Abstract
Objective
Progressive supranuclear palsy (PSP) is a progressive neurodegenerative disease, and sometimes shows idiopathic normal pressure hydrocephalus (iNPH)-like presentations. We aimed to evaluate spinal tap responsiveness in patients with PSP, including the effect of sham spinal tap.
Methods
Eleven patients with PSP, ten with probable/definite iNPH, and eight control patients were prospectively enrolled. All participants underwent sham spinal tap and spinal tap procedures. Gait was evaluated using wearable inertial sensors. We defined “tap responders” as individuals with a 10% or more improvement from baseline in any of the gait parameters (timed up-and-go test total time, stride length, and velocity during straight walking under single-task and cognitive dual-task conditions). We compared the ratio of responders in patients with PSP to patients with iNPH and controls.
Results
The ratio of tap responders and the ratio of sham tap responders in patients with PSP were significantly higher than those in control patients, and not different from those in patients with iNPH. PSP patients with iNPH-like MRI features tended to respond to the spinal tap compared to those without such imaging features. Notably, one patient with PSP, who responded to the spinal tap beyond the effect of sham spinal tap, was treated by the shunt operation.
Conclusion
This is the first prospective study to demonstrate tap and shunt responsiveness in patients with PSP while highlighting the placebo effects of the spinal tap in patients with PSP or iNPH. Our findings suggest that some PSP patients have impaired cerebrospinal fluid circulation, contributing to a distinct component of the clinical spectrum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Progressive supranuclear palsy (PSP) is a progressive neurodegenerative disease that is characterized by supranuclear gaze palsy, akinetic rigidity, gait disturbance, and dementia [1]. PSP presents with various clinical phenotypes that mimic other diseases [2] and occasionally manifests with idiopathic normal pressure hydrocephalus (iNPH)-like presentations [3, 4]. iNPH is a clinical disease entity that is characterized by the triad of gait disturbance, dementia, and urinary disturbance, and these symptoms can be improved by shunt operation [5]. We previously demonstrated that PSP develops iNPH-like MRI features, particularly a high disproportionately enlarged subarachnoid space hydrocephalus (DESH) score (≥ 5), more often than other neurodegenerative diseases, and proposed a concept of PSP with hydrocephalus [4]. Similarly, the concept of NPH secondary to neurodegenerative diseases (neurodegenerative NPH) has been also proposed [6], and PSP is one of the most common etiologies of neurodegenerative NPH [3]. However, no prospective studies have evaluated iNPH-like clinical presentations, including spinal tap/shunt responsiveness, in patients with PSP. Previous literature has reported autopsy-proven patients with PSP who responded to the shunt operation with an antemortem diagnosis of iNPH [3, 6,7,8,9], indicating the existence of iNPH-like clinical features in patients with PSP. We hypothesize that some symptoms of PSP would be improved by spinal tap/shunt operation albeit temporarily, based on these reports.
Spinal tap responsiveness is a distinct feature of iNPH and is thus included in the diagnostic criteria for probable iNPH in the Japanese guideline [10]. However, a conventional spinal tap presents several challenges for accurately diagnosing iNPH. The potential placebo effects of spinal taps and shunt operations on the symptoms have been discussed [11]. A review study performed by Espay et al. showed that the response rates to the shunt operation in patients with iNPH varied from 31 to 89% [6]. This variable response rate to the shunt operation indicates that the shunt operation is often performed for inappropriate individuals, including those who seemed to “respond” to the spinal tap by a placebo effect [11].
Furthermore, the spinal tap exhibits an average specificity of 75% in predicting the outcomes of shunt operation [12], thereby emphasizing the issue of false positives associated with this diagnostic approach. A case report has documented the utility of a sham spinal tap to address the challenge of low diagnostic accuracy [13]. Therefore, to ascertain the existence of patients with PSP having spinal tap responsiveness, we employed a novel protocol that incorporated both a spinal tap and a sham spinal tap.
In this study, we aimed to evaluate the effect of spinal taps and sham spinal taps on gait and cognitive function in patients with PSP compared to those with iNPH or control patients.
