Abstract
Freezing of gait (FOG) is an episodic gait disturbance that is commonly seen in Parkinson’s disease (PD). To date, treatment efficacy is limited. We tested the hypothesis that an intervention that utilizes motor learning provided through intensive cueing can alleviate this symptom. Fifteen subjects with PD suffering from FOG participated in a 6 week progressive motor learning program (three training sessions per week—open trial). A training session included FOG-provoking situations (e.g., turns). Prior to each presumed FOG provocation (e.g., just before a turn), rhythmic auditory stimulation (RAS) was elicited and the subject was trained to walk rhythmically, coordinate left–right stepping and to increase step size, utilizing the RAS cueing. Net training duration increased from week to week and secondary cognitive tasks while walking were added to increase FOG propensity. FOG symptom burden was assessed before, immediately, and 4 weeks after the training period. The mean number of FOG episodes (±SEM) per 10 m of walking in a standardized gait assessment decreased from 0.52 ± 0.29 in the pre-testing to 0.15 ± 0.04 in the post-testing (p < 0.05). The duration of FOG episodes decreased from 4.3 ± 2.1 to 2.6 ± 0.6 s (p < 0.05). Additional measures (e.g., FOG questionnaire, gait speed) varied in their responsiveness to the treatment. These effects were retained 4 weeks after the training. The results of this open label study support the possibility that a motor learning-based intervention is apparently effective in reducing FOG burden, suggesting that RAS can deliver ‘anti-FOG’ training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Freezing of gait (FOG) is an episodic phenomenon seen among persons with Parkinson’s disease (PD) and with parkinsonian syndromes [1, 2]. About 50 % of all patients with PD experience FOG, 10 % of PD patients with mild symptoms and 80 % of the patients with severe symptoms [1, 3]. During a FOG episode the patient experiences a sudden and transient inability to move effectively. The etiology and pathophysiology of the phenomenon are not fully understood (for recent reviews, see [4, 5]).
Several studies have demonstrated that the gait pattern in between FOG episodes is altered in PD patients who experience FOG (PD + FOG), compared to PD patients who do not [6–10]. For example, impaired gait rhythmicity [6], a continuous decrease in step length [7] and impaired ability to coordinate left–right anti-phase stepping [10], were implicated with high FOG propensity. These findings have led to the idea that FOG occurs when the gait alterations associated with FOG exceed a certain threshold [11]. If the time course of gait deterioration can be interrupted, FOG propensity may be reduced (cf., the heuristic depiction of this concept in [11]). This idea suggests that there might be a therapeutic window in which FOG can be ameliorated.
Freezing of gait episode appears more often in the OFF state, when the medication effect wears off. Still, the common pharmacological treatment in PD such as levodopa [12] and Botulinum toxin injections [13] are not optimally effective for managing FOG. Results from some intriguing pilot studies suggest that FOG may be responsive to deep brain stimulation (DBS) in non-traditional stimulation regimes [14]; however, in general, DBS typically does not provide symptom relief [15–17]. Thus, FOG is often considered to be unresponsive to current treatment options.
Physical therapy (PT)-based interventions for treating FOG are also not generally effective. Recently, treadmill training which alleviated gait asymmetry [18] was found to be effective in reducing the FOG burden as reflected by scores on the FOG questionnaire [19]. Two case studies reported that repetitive robot-assisted treadmill training may reduce FOG [20, 21]. Still, evidence supporting the efficacy of practical therapeutic options is lacking.
External sensory cueing is an effective method for ad-hoc overcoming of a FOG episode. Visual cues, such as a stick placed on the floor in front of the frozen patient, or a stripe taped to the floor, can help the patient become free from the FOG episode by triggering an ability to generate a step forward [22, 23]. Many studies demonstrated that auditory cueing in the form of rhythmic auditory stimulation (RAS) is effective in improving gait disturbances in PD. For example, Rochester et al. [24] demonstrated that cued gait training improves gait performance in PD and that the improvement is transferred to gait in the absence of cueing and even various complex conditions. However, the ability of RAS to ameliorate FOG has not been demonstrated [25].
