Abstract
Background
To analyse vitrectomy results in diabetic eyes with retinal traction detachment and to investigate which variables are associated with a worse visual outcome.
Methods
Forty-four diabetic eyes (33 patients) with central retinal traction detachment were analyzed retrospectively.
Results
After a median follow-up of 10 months, median visual acuity significantly improved from 20/800 to 20/160 (P=0.02), despite the fact that the majority of patients had a long-standing macular traction detachment (median 120 days). Twenty-two eyes (50%) achieved a visual acuity of >20/200. The retina was finally reattached in 38 eyes (86.3%). Univariate analysis showed that patients with type 2 diabetes, age older than 50 years, preoperative visual acuity <20/200, iris neovascularisation and macular detachment of >30 days had a significantly worse final visual outcome. After multiple logistic regression analysis, age and iris neovascularisation were the strongest predictors of a worse visual outcome; if both were present, the chance of a obtaining a visual outcome of <20/200 was almost 90%.
Conclusions
Age and iris neovascularisation were the strongest predictors for a low visual outcome. In a review of vitrectomy studies in eyes with severe diabetic traction detachment in the past 2 decades, we found a trend towards higher anatomic success rates, while visual outcome only slightly improved. The current study confirmed the importance of ophthalmic variables, but also indicates the importance of evaluating systemic variables in larger series in order to predict which eyes may truly benefit from vitrectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical repair of advanced diabetic traction retinal detachment remains one of the most challenging tasks of the vitreoretinal surgeon. In the last 2 decades, various new surgical techniques have been introduced, which can all be used for the removal of fibrovascular membranes in these eyes: membrane segmentation [23], segmentation with membrane delamination [9], “en-bloc” excision of diabetic membranes using the attached posterior hyaloid membrane as an extra hand [2, 33], the “modified en bloc excision” of these membranes using a bimanual technique [12] and “total en-bloc excision” in which the glial ring (Weiss ring) together with the posterior hyaloid membrane is separated from the whole posterior pole with a hook [16]. The possibilities of bimanual surgery, the availability of wide-field viewing systems, perfluorocarbon liquids and silicone oil [8] and the use of the recently introduced multiport illumination system [29] have provided major technical support for the surgeon in the past 2 decades. Yet, do all these new techniques yield better visual results?
The above-mentioned studies on the surgical outcome in this end-stage of proliferative diabetic retinopathy have focused on the surgical technique. Visual recovery after surgery is dependent on recovery of macular function, which may be severely injured by long-standing macular detachment and oedema. Moreover, these eyes often have severe complications of the proliferative process, like neovascular glaucoma. The presence of iris neovascularisation and neovascular glaucoma was found to be a significant predictor for a low visual outcome in earlier studies [7, 21, 30, 31]. In addition to ischemic changes in the macula, vitreopapillary traction may damage the anterior optic nerve and cause ischemic optic neuropathy in these eyes [17]. Thus, despite vitrectomy, progression of the natural course of these eyes with advanced diabetic retinopathy may result in poor vision [10]. Systemic complications, such as nephropathy and hypertension may have an additional negative effect [4, 24]. Important clinical trials have demonstrated that systemic factors may worsen diabetic retinopathy [4, 24, 32]. Yet, only one study on vitrectomy results for diabetic traction retinal detachment evaluated the effect of systemic variables on the surgical outcome [22]. However, no statistical analysis was performed by the authors [22].
The aim of the current study was to analyse the effect of preoperative systemic and ophthalmic variables, intra-operative variables and postoperative complications on visual outcome after vitrectomy in diabetic eyes with central retinal traction detachment.
Subjects and methods
We reviewed the charts of all patients who had a primary vitrectomy for diabetic tractional retinal detachment in our clinic between June 1998 and December 2002. Eyes with fibrovascular traction detachment involving or threatening the macula and eyes with an incomplete vitreous detachment, with or without active retinal neovascularisations, were included. Eyes with a combined traction and rhegmatogenous retinal detachment and eyes with (a history of) uveitis or trauma were excluded. Only eyes for which a follow-up of at least 3 months was available were included. Ultimately, 44 eyes of 33 patients were incorporated in this study. The study was performed with the agreement of the institutional ethics committee; all patients gave their informed consent prior to inclusion in the study and after the nature of the study and possible consequences were explained. The study was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
For all eyes, data were available from pre-and postoperative examinations, including visual acuity testing, slit-lamp examination and biomicroscopy, intraocular pressure measurement and ultrasonography if a vitreous haemorrhage obscured the fundus. All patients were seen on a regular basis by internists, who monitored and controlled the diabetes, hyperlipidemia, hypertension and/or renal functions. Of all these 44 eyes a complete analysis could be made as described below.