Material and methods
Participants
Patients with PSP and participants with hydrocephalus, as defined by a high Evans index (EI) > 0.30 [14] or a small callosal angle (CA) on the coronal plane at the posterior commissure < 90° [15], were prospectively recruited at an outpatient clinic in the Department of Neurology at Tokyo Medical and Dental University Hospital from 2018 to 2022. The clinical diagnosis was made according to the Movement Disorder Society Clinical Diagnostic Criteria for clinically suggestive of, possible, or probable PSP [16] and the Japanese guidelines for clinically probable or definite iNPH [10]. Among the participants with hydrocephalus, patients with diagnoses other than iNPH were enrolled in the control group. Patients with PSP were enrolled even if hydrocephalus was present since all previous autopsy-proven PSP patients with response to the shunt operation had hydrocephalus [3, 6,7,8,9]. Patients were included if they were older than 40 years old at enrollment and had no current medical history with anti-thrombotic medications. Patients with brain tumors, intracranial hemorrhage, bleeding tendency, difficulties in walking for at least 20 m, or skin infection at the lumbar puncture site were excluded.
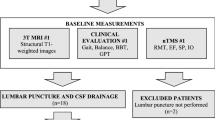
Study design
All patients underwent gait analysis five times: twice within 5 days before the sham spinal tap, once within 1 day after the sham spinal tap, and twice within 5 days after the spinal tap (Fig. 1). Better gait parameters obtained before the sham spinal tap and after the spinal tap were used for analysis. Additional gait analysis was conducted following the shunt operation in patients who underwent it. Neuropsychological tests were performed within 7 days before and 3 days after the spinal tap. Baseline disease severity was also evaluated using the Motor Examination of Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS part III) [17] and the iNPH grading scale (iNPHGS) [18]. Motor function, including gait, was assessed in all patients by a board-certified neurologist (M.O.). The Institutional Review Boards of Tokyo Medical and Dental University Hospital approved this study. All data were collected as a part of a prospective study and written informed consent was obtained from all participants.
Procedure of sham spinal tap and spinal tap test
All patients underwent a sham spinal tap after the two baseline gait assessments. Patients were explained that 30 mL of cerebrospinal fluid in total would be collected by the two spinal tap procedures. As the sham spinal tap, a needle was inserted subcutaneously after the focal anesthesia, not inserted into the spinal column, and was kept subcutaneously for 15 min. The patient was told that the spinal tap was successfully performed following the procedure. Within three days after the sham spinal tap, 30 mL of cerebrospinal fluid was removed by the spinal tap (Fig. 1). Then, the patient was told again that the spinal tap was successfully performed.
Brain MRI and DAT- and MIBG-SPECT
The EI [14], the CA in the coronal plane at the posterior commissure [15], the CA at the splenium [19], DESH score [20], and Magnetic Resonance Hydrocephalic Index (MRHI) [21] were evaluated using 3-dimensional T1-weighted image. A high DESH score (≥ 5) is a useful predictor of positive responsiveness to shunt operation in patients with iNPH [20], and may also be useful in characterizing iNPH-like MRI features in neurodegenerative disorders including PSP [4]. To ascertain the pathological background, all patients underwent dopamine transporter- and cardiac 123I-metaiodobenzylguanidine-single photon emission computed tomography (DAT-SPECT and cardiac MIBG-SPECT, respectively). Abnormalities on DAT-SPECT were assessed by visual evaluation [22, 23] and quantitative analysis [24]. We employed DaTView (Nihon Medi-Physics Co., Ltd.) which compares the DAT uptake value of the basal ganglia to the mean DAT uptake value of the whole brain excluding the basal ganglia. Patients’ specific binding ratio was compared with that of the age-matched healthy individuals to quantify dopaminergic denervation. The abnormality of cardiac MIBG-SPECT was evaluated based on the low early heart/mediastinum (H/M) ratio [25] or delayed H/M ratio [25, 26], compared with the standardized cut-off values of healthy controls. Cardiac MIBG-SPECT exhibits high sensitivity and specificity (approximately 90%) in distinguishing Lewy body diseases and disease controls [27]. DAT-SPECT and MIBG-SPECT were evaluated by radiologists who were blinded to the clinical diagnosis.
Gait analysis
The participants’ gait was measured and analyzed using inertial measurement units (IMUs; WALK-MATE Viewer®, WALK-MATE LAB., Tokyo, Japan) attached by bilateral bands at the ankles and hips [28]. All patients were instructed to walk fast-paced to minimize inter-trial variation. Stride length and stride velocity were measured under the following two conditions: 1) walking a distance of 15 m (straight walking) and 2) straight walking under a cognitive dual-task (walking with serial 7 subtractions from 500). The timed up-and-go test (TUG) was also performed 3 times using a standardized method [29] and the mean TUG total time was used for analysis. Tap responders to gait function were defined by those who exhibited a 10% improvement from baseline [30] for any of the gait parameters (TUG total time, stride length, and stride velocity during straight walking under single and cognitive dual tasks).