Contrary to early thinking, motor learning apparently can be achieved in PD. For example, Mirelman et al. [26] demonstrated that progressive and intensive treadmill training combined with virtual reality can induce motor learning processes that improve gait in PD during complex, challenging conditions. Since RAS has known immediate beneficial impacts on gait in PD [25, 27, 28], we decided to use RAS as a vehicle to deliver a motor learning-based rehabilitation program to address FOG in PD.
We hypothesized that an intervention program based on motor learning principles with RAS as the means of imparting procedural learning can reduce the FOG burden in subjects with PD. To test this idea, we employed RAS in an open-loop, feed-forward manner whenever a subject encounters a FOG-provoking condition in order to avoid the impending episode in a 6-week training program.
Methods
Participants
Subjects with PD were recruited to participate in the study in which we assessed the efficacy of a 6 week progressive gait training program (open trial). The subjects were referred by the Movement Disorders Unit (MDU) at the Tel Aviv Sourasky Medical Center.
They were included if they:
-
1.
Were able to walk unassisted for at least 5 min;
-
2.
Suffer from the FOG symptom. For this criterion a screening threshold was based on the response to the question “Do you feel that your feet get glued to the floor while walking, making a turn or when trying to initiate walking?” (Question #3 from the original FOG-Q [19]. If the answer was “at least once a day”, they were invited to the second stage of screening, which was based on a short, performance-based test of FOG that includes FOG-provoking conditions (e.g., turns, doorways). Subjects who exhibited two or more FOG episodes during this trial were included. This relatively stringent inclusion criterion was needed to avoid ceiling or floor effects;
-
3.
Were free of serious co-morbidities or acute illness that would make training inappropriate.
-
4.
Did not have brain surgery of any kind, including implantation of electrodes for DBS.
The study was approved by the Human Studies Committee of Tel Aviv Sourasky Medical Center. All subjects provided informed written consent prior to entering the study.
Intervention protocol
Rationale
The goal of the training program was to generate ‘conditional’ response that will improve three gait features that are known to be associated with FOG: gait rhythmicity, step scaling and bilateral coordination of stepping. Conditioning the improved response was done with the use of RAS. Therefore, the subjects were intensively exposed to gait situations that are likely to invoke freezing (see Fig. 1).
Schemes of the different gait training tasks. Double head arrows indicate places where RAS was started. Gait training based on schemes a–c, was performed in a quiet and isolated gait lab in weeks 1 and 2 of the training sessions. a Back and forth straight line walking. These tasks were performed without (top) and with narrow passage (middle panel). As seen in the lower panel, the narrow passage was a metal frame that could be quickly rolled in or out the path by wheels. Frame width could vary between 70 and 90 cm. On both sides of the frame, black drapes served as ‘wings’ that obstructed the view of the corridor, thus creating the illusion of moving from one space to another by going through the passage. b ‘Slalom walking trials’. Small plastic ‘bowling pins’ like objects were put in the trajectory and the subjects slalomed between them. These trials were performed in the presence and the absence of the same narrow passage as in a (not shown). Dashed lines indicate the reversed trajectory (with gray, rather than black, double arrows indicating the places for RAS activation in the reversed trajectories). c Circling a chair. d Office space site for training. Small circles represent placing of slalom walking trail which described in (b). Thick bar represents narrow passage placing. In this site 90° turning (dashed line) and entering and exiting rooms were trained as well. e Incorporating training in semi daily living conditions was achieved by adding ‘hospital tour’. The site described in d is designated as ‘gait lab’. With accordance to individual endurance and fatigue subjects walked the main corridor only, or preformed full indoor and outdoor ‘tour’ within the medical center premises. In this panel think lines represent the external walls of the Tel Aviv Sourasky Medical Center north wing. In addition to fixed places (e.g., in the places marked by double headed arrows), RAS was also elicited when subjects encountered crowds
Motor learning mechanism
During the training sessions, whenever the subject crossed pre-defined spots in the training path (i.e., spots in the path that are likely to provoke FOG episodes, recall Fig. 1), the trainer started a metronome that provided RAS to earphones worn by the subjects. This was achieved using a wireless controller (the subjects were not aware to the existence of small marks on the floor and the walls designating RAS triggering points). RAS lasted for 5 s unless a FOG episode actually occurred. In that case, the RAS lasted 5 s after the termination of the FOG episode. The subjects were taught to respond to the metronome sound in the following manner: (1) To synchronize the stepping pace with the RAS rhythm; (2) To take larger steps (i.e., increase step length); and (3) To coordinate the left–right phasing in an anti-phased manner (achieved by side to side weight shifting). These three tasks were taught stepwise and not as triple task. First the subjects were trained to synchronize the stepping rhythm with the RAS, then to scale up stride size. These two features were trained in the first 2 weeks. At the start of week #3 we began training the task of improving left–right coordination.
