007/s00417-004-1102-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-004-1102-9