Neuropsychological tests
Global cognition was first evaluated by using the Japanese version of the Montreal Cognitive Assessment test (MoCA-J) [31]. Then, comprehensive neurocognitive assessments, which were composed of six cognitive domains, were performed by neuropsychologists. Six cognitive domains were evaluated by at least two batteries for each cognitive domain as follows: (1) Immediate memory: list memory and episode memory (subsection of the Japanese version of the repeatable battery for the assessment of neuropsychological status (RBANS) [32]), (2) Delayed memory: list recall, list recognition, episode recall, and figure recall (subsection of RBANS), (3) Visuospatial function: figure copy and line orientation (subsection of RBANS), (4) Language: picture-naming and category fluency (subsection of RBANS) as well as auditory verbal comprehension (subsection of Western Aphasia Battery [33]), (5) Attention/working memory: digit span and letter-number sequencing subtests (subsection of RBANS), and (6) Executive function: the rule shift cards test (subsection of the Behavioral Assessment of the Dysexecutive Syndrome [34]), letter fluency test [35], and time to complete part A and part B of trail making test [36]. Each test score was converted to a scaled score by using age-matched norms. In a previous report about the diagnostic criteria for mild cognitive impairment in Parkinson’s disease, deficits of at least − 1.5 standard deviations (SD) on two or more subtests in neuropsychological tests were reported to be suitable to diagnose Parkinson’s disease with mild cognitive impairment [37, 38]. Based on these reports, tap responders to cognitive function were defined as those who exhibited a 1.5 SD or more improvement in the scaled score from baseline in at least two or three neuropsychological test.
Outcome measures
The primary outcome was to evaluate the inter-group difference between patients with PSP and iNPH or control patients regarding the ratio of the spinal tap responders to gait function. The secondary outcome was to examine the inter-group differences between patients with PSP and iNPH or control patients in the ratio of the spinal tap responders to cognitive function and in the ratio of the sham spinal tap responders to gait function.
Statistical analyses
Statistical analyses were performed using the GraphPad Prism 9 software (GraphPad Software, San Diego, CA, USA). For continuous variables, inter-group differences between patients with PSP and the other groups were evaluated using the Kruskal–Wallis test followed by Dunn’s test. For categorical variables, inter-group differences between patients with PSP and the other groups were evaluated using Fisher’s exact test with the Bonferroni correction. The Friedman test followed by Dunn’s test was performed to analyze the changes in gait parameters in the three groups over time (at baseline, after the sham spinal tap, and after the spinal tap).
Results
Demographic and clinical data in the three groups
Eleven drug-naïve patients with PSP (nine with probable PSP with Richardson’s syndrome (PSP-RS) and two with suggestive PSP with predominant postural instability) and 22 patients with hydrocephalus were prospectively enrolled (Fig. 2). Eight of the 22 patients with hydrocephalus had diagnoses other than iNPH and were enrolled in the control group (see their diagnosis in Fig. 2). Ten of the 22 patients with hydrocephalus were diagnosed with probable or definite iNPH. Two patients with possible iNPH who neither exhibited DESH nor responded to spinal taps were excluded. Two patients without shunt responses were analyzed separately as shunt non-responders 1 and 2 (Fig. 2). The clinical data of the participants are shown in Table 1. Individual data are shown in Supplementary Table 1. Age, sex, and disease duration in patients with PSP were not significantly different from those in the iNPH and control groups. The ratio of patients with vertical supranuclear gaze palsy or fall tendency in the PSP group was significantly higher than that in the iNPH (P = 0.0004, 0.0004, respectively) and control groups (P = 0.001, 0.0004, respectively). The iNPHGS gait domain and MDS-UPDRS part III scores were significantly higher in patients with PSP than in controls (P = 0.007 and 0.002, respectively). The imaging parameters at baseline are also listed in Table 1 and Supplementary Table 1. No significant differences in the ratio of patients with abnormal EI or CA at the posterior commissure were observed between the groups. The ratio of patients with abnormal CA at the splenium or abnormal MRHI in PSP was significantly smaller than those in iNPH (P = 0.047, 0.018, respectively) and the ratio of patients with abnormal DESH score in PSP was significantly smaller than those in controls (P = 0.040). The ratio of patients with DAT-SPECT abnormalities in patients with PSP was significantly higher than that in patients with iNPH (P < 0.0001) and control patients (P = 0.002).