Training sessions structure and syllabus
Three weekly training sessions carried out over 6 consecutive weeks formed the intervention program. The training sessions were designed according to the following principles: (a) Progressive training, i.e., increasing the frequency of gait situations with high probability for freezing and the training time from session to session; (b) Incorporating daily living conditions during the training, for example, by having the subject carry a tray with a glass filled with water, or by walking in crowded corridors and halls. The introduction of a cognitive task (e.g., serial 3 subtraction, naming) was also used to increase the propensity to freezing and to imitate real-life attention diversions during walking. (c) Individual adjustments: during the training sessions, the trainer identified situations that were more likely to cause freezing in each individual. These situations were given extra weight in the individual’s training program.
To add training elements that target daily living conditions and not only ‘sterile’ laboratory conditions, the site in which training took place varied as training progressed (see Fig. 1). In the first and second weeks, the subject was trained in an isolated gait laboratory. In this stage, the required response to RAS was trained. In weeks 3–4, the training took place in a quiet office area, i.e., our laboratory’s office area. A similar corridor space to the one used in the isolated gait laboratory in weeks 1–2 was used (see Fig. 1d). However, this time the subject was also exposed to occasional passing of other people, doors opening, and other office activity. In weeks 5–6, training also took place in the general hospital corridors where the walking space was more crowded and daily activities were performed, e.g., entering stores in the hospital lobby (see Fig. 1e). Table 1 describes the content of the training session in greater detail.
All training sessions were conducted during the “ON” stage of the anti-parkinsonian medication cycle, approximately in the middle third of the interval between two consecutive intakes. Prior to each training session, the trainer practiced large, paced and bilaterally coordinated steps with the RAS. The RAS frequency was individually determined for each subject based on his/her regular cadence during locomotion. At the beginning of the first week, RAS frequency was initially set to 80 % of the cadence, then the frequency was slightly adjusted so each patient could utilize the RAS comfortably to alter his/her gait pattern. At the beginning of every training week, the RAS frequency was adjusted as needed.
Efficacy assessment
Subjects who met the criteria for participation were scheduled for 6 weeks training, and for three assessments in three different times: (1) 2–3 days before the training program started (‘PRE’); (2) 2–3 days after they completed the 6 weeks program (‘POST’); and (3) about 4 weeks after they completed the training program (4W) (in a couple of cases no later than 6 weeks after the completion of the intervention).
The PRE assessments included a full medical history, history of falls, signs and symptoms of the disease, the Unified Parkinson’s disease Rating Scale (UPDRS; [29]) and The Montreal Cognitive Assessment (MoCA, [30]) to assess cognitive state. The above assessments served for describing the background clinical state of the participants. The remainder of the examination was the same in all three evaluation appointments (i.e., PRE, POST, 4W) and included:
-
1.
Fully controlled gait trials: (a) 76 m straight line walking, back and forth (2 × 38 m) within a 50 m long × 2 m wide corridor; (b) same path while performing dual tasking (DT), i.e., subtracting serial 3 s (S3, e.g., 500, 497, 494…); (c) 10 laps of figure 8 shaped trajectory. Each lap is approximately 10 m long. (d) 10 laps of figure 8 shaped trajectories + S3. During the fully controlled gait trials no RAS was presented at any time to the subjects, earphones were not worn, and the metronome was not present.