Retrospectively, we recorded for each eye the following systemic preoperative variables: age, sex, duration of follow-up, type and duration of diabetes, glycosylated hemoglobin A1c (HbA1c), the number of systemic medications and whether the patient suffered from or had a history of hypertension, defined as a diastolic pressure of >90 mmHg, nephropathy or proteinuria, polyneuropathy, cardiovascular complications, such as myocardial infarction or congestive heart failure, varicose ulcer or amputation, or cerebrovascular accidents. In this study we used as criterion for a type 2 diabetes the onset of diabetes after the age of 30 years [30]. The following preoperative ophthalmic variables were collected: visual acuity in Snellen lines, previous ocular history and surgeries, including whether the eye was (a-)phakic or pseudophakic, whether or not panretinal photocoagulation or cryocoagulation and/or macular photocoagulation had been performed, the presence of vitreous haemorrhage or iris neovascularisation, whether the macula was attached or detached and the approximate duration of macular detachment. The following operative variables were evaluated: lensectomy, laser photocoagulation or external cryotherapy, iatrogenic retinal breaks and tamponade with silicone oil or gas. Also, the number and causes of additional operations were noted. In addition to vision and anatomic success, the following postoperative complications were recorded: recurrent traction detachment or rhegmatogenous retinal detachment, vitreous haemorrhage, new onset neovascular glaucoma, ischemic optic neuropathy, retinal ischemia or progressive cataract.
For follow-up, all patients were seen at regular intervals of 3 to 4 weeks by the authors. Visual acuity was measured in Snellen acuity. A change in vision was defined to be two lines if there was a change from light perception to finger counting or from finger counting to 20/200 and vice versa, as described earlier [18]. Final vision and anatomic success were determined from results of the most recent examination. An anatomic success was defined as a complete attachment of the retina or when there was a stable situation with a local detached peripheral retina anterior to the equator of less than two quadrants.
Operations were performed by three surgeons (EL, FH and AL). A standard three-port vitrectomy and segmentation/delamination technique [9] was used to remove central and midperipheral vitreous and fibrovascular membranes and to relieve antero-posterior and tangential epiretinal traction. We used a wide-angle viewing system (SDI/BIOM, Oculus, Wetzlar, Germany) in combination with an unimanual technique. In addition to the BIOM system, we used flat self-retaining disposable silicone vitrectomy lenses (DORC, Zuidland, The Netherlands) to enhance our view of the central macular area. In the majority of eyes, intra-operative endolaser or cryocoagulation was performed. The lens was simultaneously removed only in eyes that had a dense cataract that precluded a good retinal view during the operation. Oil or gas tamponade was used in eyes with long-standing traction retinal detachment as deemed necessary by the surgeon, or in eyes in which a retinal break occurred during the vitrectomy. At the end of surgery, subconjunctival injections of dexamethasone (2 mg) and gentamicin (4 mg) were administered. Postoperatively, eyes were treated topically with prednisolone acetate 0.1%, atropine 1% and ketorolac 0.5% (Acular) for approximately 3 months.
For statistical analysis, we consulted a professional statistician at our University Hospital (AGH Kessels, co-author). Snellen visual acuities were converted to a logarithmic scale (LogMAR, i.e., the logarithm of the minimal angle of resolution), as described earlier [11]. Comparisons between preoperative and postoperative visual acuities were made using the Wilcoxon signed rank test. For statistical analysis, visual acuity results were used that were obtained at the last follow-up visit, i.e., final corrected postoperative visual acuity. A poor visual outcome was defined as a visual acuity at final follow-up of less than 20/200. Univariate analysis was performed with the Chi-square or Fisher’s exact test to determine which of the preoperative, intra-operative and postoperative clinical variables was associated with a poor visual outcome. Secondly, a stepwise forward multiple logistic regression analysis was used for the following preoperative variables to determine the strongest predictors of a poor visual outcome, using a probability for entry of 0.1: age older than 50 years, duration of diabetes longer than 10 years, type of diabetes, more than three systemic medications, all the above-mentioned systemic complications, whether the eye was pseudophakic or aphakic or phakic at the time of vitrectomy, whether or not panretinal photocoagulation was performed preoperatively, the presence of a vitreous hemorrhage, iris neovascularisation and whether the macula was attached or detached for less than 30 days at the time of surgery. Although 11 of the 33 patients in this study were operated on both eyes, statistical analysis was performed on the total of 44 eyes, because some of the systemic factors differed between the eyes within the same patient as a consequence of a different time point at which the second eye was operated.