Inter-trial comparison of the spinal tap/sham tap effect on gait function
Gait variables in the three groups at baseline, after the sham spinal tap, and after the spinal tap are shown in Table 2. For patients with PSP, the TUG total time after spinal tap test was significantly shorter than that at baseline (P = 0.038) and the dual-task stride velocity after spinal tap was significantly higher than at baseline (P = 0.028). For patients with iNPH, stride length and velocity after spinal tap test were significantly higher than at baseline (P = 0.028 and 0.007, respectively). The trajectories of gait variables after each procedure were described in Supplementary Fig. 1. Some patients showed improvements in gait parameters only in the second post-tap assessment, indicating the presence of individual variabilities in response timing to the spinal tap.
The magnitude of improvement from baseline in gait parameters was also compared between after sham spinal tap and after spinal tap within each group (Supplementary Fig. 2). There were some trends that gait parameters such as TUG total time were improved after the spinal tap compared to those after the sham tap in patients with PSP. In patients with iNPH, both stride lengths and velocities under the dual-task condition were significantly improved after the spinal tap than those after the sham tap (P = 0.020, 0.020, respectively).
Inter-group comparison of responder ratio on gait function to the spinal tap/sham spinal tap
The ratios of responders to the spinal taps and sham spinal taps in each group are shown in Table 3. The proportion of patients with improvement in any gait parameter after the spinal tap in the PSP group (9 out of 11 patients, 82%) was significantly higher than that in the control group (2 out of 8 patients, 25%; P = 0.047), but it was not significantly different from that in iNPH group (9 out of 10 patients, 90%; P > 0.999). The proportion of patients with improvement in any gait parameter after the sham spinal tap in patients with PSP (8 out of 11 patients, 73%) was significantly higher than that in control patients (1 out of 8 patients, 13%; P = 0.040), but it was not significantly different from that in patients with iNPH (6 out of 10 patients, 60%; P > 0.999). The ratio of patients with improvement in any gait parameter after the spinal tap, as compared to the better gait parameters at the baseline or after sham spinal tap measurements, did not demonstrate a significant difference between patients with PSP (5 out of 11 patients, 45%), patients with iNPH (6 out of 10 patients, 60%; P > 0.999), or control patients (2 out of 8 patients, 25%; P > 0.999). A comparison of the magnitude of gait improvement following each test showed no significant differences between PSP group and iNPH group or control group (Supplementary Fig. 3).
Within the PSP cohort, the ratio of responders to gait function was compared between patients with PSP with a high DESH score ≥ 5 and patients with PSP with a low DESH score < 5 (Table 4). The ratio of those who showed improved stride length after the spinal tap was significantly larger in patients with PSP with DESH score ≥ 5 than in patients with PSP with DESH score < 5 (Table 4; P = 0.024). Similarly, the gait of PSP patients with abnormal EI and CA at the posterior commissure also tended to improve after the spinal tap (Supplementary Table 2).
The ratio of the responder to the spinal tap and sham spinal tap in nine patients with PSP-RS was compared to that in other groups (Supplementary Table 3). Although there were no significant differences in the proportion of responders between PSP-RS cohort and other groups, patients with PSP-RS tended to respond to the spinal tap compared with the control group (at least one gait parameter; P = 0.113).
Inter-group comparison of responder ratio on cognitive function to the spinal tap
The cognitive functions of the tap responders were compared between the groups (Table 5). When at least 1.5 SD changes of the scaled score in two or more cognitive batteries were defined as responders, 5 out of 11 patients with PSP (45%) responded to the spinal tap, while 5 out of 10 patients with iNPH (50%) and 3 out of 8 control patients (38%) responded to the spinal tap. When at least 1.5 SD changes in the scaled score in three or more cognitive batteries were defined as responders, 1 out of 11 patients with PSP (9%) responded to the spinal tap, while 3 out of 10 patients with iNPH (30%), and 1 out of 8 control patients (13%) responded to the spinal tap. There was no significant difference between the groups in the ratio of patients with improved cognitive function with at least two batteries and at least three batteries.