-
2.
Short FOG and festination assessment [31]. This is a recently proposed assessment protocol. Briefly, the subjects are requested to perform a continuous sequence of short walking related tasks (e.g., turning in place within 40 × 40 cm rectangle marked on the floor, walking 1 and 2 m straight line segments). These gait related tasks also combine functional elements such as opening a door or multi levels of dual tasking, e.g., carrying a tray. The scoring of the performance reflects FOG, shuffled gait and festination. Thus, higher scores (range 0–36) indicates worse performance (see [31] for further details). During the short FOG and festination assessment no RAS was presented at any time to the subjects, earphones were not worn, and the metronome was not present.
-
3.
The gait trials and the short FOG and festination assessments were videotaped. To minimize distractions, during the figure 8 shaped and the short FOG and festination assessments the video camera was placed on a tripod, while during the corridor walking the camera man was following from far behind the subject using the zoom in mode in order to stay well outside the field of view of the subject.
-
4.
The new Freezing of Gait Questionnaire (NFOG-Q) A subjective measure of FOG symptom severity in people with Parkinsonism [32].
-
5.
Clinical and functional assessments: (a) the motor part of the UPDRS (part 3; UPDRS-III); (b) The Timed Up and Go (TUG) test of mobility [33, 34]; (c) The 39-item Parkinson’s Disease Questionnaire (PDQ-39) [35] which is used to assess quality of life (QOL); (d) Activities-specific Balance Confidence (ABC) scale to assess fear of falling [36] (e) Geriatric Depression Scale (GDS).
The PRE, POST, and 4W testing sessions were preformed while the subjects were in the “ON” state. We tried to start the testing of the POST and 4W evaluations at the same time with respect to medication intake as in the PRE evaluation. We monitored and found that drug prescriptions were not changed for any of the participants during the ~10 week study period. The subjects were also asked prior to the beginning of the study not to add, change or quit any other form of therapy activity (e.g., hydrotherapy).
Outcome measures
Primary outcomes
Frequency and duration of FOG episodes were determined for each walking condition in all three (PRE, POST, 4W) assessments by post hoc video analysis. Three assessors scored the videos using a set of predetermined, standardized and performance-based criteria, as previously described [37]. The assessors (MB, SS, MD) were not blinded to the testing, and in general there was minimal overlap between the tests that they assessed, and they consulted with each other when needed. To control for effects of participant fatigue that may vary between subjects and, at times, within subjects between the PRE, POST and 4W assessments, the following steps were also taken:
-
(a)
If the subject requested to stop in the PRE assessment prior to completing 10 laps of figure 8 shaped trajectories (with or without DT), then in the POST and in the 4W assessments, he/she would be stopped after performing a similar number of laps as in the PRE assessment in the corresponding condition.
-
(b)
The FOG frequency and FOG duration outcome measures were standardized as follows. FOG frequency (number of FOG episodes per 10 m) was calculated per walk as a function of the total number of FOG episodes and the distance walked [=number of FOG episodes/(distance walked/10)]. Similarly, average FOG episode duration was calculated based on the total FOG duration and the number of FOG episodes.
Secondary outcomes
-
(1)
FOG related outcomes: (a) The short FOG and festination assessment score [31]; (b) The new FOG questionnaire NFOG-Q score [32].
-
(2)
General gait performance outcomes: (a) Gait speed was calculated based on the video inserts. The distance covered, as was measured from pre-assigned landmarks on the walking path, was divided by the time to traverse that path, excluding the time duration of the freezing episodes; (b) TUG score; (c) ABC score.
-
(3)
Background clinical measures: (a) UPDRS-III; (b) PDQ-39; (c) GDS.
Statistical analysis
To test the study hypotheses we used non-parametric statistics. The Friedman’s two-way ANOVA by ranks (three conditions: PRE, POST and 4W) was used. If there was a significant effect, post hoc comparisons were made between each pair of conditions. A p value of less than or equal to 0.05 (two sided) was considered statistically significant.