Results
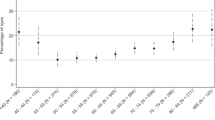
The baseline systemic and ophthalmic characteristics of the 44 eyes of 33 patients are summarized in Table 1. Nineteen patients were female, fourteen were male. Twenty-two (50%) of the 44 eyes had a visual acuity of >20/200 at the end of follow-up, and 28 (64%) had a visual acuity of >5/200. After a median follow-up of 10 months (range 3 to 36 months), median visual acuity significantly improved from 20/800 (range: light perception to 20/50) to 20/160 (range no light perception to 20/20) (P=0.02), despite the fact that the majority of patients had a long-standing macular traction detachment (median 120 days, range 10 days to more than 1 year) (Fig. 1). In 33/44 eyes (75%) final visual acuity stabilised or improved by one line after vitrectomy. Six eyes decreased one line in visual acuity, four eyes had a deterioration in their visual acuity of three to four lines, and one eye decreased by ten lines. This latter eye developed neovascular glaucoma and a rhegmatogenous retinal detachment after the primary vitrectomy. Iris neovascularisation was present in eight eyes preoperatively, and regressed postoperatively in three eyes.
Univariate analysis showed that age older than 50 years (P=0.026), type 2 diabetes (P=0.021), a preoperative visual acuity of less than 20/200 (P=0.021), iris neovascularisation (P=0.019) and macula detached for more than 30 days (P=0.042) were preoperative variables that were significantly associated with a worse visual outcome (Table 1). After a step-wise multiple logistic regression analysis with all preoperative variables using a probability for entry of 0.1, age older than 50 years (odds ratio 3.7, 95% confidence interval 0.9 to 15.4) and iris neovascularisation (odds ratio 7.8, 95% confidence interval 0.8 to 74.1) were the strongest predictors for a poor visual outcome. We incorporated age older than 50 years and iris neovascularisation in a prediction algorithm (model), which resulted in the following prediction rule: if both variables were present, the chance of obtaining a visual outcome of <20/200 was 86%. As a rule of thumb, Harrell et al. [13] suggested that in order to have a reliable predictive discrimination, the number of parameters in such a model should not exceed m/10, with m the number of patients in the less frequent outcome category. In our model, we included two parameters (age and iris neovascularisation), and the number of patients (eyes) with a visual outcome of <20/200 was 22, whereas the number of patients (eyes) with a visual outcome of >20/200 was also 22 (i.e., m=22).
Intraocular tamponade was deemed necessary in 19 eyes. Silicone oil was used in ten eyes and long-acting gas (16% C3F8) was used in nine eyes. In the other 25 eyes no (air) tamponade was used. Table 2 summarises details of variables related to the vitrectomy procedure and postoperative complications in relation to the final visual acuity. Primary lensectomy was performed in a minority of the eyes. The majority of eyes (41/44, Table 1) had panretinal photocoagulation before the operation, and 35/44 eyes were also treated with endolaser or cryotherapy during the vitrectomy (Table 2). None of the intraoperative variables had a significant association with a poor visual outcome.
The retina was reattached in 31/44 (70%) eyes after one vitrectomy. Ten eyes developed a recurrent retinal traction detachment and three other eyes developed a rhegmatogenous retinal detachment as complication of the primary vitrectomy (Table 2). These latter three eyes all had subsequent vitrectomy with silicone oil and had an attached retina at final follow-up. Five eyes with a recurrent macular traction detachment had one or more subsequent vitrectomies after the primary vitrectomy. In addition, five other eyes that developed a recurrent macular traction detachment were not reoperated, and further surgery was abandoned for the following reasons: two of these five eyes had a traction retinal detachment that had existed for approximately 1 year before we performed the primary vitrectomy. One eye developed an uncontrollable neovascular glaucoma with no light perception, one eye had an ischemic optic neuropathy and one patient deceased. Thus, finally the retina was reattached in 38/44 (86%) of the eyes. In 11 eyes silicone oil was not removed at the end of this study.