Analysis for patients who had shunt operation
One of the 11 patients with PSP (Case 1 in Fig. 3, Table 6) and 4 of the 12 patients with probable iNPH (Fig. 2) underwent a shunt operation. The response rates of the gait parameters after sham spinal tap, spinal tap, and shunt operations are shown in Table 6. One patient with PSP-RS (Case 1 in Fig. 3 and Table 6) and two patients with definite iNPH (definite iNPH-1 and definite iNPH-2 in Table 6), who responded to the shunt operation, initially responded to the spinal tap more than the sham spinal tap. However, two shunt non-responders (shunt non-responder-1 and shunt non-responder-2 in Table 6) did not respond to the spinal tap more than the sham spinal tap.
Representative PSP patients with spinal tap responsiveness. a–c T1-weighted images and d DAT-SPECT in a 76-year-old woman with probable PSP-RS (Case 1). Right SBR was 1.79 and left SBR was 1.79. e Longitudinal gait/MDS-UPDRS part III assessments in Case 1. f–h T1-weighted images and i DAT-SPECT in a 72-year-old man with probable PSP-RS (Case 2). Right SBR was 1.79 and left SBR was 2.49. j Longitudinal gait/MDS-UPDRS part III assessments in Case 2. e, j Improvements by more than 10% from the baseline are shown in bold italics. TUG timed up-and-go test, MDS-UPDRS Movement Disorder Society Unified Parkinson’s Disease Rating Scale, SBR Specific Binding Ratio
Two representative patients with PSP-RS who responded to spinal taps are shown in Fig. 3. Case 1 is a 76-year-old woman presented with the typical symptoms of PSP-RS, including supranuclear vertical gaze palsy and postural instability (Fig. 3a–e). MRI showed slight atrophy of the midbrain, ventricular enlargement, a dilated Sylvian fissure, and a high tight convexity, suggesting the presence of iNPH-like MRI features (Fig. 3a–c). Although DAT-SPECT showed dopaminergic denervation (Fig. 3d), cardiac MIBG-SPECT results were normal. Her gait parameters and MDS-UPDRS part III scores improved after spinal tap and shunt operations (Fig. 3e). In Case 2, a 72-year-old man presented with progressive gait difficulties and frequent falls (Fig. 3f–j). Neurological examination revealed supranuclear vertical gaze palsy and Parkinsonism with marked postural impairment. Brain MRI revealed midbrain atrophy and dilatation of the lateral ventricles (Fig. 3f–h). While DAT-SPECT showed dopaminergic denervation (Fig. 3i), cardiac MIBG-SPECT findings were normal. All gait parameters were improved by 10% or more after the spinal tap compared with those at baseline, but their improvement was less than 10% compared with those after the sham spinal tap (Fig. 3j). The MDS-UPDRS part III scores did not change after the spinal tap.
Discussion
In our study, patients with PSP responded to the spinal tap more often than control patients, and some of their gait parameters were significantly improved following the spinal tap. Notably, patients with PSP with a high DESH score (≥ 5) or with abnormal EI > 0.30 and abnormal CA at the posterior commissure < 90°, which serves as an indicator of iNPH-like MRI features, tended to show a higher response rate to the spinal tap in some gait parameters. Based on these results, it is possible that gait disturbances in certain patients with PSP, particularly those with iNPH-like MRI features, tend to respond favorably to spinal taps.
It should be noted that the improvement in gait parameters observed in patients with PSP may also be attributed to the placebo effect. In our study, patients with PSP responded to the sham spinal tap more often than control patients (Table 3). In Fig. 3, Case 2 did not show improvement in gait parameters exceeding 10% after the spinal tap compared to those after the sham tap, and he did not undergo a shunt operation. In contrast, Case 1, who improved gait parameters after the spinal tap beyond the placebo effect, also responded to the shunt operation. This patient presented with iNPH-like MRI features with a high DESH score, abnormal EI > 0.30, and small CA at the posterior commissure < 90°. It is conceivable that the shunt operation effectively alleviates gait disabilities in patients with PSP who have iNPH-like MRI features and who respond to the spinal tap surpassing the placebo effect.
