Abstract
Purpose
To investigate the effect of retrobulbar anaesthesia on retrobulbar haemodynamics, colour Doppler imaging was performed. Furthermore, the additive effect of epinephrine was examined.
Method
Forty-one patients (age 72.7±8.9; 22 f, 19 m) undergoing planned cataract surgery were included in a prospective study. Colour Doppler imaging was performed before and directly after retrobulbar anaesthesia and after cataract surgery to measure the peak systolic velocity (PSV) and end-diastolic velocity (EDV) in the ophthalmic artery, central retinal artery and central retinal vein. In 18 patients lidocaine 2% without additives (2 ml, retrobulbar transconjunctival injection) and in 23 patients lidocaine 2% with epinephrine 1:200,000 was used.
Results
After retrobulbar anaesthesia both groups had a significant reduction of the PSV and of the EDV. After surgery flow velocities increased again. The addition of epinephrine resulted in a significantly greater reduction and slower recovery of flow velocities.
Conclusion
Retrobulbar anaesthesia induces a marked reduction of velocity in the retrobulbar vessels. The supplement epinephrine increases this effect, and recovery is much slower. Thus, particularly in patients with already disturbed ocular haemodynamics epinephrine should not be used in order to avoid irreversible functional damage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Different types of anaesthesia techniques for cataract surgery are common. In the eighties retrobulbar anaesthesia was, at 85%, the most common form used for anaesthesia [14]. Although drop anaesthesia is becoming more and more attractive, retrobulbar anaesthesia is still employed in patients with high motility of the eye and in cases expected to be difficult. Different local anaesthetic drugs and different drug supplements like epinephrine are used. The vasoconstrictive effect of epinephrine is utilised in retrobulbar anaesthesia to slow absorption of the anaesthetic in general circulation and thus to achieve a longer effect in the orbit. However, the effect of different local anaesthetic procedures, local anaesthetics and drug supplements on ocular blood flow is not clear.
Complications beside penetration of the needle in the globe following local anaesthesia are ischaemic optic neuropathy [1, 7, 20] occlusion of the central retinal artery [12] and retinal [4] or outer retinal ischaemic infarction [19]. This implies that there is a vascular change after local anaesthesia and the complication risk differs by local anaesthetic technique and drug supplement, and vascular risk factors of the patients.
Previous studies with different techniques assessed the influence of retrobulbar anaesthesia. The pulsatile ocular blood flow decreased markedly after retrobulbar anaesthesia with and without epinephrine [11]. The recovery of the pulsatile ocular blood flow after retrobulbar anaesthesia was very slow [2]. Recent examinations by colour Doppler imaging (CDI) in monkeys showed that retrobulbar anaesthesia with lidocaine and epinephrine significantly reduced the retrobulbar haemodynamics in the central retinal artery and the posterior ciliary arteries [18].
CDI is a non-invasive ultrasound technique that combines B-scan grey-scale imaging of the tissue structure, coloured representation of blood flow based on Doppler-shifted frequencies and pulsed-Doppler measurement of blood flow velocities. CDI can give data on flow velocities of retrobulbar blood vessels and vascular downstream resistance. A variety of occlusion diseases of the eye and the orbit have been examined by CDI. CDI is also used in a wide range of other diseases of the eye in which vascular aetiology has been implicated, e.g. glaucoma [3, 6, 15, 23].
In this study CDI was performed to quantify the effect of retrobulbar anaesthesia on retrobulbar haemodynamics. Furthermore, the additive effect of the drug supplement epinephrine was examined.
Material and methods
Patients
In this prospective study 41 patients scheduled for cataract surgery (small incision, phako with IOL implantation) were recruited. Eyes with a refractive error greater than 4 dioptres and eyes with an axial length less than 21 mm or more than 25.5 mm were excluded. Exclusion criteria were the presence of systemic diseases affecting ocular circulation, e.g. arterial hypertension or diabetes mellitus. Furthermore, patients with vascular occlusion in the studied or in the second eye were excluded. The patients with systemic intake of vaso-active medication, e.g. aspirin, were also excluded.