Neovascular glaucoma was present in eight eyes postoperatively, and this complication was significantly associated with a worse visual outcome (P=0.046). Three of these eight eyes developed this complication after the vitrectomy (Table 2). Ischemic optic neuropathy and ischemic retinopathy after an arterial or venous occlusion were two other major complications responsible for a low final visual acuity; however, they were not statistically significant. Two eyes ended with no light perception due to neovascular glaucoma and ischemic optic neuropathy. None of the eyes developed hypotony after vitrectomy.
Discussion
By univariate analysis we found that the following preoperative ophthalmic variables were significantly associated with a worse visual outcome: a preoperative visual acuity <20/200, iris neovascularisation and macular detachment of >30 days. With multiple logistic regression analysis, iris neovascularisation was the strongest ophthalmic variable that predicted a worse visual outcome. Our findings on these ophthalmic variables confirm previous studies [7, 25, 26, 30, 31].
From large clinical trials it is known that severe diabetic retinopathy is an indicator of poor metabolic control and poor physical condition of the patient [4, 24, 32]. An earlier study on vitrectomy for diabetic retinopathy found that 50% of patients with heart disease died within 3.5 years [24]. Advanced renal disease, hypertension and anemia are risk factors for the progression of diabetic retinopathy [4, 24, 32]. But also, the treatment of systemic complications can affect the progression of diabetic retinopathy. Despite their importance, systemic variables were not statistically analysed in any of the previous studies on the outcome of vitrectomy in these patients. Eleven systemic variables were evaluated in the current study, and we found that age (after multivariate analysis) and type 2 diabetes (after univariate analysis) were significantly associated with a poor visual outcome. More systemic variables would probably be significant with a larger number of eyes. Thus, in addition to its retrospective nature, a disadvantage of the current study was a relatively high number of variables compared to a relatively small number of study eyes.
In a review of the literature, we found that after vitrectomy with membrane dissection improved or stabilised vision is reported in 55 to 89% of the eyes [1, 5, 6, 7, 8, 12, 15, 16, 20, 21, 22, 25, 26, 27, 28, 29, 30, 31, 33, 34]. Table 3 summarises studies on vitrectomy results of eyes with central diabetic retinal traction detachment over the past 25 years. About 60 to 80% (range 22 to 77%) of eyes achieve a visual acuity of >5/200, and a final anatomic success is reported in 33 to 100% [1, 5, 6, 7, 8, 12, 15, 16, 20, 21, 22, 25, 26, 27, 28, 29, 30, 31, 33, 34]. Earlier studies are comparable to the current study, in which these percentages were 64 and 86%, respectively. In all studies, however, different entry and exclusion criteria are used and percentages are therefore sometimes difficult to compare. In some studies eyes with a combined traction and rhegmatogenous retinal detachment [8, 15, 20, 31] were included. Other studies excluded eyes with preoperative iris neovascularisation [29] or pre-existing retinal breaks [29, 30], which are variables that have been shown to be significantly associated with a poorer visual outcome [31, 7]. Studies from the United States, where the use of silicone oil was temporarily limited by the U.S. Food and Drug Administration [5], used silicone oil only in very severe cases, and this may explain the lower levels of visual outcome in some of these studies [6, 28]. Moreover, the percentage of eyes in which oil is removed at final follow-up may vary, depending on the stability of the retinal attachment and the severity of the proliferative process, and this may also be an indication of case complexity. In the current study, oil was removed in 3 (23%) of 13 eyes, which is somewhat higher than reported in earlier studies (8 to 21% [5, 15]), or by Meier et al. [22] (none of the 28 eyes) and somewhat lower than recently reported by Castellarin et al. [8] (35%).
Despite major improvements in surgical techniques and equipment, visual outcome after vitrectomy in these eyes with central traction retinal detachment has only slightly improved in the past 25 years (Table 3). This trend with improvement in anatomical success but limited visual improvement was also reported earlier for primary rhegmatogenous retinal detachment (RRD) repair [3]. A delay from first clinic attendance to time of surgery and an increase in the incidence of macular detachments were probably responsible for this lack of visual improvement [3]. In the current study, in which the majority of patients were referred to our clinic and already had long-standing macular traction detachment, this may partly explain our moderate visual outcome.