Several previous studies have shown that the placebo effect may be associated with improved clinical symptoms in patients with iNPH following a spinal tap or shunt operation [11, 13]. In our study, although 92% of the patients with iNPH responded to the spinal tap, 67% responded to the sham spinal tap, indicating that the placebo effect, at least in part, contributed to the improvement in gait performance among some patients with iNPH. The sham spinal tap may be useful in preventing overestimating the effects of the spinal tap. In a cohort of iNPH patients having shunt operations (Table 6), the two patients who responded to the shunt operation also responded to the spinal tap beyond the placebo effect. However, the other two patients who did not respond to the shunt operation also did not respond to the spinal tap beyond the placebo effect. Therefore, a sham spinal tap may also be helpful to avoid unnecessary shunt operations.
The definition of “responder” may have an impact on the results of our study. We used a cut-off value of 10% improvement in the gait parameter to classify responders after each test compared to baseline [30]. A recent Japanese guideline on iNPH suggested that a cut-off value of 10% could result in more false positives for the spinal tap in patients with iNPH. According to Yamada et al., a reduction in TUG total time by more than 5 s was reported to be more specific for identifying those who responded to the shunt operation. However, it is not sensitive enough to detect shunt responders with mild gait disturbance [39]. Therefore, the appropriate criteria for defining a spinal tap responder who will respond positively to shunt operations have not yet been established. On the contrary, a review study conducted by Mihalj et al. demonstrated that the sensitivity of the spinal tap in predicting shunt response was only 58% [12], suggesting that a negative response to the spinal tap does not necessarily exclude these patients from being suitable candidates for the shunt operation. To supplement this low sensitivity of the spinal tap, we used a cut-off value of 10% improvement for multiple gait measures and defined the responder as those who showed improvement in at least one gait parameter.
Many reports have assessed cognitive function in patients with iNPH before and after the spinal tap using the MMSE total score [40,41,42,43] and have suggested that the MMSE total score improved following the spinal tap [40]. However, the MMSE can be influenced by a learning effect [44] and evaluate limited cognitive domains. In this study, we employed the RBANS, designed to avoid the learning effect, and conducted a comprehensive neurocognitive assessment by thoroughly evaluating all cognitive domains of the participants. Unlike the gait function, although some patients with PSP showed improvements in cognitive function following the spinal tap, there was no significant difference in the ratio of tap responders regarding cognitive function among the groups. Together, cognitive function may be, at least in part, improved after the spinal tap test in patients with PSP, but this remains to be confirmed.
Our study had several limitations. First, it enrolled a limited number of patients, particularly those who underwent shunt surgery. A larger prospective study that enrolls more patients with PSP and definite iNPH patients is necessary to validate our findings. Second, all patients were diagnosed clinically, and they were not pathologically confirmed. However, to ascertain the pathological background, we conducted DAT-SPECT and cardiac MIBG-SPECT in all patients with PSP and 11 of the 12 patients with iNPH, supporting our diagnosis. Moreover, patients with PSP-RS who comprise most of our study cohort showed higher clinicopathological correlations [45], and therefore, we expect that the diagnosis of PSP is reasonably valid. Finally, it is noteworthy that our control patients had diverse etiologies, and their responses to spinal taps were unknown. However, we could not include healthy elderly individuals in the spinal tap test because of ethical concerns.
Data availability
Investigators may request access to anonymized data that was used in this study. Before using the data, proposals must be approved by the Institutional Review Boards at Tokyo Medical and Dental University Hospital.