Twenty-three of the patients (age 71±8 years; 14 men, 9 women) underwent retrobulbar anaesthesia with 2 ml lidocaine (Xylocaine) 2% and epinephrine (1:200,000). The other 18 patients (age 75±9 years; 5 men, 13 women), selected randomly, had retrobulbar anaesthesia with 2 ml lidocaine 2% without epinephrine supplement. For safety reasons the surgeon was not blinded to the content of the retrobulbar injection. The data of both groups are shown in Table 1.
Informed consent was obtained from each subject including detailed explanation of all procedures before participation in the study. The study adhered to the tenets of the Helsinki declaration.
Method
Measurements of retrobulbar velocity were performed using a CDI device (Sonoline Sienna; Siemens, Germany) in a standardised manner [5]. The scan was performed with the patient in supine position with eyes closed and directed to gaze towards the ceiling. A 7.5-MHz linear phased-array transducer was applied with contact jelly on the upper eyelid while the examiner’s hand rested upon the orbital margin to minimise the pressure on the globe. All examinations were performed by one experienced examiner (K.K.H.). A 0.2 mm by 0.2 mm Doppler sample window was used to perform the measurements of the ophthalmic artery, the central retinal artery and the central retinal vein. Peak systolic velocities (PSV) and end-diastolic velocities (EDV) were obtained from the velocity waveforms of each artery. The resistive index (RI) known as Pourcelot’s ratio was measured. This parameter of downstream resistance was calculated by the formula (PSV − EDV)/(PSV) to characterise peripheral vascular resistive of the vessels studied [5].
In this study CDI was carried out before and directly after retrobulbar anaesthesia and after completion of cataract surgery. Furthermore, the cardiovascular parameters systolic and diastolic blood pressure and pulse were measured simultaneously. Cataract surgery was performed by one surgeon (A.R.) with a close-to-cornea 2.8-mm incision and phakoemulsification with implantation of a hydrophobic foldable intraocular lens (Acrysof; Alcon, Fort Worth, USA).
Statistical analysis
The statistical analysis was performed using analysis of variance (ANOVA) as computed with Statview (SAS Institute, Cary, NC, USA). A repeated-measures ANOVA was used for testing the interaction of added supplements.
For post hoc testing, calculations with Fisher’s protected least significant difference were carried out. Findings of probability of a type error less than 0.05 were considered to be statistically significant. For the comparison of discrete variables, a Chi-square test was calculated for each contingency table.
Results
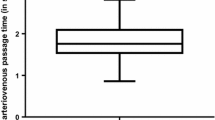
After retrobulbar anaesthesia both groups had a significant reduction in PSV and EDV for all measured vessels. For the ophthalmic artery the PSV decreased by 34% and the EDV by 27%. In the central retinal artery the PSV decreased by 26% and the EDV by 23%. In the central retinal vein there was a reduction of the PSV by 30% and of the EDV by 26%. After surgery, flow velocities increased again. In the ophthalmic artery the PSV increased by 26% and the EDV by 40%. In the central retinal artery the velocities increased by 19% for the PSV and by 22% for the EDV (p<0.0001). The PSV of the central retinal vein increased by 20% and the EDV by 23%. The RI in all vessels remained unchanged after retrobulbar anaesthesia and after surgery for both groups. Furthermore, axial length had no influence on retrobulbar haemodynamics.
Subgroup analysis revealed that the eyes treated with epinephrine had a significantly greater reduction in velocity after retrobulbar anaesthesia. Exact means and standard deviations of the velocities as shown by CDI (cm/s) are presented in Table 2.
ANOVA statistics (Tables 2, 3) showed that the addition of epinephrine resulted in significantly greater reductions and slower recovery of the PSV in the ophthalmic artery (p<0.0004) and central retinal artery (p<0.0001). Furthermore, the EDV of the ophthalmic artery (p=0.0014), the central retinal artery (p=0.0335) and the central retinal vein (p<0.0355) decreased more and recovered more slowly in the group with added epinephrine (Figs. 1, 2, 3).