In a recent study, Castellarin et al. [8] used a complexity score indicating the severity of the proliferative process in the evaluation of vitrectomy results on eyes with severe diabetic traction detachment. Although techniques have markedly improved since the earlier studies from the DRVS, it was already shown in the DRVS [10] report no. 3 that of the eyes with advanced active proliferative diabetic retinopathy and a useful vision of 10/200 that underwent early vitrectomy, only about 60% achieved a vision of >5/200 or better after 2 years because of complications resulting from the proliferative process [10]. As in earlier studies, in the current study, iris neovascularisation was significantly associated with a worse visual outcome [7, 21, 30, 31]. Neovascular glaucoma was another major factor responsible for a low final visual outcome, which confirms earlier reports [7, 21, 30, 31]. Loss of light perception may occur in up to 23% of eyes [1, 5, 6, 7, 8, 12, 15, 16, 20, 21, 22, 25, 26, 27, 28, 29, 30, 31, 33, 34]. In the current study, two eyes (5%) ended with no light perception (NLP). Loss of light perception may be due to progression of the proliferative process or result from ischemic maculopathy and/or optic nerve atrophy. NLP can occur postoperatively in a number of eyes with advanced ischemic PDR, and it is likely that this percentage of postoperative eyes with NLP will increase with the duration of follow-up. By re-calculating the data form Table 3, the number of cases with more than 10 months of follow-up have a higher rate of postoperative blindness than those with a shorter follow-up (P=0.09). With a higher number of cases, this difference would probably become more statistically significant. Ischemia of the retina and optic nerve seem to be the main reason for a postoperative total loss of vision. Results from the DRVS [10] showed that approximately 41% of eyes classified as having Very Severe New Vessels (NVC-4) that were assigned to conventional management and 31% of these NVC-4 eyes assigned to early vitrectomy ended with no light perception after 3 years.
In summary, age and iris neovascularisation were the strongest predictors for a low visual outcome in the current study. Since this group of patients has a high rate of systemic complications associated with progression of diabetic retinopathy, systemic preoperative variables should be incorporated in every preoperative complexity score. In a review of vitrectomy studies on eyes with severe diabetic traction detachment in the past 2 decades, we found a trend towards higher anatomic success rates, while visual outcome only slightly improved. The current study confirmed the importance of ophthalmic variables, but also indicates the importance of evaluating systemic variables in larger series in order to predict which eyes may truly benefit from vitrectomy.
References
Aaberg TM (1981) Pars plana vitrectomy for diabetic traction retinal detachment. Ophthalmology 88:639–642
Abrams GW, Williams GA (1987) “En bloc” excision of diabetic membranes. Am J Ophthalmol 103:302–308
Ah-Fat FG, Sharma MC, Majid MA, et al (1999) Trends in vitreoretinal surgery at a tertiary referral centre: 1987 to 1996. Br J Ophthalmol 83:396–398
Aiello LP, Cahill MT, Wong JS (2001) Sytemic considerations in the management of diabetic retinopathy. Am J Ophthalmol 132:760–776
Azen SP, Scott IU, Flynn HW Jr, et al (1998) Silicone oil in the repair of complex retinal detachments. A prospective observational multicenter study. Ophthalmology 105:1587–1597
Brourman ND, Blumenkranz MS, Cox MS, et al (1989) Silicone oil for the treatment of severe proliferative diabetic retinopathy. Ophthalmology 96:759–764
Bustros de S, Thompson JT, Michels RG, Rice TA (1987) Vitrectomy for progressive proliferative diabetic retinopathy. Arch Ophthalmol 105:196–199
Castellarin A, Grigorian R, Bhagat N, Del Priore L, Zarbin MA (2003) Vitrectomy with silicone oil infusion in severe diabetic retinopathy. Br J Ophthalmol 87:318–321
Charles S (1981) Vitreous Microsurgery. Williams and Wilkins, Baltimore, pp 107–120
Diabetic Retinopathy Vitrectomy Study Research Group (1988) Early vitrectomy for severe proliferative diabetic retinopathy in eyes with useful vision. Results of a randomized trial diabetic retinopathy vitrectomy study, report 3. Ophthalmology 95:1307–1320