References
Steele JC, Richardson JC, Olszewski J (1964) Progressive supranuclear palsy. A heterogeneous degeneration involving the brain stem, basal ganglia and cerebellum with vertical gaze and pseudobulbar palsy, nuchal dystonia and dementia. Arch Neurol 10:333–359
Colosimo C, Bak TH, Bologna M et al (2014) Fifty years of progressive supranuclear palsy. J Neurol Neurosurg Psychiatry 85(8):938–944
Starr BW, Hagen MC, Espay AJ (2014) Hydrocephalic Parkinsonism: lessons from normal pressure hydrocephalus mimics. J Clin Mov Disord 1:2
Ohara M, Hattori T, Yokota T (2020) Progressive supranuclear palsy often develops idiopathic normal pressure hydrocephalus-like magnetic resonance imaging features. Eur J Neurol 27(10):1930–1936
Adams RD, Fisher CM, Hakim S et al (1965) Symptomatic occult hydrocephalus with “normal” cerebrospinal-fluid pressure. A treatable syndrome. N Engl J Med 273:117–126
Espay AJ, Da Prat GA, Dwivedi AK et al (2017) Deconstructing normal pressure hydrocephalus: Ventriculomegaly as early sign of neurodegeneration. Ann Neurol 82(4):503–513
Magdalinou NK, Ling H, Smith JD et al (2013) Normal pressure hydrocephalus or progressive supranuclear palsy? A clinicopathological case series J Neurol 260(4):1009–1013
Klassen BT, Ahlskog JE (2011) Normal pressure hydrocephalus: how often does the diagnosis hold water? Neurology 77(12):1119–1125
Curran T, Lang AE (1994) Parkinsonian syndromes associated with hydrocephalus: case reports, a review of the literature, and pathophysiological hypotheses. Mov Disord 9(5):508–520
Nakajima M, Yamada S, Miyajima M et al (2021) Guidelines for Management of Idiopathic Normal Pressure Hydrocephalus (Third Edition): Endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurol Med Chir (Tokyo) 61(2):63–97
Saper CB (2017) Is there even such a thing as “Idiopathic normal pressure hydrocephalus”? Ann Neurol 82(4):514–515
Mihalj M, Dolić K, Kolić K et al (2016) CSF tap test - Obsolete or appropriate test for predicting shunt responsiveness? A systemic review J Neurol Sci 362:78–84
Gupta A, Lang AE (2011) Potential placebo effect in assessing idiopathic normal pressure hydrocephalus. J Neurosurg 114(5):1428–1431
Synek V, Reuben JR, Du Boulay GH (1976) Comparing Evans’ index and computerized axial tomography in assessing relationship of ventricular size to brain size. Neurology 26(3):231–233
Ishii K, Kanda T, Harada A et al (2008) Clinical impact of the callosal angle in the diagnosis of idiopathic normal pressure hydrocephalus. Eur Radiol 18(11):2678–2683
Höglinger GU, Respondek G, Stamelou M et al (2017) Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov Disord 32(6):853–864
Goetz CG, Tilley BC, Shaftman SR et al (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23(15):2129–2170
Kubo Y, Kazui H, Yoshida T et al (2008) Validation of grading scale for evaluating symptoms of idiopathic normal-pressure hydrocephalus. Dement Geriatr Cogn Disord 25(1):37–45
Hattori T, Ohara M, Yuasa T, et al. (2023) Correlation of callosal angle at the splenium with gait and cognition in normal pressure hydrocephalus. J Neurosurg 1–11
Shinoda N, Hirai O, Hori S et al (2017) Utility of MRI-based disproportionately enlarged subarachnoid space hydrocephalus scoring for predicting prognosis after surgery for idiopathic normal pressure hydrocephalus: clinical research. J Neurosurg 127(6):1436–1442
Quattrone A, Sarica A, La Torre D et al (2020) Magnetic resonance imaging biomarkers distinguish normal pressure hydrocephalus from progressive supranuclear palsy. Mov Disord 35(8):1406–1415
Kahraman D, Eggers C, Schicha H et al (2012) Visual assessment of dopaminergic degeneration pattern in 123I-FP-CIT SPECT differentiates patients with atypical parkinsonian syndromes and idiopathic Parkinson’s disease. J Neurol 259(2):251–260
Davidsson A, Georgiopoulos C, Dizdar N et al (2014) Comparison between visual assessment of dopaminergic degeneration pattern and semi-quantitative ratio calculations in patients with Parkinson’s disease and Atypical Parkinsonian syndromes using DaTSCAN® SPECT. Ann Nucl Med 28(9):851–859
Tossici-Bolt L, Hoffmann SM, Kemp PM et al (2006) Quantification of [123I]FP-CIT SPECT brain images: an accurate technique for measurement of the specific binding ratio. Eur J Nucl Med Mol Imaging 33(12):1491–1499
Orimo S, Suzuki M, Inaba A et al (2012) 123I-MIBG myocardial scintigraphy for differentiating Parkinson’s disease from other neurodegenerative parkinsonism: a systematic review and meta-analysis. Parkinsonism Relat Disord 18(5):494–500