Cardiovascular parameters in both groups were significantly different before and after surgery with regard to the systolic (p<0.005) and diastolic (p<0.0177) blood pressures. The mean arterial blood pressure (p<0.0404) and the heart rate (p<0.0154) also differed significantly before and after surgery (Tables 4, 5). The patients treated with epinephrine supplement showed no difference in cardiovascular parameters from those without epinephrine.
Discussion
In this study we found a reduction in retrobulbar blood flow velocities after retrobulbar anaesthesia. The velocities recovered only slowly and were still below baseline after surgery. These findings confirm previous reports on the influence of retrobulbar anaesthesia on ocular blood flow. Hulbert et al. [11] found a marked decrease in the pulsatile ocular blood flow after retrobulbar anaesthesia with and without epinephrine.
Several factors may account for the dramatic reduction in blood flow velocity after retrobulbar anaesthesia. First, there is mechanical compression of the retrobulbar tissue space, as a volume effect. This may initiate the decrease in retinal perfusion. Previously, reductions in the systolic retinal and ciliary perfusion pressures were found after an injection of 5 ml but not after an injection of 2 ml [9]. In this study we found a reduction in retrobulbar velocity after an injection volume of 2 ml.
Second, it is known, that retrobulbar anaesthesia induces a rise in the intraocular pressure (IOP) of 3–4 mmHg [9, 16]. The effect of the IOP increase after retrobulbar anaesthesia is only short term [9]. Hessemer et al. [9] showed that the retinal and ciliary perfusion pressures remained decreased after the IOP had already returned to baseline.
Third, the autoregulation of the retinal circulation may be affected by local anaesthesia. Meyer et al. [17] demonstrated that bradykinin is prevented from relaxing porcine ciliary arteries in the presence of amide-type anaesthetic agents such as lidocaine. This may be an explanation for the sustained decrease in ocular blood flow. The diffusion of local anaesthetic into the retrobulbar vessels is proven by the detection of local anaesthetic agent in the peripheral blood [21].
In conclusion, the reduction in the retrobulbar velocity after retrobulbar anaesthesia was less marked, but still present, after surgery, when IOP had returned to baseline [9]. At that time the volume effect of the local anaesthetic on the retrobulbar haemodynamics has dissipated, because the agent has already spread into the surrounding tissue. This supports the theory of drug-induced vasoconstriction after retrobulbar anaesthesia.
Epinephrine is used in retrobulbar anaesthesia to slow the absorption of the anaesthetic, presumably by local vasoconstriction. Use of epinephrine in the retrobulbar solution may prolong the duration of anaesthesia [13]. On the other hand, epinephrine is known to have a vasoconstrictive effect [22]. In this study we showed a greater reduction and slower recovery of retrobulbar velocity after retrobulbar anaesthesia with the supplement of epinephrine. These results confirm those of other studies; greater reductions in ocular pulsation volume and in ciliary and retinal perfusion pressure are reported after retrobulbar anaesthesia with epinephrine [10]. Thus, there is a higher risk of reduced blood supply in the retina. Retrobulbar anaesthesia with epinephrine may therefore be associated with an increased risk of ischaemic complications [8].
In summary, there is a reduction in the retrobulbar velocity after retrobulbar anaesthesia; this may be due to a drug-induced vasoconstrictive effect of the local anaesthetics. This effect is enhanced by supplementation with epinephrine. Therefore, particularly in patients with already disturbed ocular haemodynamics retrobulbar anaesthesia with epinephrine should not be used in order to avoid irreversible functional damage.