Ferris FL, Kassoff A, Bresnick GH, et al (1982) New visual acuity charts for clinical research. Am J Ophthalmol 94:91–96
Han DP, Murphy ML, Mieler WF (1994) A modified en bloc excision technique during vitrectomy for diabetic traction retinal detachment. Ophthalmology 101:803–808
Harrel F, Lee K, Mark D (1996) Tutorial in biostatistics multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Helbig H, Kellner U, Bornfeld N, et al (1996) Life expectancy of diabetic patients undergoing vitreous surgery. Br J Ophthalmol 80:640–643
Imamura Y, Minami M, Ueki M, et al (2003) Use of perfluorocarbon liquid during vitrectomy for severe proliferative diabetic retinopathy. Br J Ophthalmol 87:563–566
Kakehashi A (2002). Total en bloc excision: a modified vitrectomy technique for proliferative diabetic retinopathy. Am J Ophthalmol 134:763–765
Kroll P, Wiegand W, Schmidt J (1999) Vitreopapillary traction in proliferative diabetic vitreoretinopathy; Br J Ophthalmol 83:261–264
La Heij EC, Hendrikse F, Kessels AGH et al (2001) Vitrectomy results in diabetic macular oedema without evident vitreomacular traction. Graefes Arch Clin Exp Ophthalmol 239:264–270
Lucke KH, Foerster MH, Laqua H (1987) Long-term results of vitrectomy and silicone oil in 500 cases of complicated retinal detachments. Am J Ophthalmol 104:624–633
Maturi RK, Merrill PT, Lomeo MD, Diaz-Rohena R, Khan M, Lambert HM (1999) Perfluoro-N-octane (PFO) in the repair of complicated retinal detachments due to severe proliferative diabetic retinopathy. Ophthalmic Surg Lasers 30:715–720
McCuen BW 2nd, Rinkoff JS (1989) Silicone oil for progressive anterior ocular neovascularisation after failed diabetic vitrectomy. Arch Ophthalmol 107:677–682
Meier P, Wiedemann P (1997) Vitrectomy for traction macular detachment in diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 235:569–574
Meredith TA, Kaplan HJ, Aaberg TM (1980) Pars plana vitrectomy techniques for relief of epiretinal traction by membrane segmentation. Am J Ophthalmol 89:408–413
Rice TA, Michels RG (1983) Vitrectomy for diabetic rhegmatogenous retinal detachment. Am J Ophthalmol 95:34–44
Rice TA, Michels RG, Rice EF (1983) Vitrectomy for diabetic retinal detachment involving the macula. Am J Ophthalmol 95:22–33
Rinkoff JS, de Juan E Jr, McCuen BW 2nd (1986) Silicone oil for retinal detachment with advanced proliferative vitreoretinopathy following failed vitrectomy for proliferative diabetic retinopathy. Am J Ophthalmol 101:181–186
Scott IU, Flynn HW, Lai M, et al (2000) First operation anatomic success and other predictors of postoperative vision after complex retinal detachment repair with vitrectomy and silicone oil tamponade. Am J Ophthalmol 130:745–750
Steinmetz RL, Grizzard S, Hammer ME (2002) Vitrectomy for diabetic tration retinal detachment using the multiport illumination system. Ophthalmology 109:2303–2307
The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group (2000) Retinopathy and nephropathy in patients with type 1 diabetes 4 years after a trial of intensive therapy. N Engl J Med 342:381–389
Thompson JT, Bustros de S, Michels RG, Rice TA (1987) Results and prognostic factors in vitrectomy for diabetic traction retinal detachment of the macula. Arch Ophthalmol 105:497–502
Thompson JT, Bustros de S, Michels RG, Rice TA (1987) Results and prognostic factors in vitrectomy for diabetic traction retinal detachment of the macula. Arch Ophthalmol 105:503–507
UK Prospective Diabetes Study Group (1998) Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes. UKPDS 38. BMJ 31:317:703–713
Williams DF, George A. Williams, Arthur Hartz, William F. Mieler, Gary W. Abrams, Aaberg TM (1989) Results of vitrectomy for diabetic traction retinal detachments using the en bloc excision technique. Ophthalmology 96:752–758
Yeo JH, Glaser BM, Michels RG (1987) Silicone oil in the treatment of complicated retinal detachments. Ophthalmology 94:1109–1113
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have not received any financial support. The authors have no proprietary interest related to this article.
Rights and permissions
About this article
Cite this article
La Heij, E.C., Tecim, S., Kessels, A.G.H. et al. Clinical variables and their relation to visual outcome after vitrectomy in eyes with diabetic retinal traction detachment. Graefe's Arch Clin Exp Ophthalmol 242, 210–217 (2004). https://doi.org/10.1007/s00417-003-0815-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-003-0815-5