Treglia G, Cason E, Stefanelli A et al (2012) MIBG scintigraphy in differential diagnosis of Parkinsonism: a meta-analysis. Clin Auton Res 22(1):43–55
Tateno F, Sakakibara R, Kishi M et al (2011) Sensitivity and specificity of metaiodobenzylguanidine (MIBG) myocardial accumulation in the diagnosis of Lewy body diseases in a movement disorder clinic. Parkinsonism Relat Disord 17(5):395–397
Hori K, Mao Y, Ono Y et al (2019) Inertial Measurement Unit-Based Estimation of Foot Trajectory for Clinical Gait Analysis. Front Physiol 10:1530
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148
Ishikawa M, Yamada S, Yamamoto K (2016) Early and delayed assessments of quantitative gait measures to improve the tap test as a predictor of shunt effectiveness in idiopathic normal pressure hydrocephalus. Fluids Barriers CNS 13(1):20
Nasreddine ZS, Phillips NA, Bédirian V et al (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699
Matsui M, Kasai Y, Nagasaki M (2010) Reliability and validity of the Japanese version of the repeatable battery for the assessment of neuropsychological status [in Japanese]. Toyama Med J 21:31–36
Goodglass H, Kaplan E (1972) Assessment of aphasia and related disorders. Lee & Febiger, Philadelphia
Wilson BA, Alderman N, Burgess PW et al (1996) Behavioural assessment of the dysexecutive syndrome. Bury St. Thames Valley Test Company, Edmunds, England
Benton AL, Hamsher K, Sivan AB (1976) Multilingual aphasia examination. AJA Associates, Iowa city
Reitan RM (1955) The relation of the trail making test to organic brain damage. J Consult Psychol 19(5):393–394
Dalrymple-Alford JC, Livingston L, MacAskill MR et al (2011) Characterizing mild cognitive impairment in Parkinson’s disease. Mov Disord 26(4):629–636
Litvan I, Goldman JG, Tröster AI et al (2012) Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society Task Force guidelines. Mov Disord 27(3):349–356
Yamada S, Ishikawa M, Miyajima M et al (2017) Timed up and go test at tap test and shunt surgery in idiopathic normal pressure hydrocephalus. Neurol Clin Pract 7(2):98–108
Schmidt H, Elster J, Eckert I et al (2014) Cognitive functions after spinal tap in patients with normal pressure hydrocephalus. J Neurol 261(12):2344–2350
Lee WJ, Wang SJ, Hsu LC et al (2010) Brain MRI as a predictor of CSF tap test response in patients with idiopathic normal pressure hydrocephalus. J Neurol 257(10):1675–1681
Naito H, Sugimoto T, Kimoto K et al (2021) Clinical comorbidities correlated with a response to the cerebrospinal fluid tap test in idiopathic normal-pressure hydrocephalus. J Neurol Sci 430:120024
Ishikawa M, Hashimoto M, Mori E et al (2012) The value of the cerebrospinal fluid tap test for predicting shunt effectiveness in idiopathic normal pressure hydrocephalus. Fluids Barriers CNS 9(1):1
Galasko D, Abramson I, Corey-Bloom J et al (1993) Repeated exposure to the Mini-Mental State Examination and the Information-Memory-Concentration Test results in a practice effect in Alzheimer’s disease. Neurology 43(8):1559–1563
Boxer AL, Yu JT, Golbe LI et al (2017) Advances in progressive supranuclear palsy: new diagnostic criteria, biomarkers, and therapeutic approaches. Lancet Neurol 16(7):552–563
Acknowledgements
The authors thank Taiki Matsubayashi, MD, PhD, and Satoko Kina, MD for collecting gait data, Nobuo Sanjo, MD, PhD, Yui Nosaki, Miki Yoshitake, and Meiko Hirai for collecting neuropsychological data, and the clinical staff members in our hospitals for taking care of patients.
Funding
This research was supported by the Nakayama Foundation for Human Science and Taiju Life Social Welfare Foundation.
Author information
Authors and Affiliations
Contributions
MO, TH, and TY contributed to the conception and design of the study; MO, TH, QC, KS, KH, and MM contributed to the acquisition and analysis of data; MO and TH contributed to drafting the text or preparing the figures.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Ohara, Dr. Chen, Dr. Shimano, Dr. Hirata, Dr. Matsui, and Dr. Yokota declare no conflict of interest associated with this manuscript. Dr. Hattori has received speaker’s honoraria from Daiichi Sankyo Company, Limited; Sumitomo Dainippon Pharma Co., Ltd.; and Kyowa Kirin Co., Ltd.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ohara, M., Hattori, T., Chen, Q. et al. Is there a spinal tap responder in progressive supranuclear palsy? The first prospective study. J Neurol 271, 4473–4484 (2024). https://doi.org/10.1007/s00415-024-12391-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-024-12391-4