References
Caroll FD (1973) Optic nerve compressions of cataract extraction. Trans Am Acad Ophthalmol Otolaryngol 77:623–629
Coupland SG, Deschenes MC, Hamilton RC (2001) Impairment of ocular blood flow during regional orbital anesthesia. Can J Ophthalmol 36:140–144
Evans DW, Harris A, Garrett M, Chung HS, Kagemann L (1999) Glaucoma patients demonstrate faulty autoregulation of ocular blood flow during posture change. Br J Ophthalmol 83(7):809–813
Gass JD, Parrish R (1982) Outer retinal ischemic infarction—a newly recognized complication of cataract extraction and closed vitrectomy. Part 1. A case report. Ophthalmology 89(12):1467–1471
Harris A, Williamson TH, Martin B et al (1995) Test/retest reproducibility of color Doppler imaging assessment of blood flow velocity in orbital vessels. J Glaucoma 4:281–286
Harris A, Spaeth G, Wilson R, Moster M, Sergott R, Martin B (1997) Nocturnal ophthalmic arterial hemodynamics in primary open-angle glaucoma. J Glaucoma 6(3):170–174
Hayreh SS (1980) Anterior ischemic optic neuropathy. IV. Occurrence after cataract extraction. Arch Ophthalmol 98(8):1410–1416
Hessemer V (1991) Anesthesia effects on ocular circulation. Synopsis of a study. Fortschr Ophthalmol 88(5):577–587
Hessemer V, Wieth K, Heinrich A, Jacobi KW (1989) Changes in uveal and retinal hemodynamics caused by retrobulbar anesthesia using various injection volumes. Fortschr Ophthalmol 86(6):760–766
Hessemer V, Heinrich A, Jacobi KW (1990) Ocular circulatory changes caused by retrobulbar anesthesia with and without added adrenaline. Klin Monatsbl Augenheilkd 197(6):470–479
Hulbert MF, Yang YC, Pennefather PM, Moore JK (1998) Pulsatile ocular blood flow and intraocular pressure during retrobulbar injection of lignocaine: influence of additives. J Glaucoma 7(6):413–416
Klein ML, Jampol LM, Condon PI, Rice TA, Serjeant GR (1982) Central retinal artery occlusion without retrobulbar hemorrhage after retrobulbar anesthesia. Am J Ophthalmol 93(5):573–577
Krohn J, Hovding G, Seland JH, Aasved H (1995) Retrobulbar anesthesia with and without adrenaline in extracapsular cataract surgery. A prospective, randomized, double-blind study. Acta Ophthalmol Scand 73(1):56–60
Leaming DV (1987) Practice styles and preferences of ASCRS members—1986 survey. J Cataract Refract Surg 13:561–567
Lieb WE (1998) Color Doppler imaging of the eye and orbit. Radiol Clin North Am 36(6):1059–1071
Meyer D, Hamilton RC, Loken RG, Gimbel HV (1992) Effect of combined peribulbar and retrobulbar injection of large volumes of anesthetic agents on the intraocular pressure. Can J Ophthalmol 27(5):230–232
Meyer P, Flammer J, Luscher TF (1993) Local anesthetic drugs reduce endothelium-dependent relaxations of porcine ciliary arteries. Invest Ophthalmol Vis Sci 34(9):2730–2736
Netland PA, Siegner SW, Harris A (1997) Color Doppler ultrasound measurements after topical and retrobulbar epinephrine in primate eyes. Invest Ophthalmol Vis Sci 38(12):2655–2661
Parrish R, Gass JD, Anderson DR (1982) Outer retina ischemic infarction—a newly recognized complication of cataract extraction and closed vitrectomy. Part 2. An animal model. Ophthalmology 89(12):1472–1477
Ruprecht KW, Naumann GOH (1985) Uni- und bilaterale ischämische Papilleninfarkte nach Katarakt-Extraktion. Fortschr Ophthalmol 82:349–352
Schaffer J, Biscoping J, Werry H, Morche F, Piepenbrock S (1989) Local anesthetic level and cardiovascular changes following local anesthesia in cataract operations with 3% mepivacaine. Fortschr Ophthalmol 86(4):319–322
Syrdalen P, Horven I (1970) Corneal indentation pulse and retrobulbar anesthesia. Acta Ophthalmol 48(4):719–730
Williamson TH, Harris (1996) Color Doppler ultrasound imaging of the eye and orbit. Surv Ophthalmol 40(4):255–267
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huber, K.K., Remky, A. Colour Doppler imaging before and after retrobulbar anaesthesia in patients undergoing cataract surgery. Graefe's Arch Clin Exp Ophthalmo 243, 1141–1146 (2005). https://doi.org/10.1007/s00417-004-0987-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-004-0987-7