Results
Patients: screening and compliance with training
Thirty-one subjects were referred by the neurologists of the MDU to the research team. All of these patients met the first stage of the screening based on the threshold with respect to their freezing burden, but only 18 passed the second stage and entered the study and started training. Thirteen subjects did not exhibit two or more FOG episodes during a short, performance-based test that includes FOG-provoking conditions and were not invited to continue to training (see inclusion criteria above). Among the 18 subjects who passed the first and second stages of the screening, one subject dropped out from the study before completing the intervention due to a leg injury unrelated to the trial. Two others dropped out due to low motivation. Among the 15 subjects who completed the protocol, adherence to training was high; these 15 patients completed all training sessions. All 15 subjects also completed the PRE and POST assessments, but one did not perform the 4W assessment. There were no problems with fatigue or exhaustion, no adverse events of any kind, and no treatment related complaints by these patients. Baseline characteristics of these are detailed in Table 2.
The effect of the training on freezing of gait
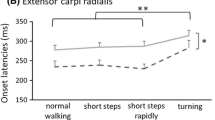
Figure 2 and Table 3 detail the FOG related outcome measures as recorded in the PRE, POST and 4W. FOG burden was significantly reduced as expressed by lower frequency of FOG episodes (p = 0.003) and the shorter duration of a FOG episode (p = 0.01) during the experimental gait trials. Figure 2 depicts data combined from all gait trials. It can be seen (Fig. 2a) that the frequency of the FOG episodes was reduced significantly in the post-testing (0.15 ± 0.04 [SEM] episodes per 10 m walking) as compared to the pre-testing (0.52 ± 0.29 [SEM] episodes per 10 m walking). FOG episodes occurrences remained significantly reduced in the 4W follow-up testing as compared to the pre-testing (0.08 ± 0.05 [SEM] episodes per 10 m walking). Similar trends were seen with regards to the mean duration of the FOG episodes (see Fig. 1b). Data presented in Table 3 suggests that these effects were observed for the straight line walking and the figure 8 shaped walking.
The effect of the intervention on the FOG burden seen during fully control gait trials. Data were combined from all gait trials, and the figure depicts group means. Error bars SEM. a Number of freezing episodes normalized to distance of 10 m long path. b Mean duration of the freezing episodes. Significant post hoc comparisons are indicated in the figures. Data from two subjects that used walking aids in the ‘Post’ assessment were omitted from the analysis
Significant improvements were observed in the results of the short FOG and festination assessment. The scores on the NFOG-Q tended to improve both in the POST and 4W assessments, but these improvements were not statistically significant (Table 3).
The effect of the training on functional gait measures and on fear of falling
The upper part of Table 4 describes the effect of the training on gait speed, TUG and on the score of the ABC questionnaire. ‘Inter-ictal’ gait speed (i.e., excluding FOG episodes periods) improved in the straight line walking, but the improvement was statistically significant only for the dual tasking trials. When tested in figure 8 shaped trajectories, only small changes in gait speed were observed. Significant improvement in the TUG performance was observed as well.
The effect of the training on background clinical measures
There was a tendency for improvement in the UPDRS-III scores. Similar UPDRS-III scores were recorded immediately after the training and 4 weeks after. No statistically meaningfully changes were seen in the PDQ-39 and GDS Scores (lower part of Table 4).
Correlation analyses in relation to the PRE and POST assessments suggest that improvements in FOG burden as expressed by the differences in the mean FOG duration and FOG frequency per 10 m, were highly correlated with the improvements in the TUG assessment (i.e., as expressed by the difference between the TUG scores; Spearman’s ρ > 0.884; p < 0.001), but not with the clinical improvements as expressed by the UPDRS-III (non-significant inverse correlation).
Discussion
Summary of findings
The intervention significantly reduced the FOG burden (i.e., frequency and duration of FOG episodes, c.f. Table 3; Fig. 2), as measured in a standardized gait trails, and in the short FOG and festination assessment [31]. There was a decrease in the NFOG-Q scores, but this decrease was not statistically significant. Improvements were also expressed in functional gait measurements such as gait speed and performance on the TUG tests, which are common improvements seen after intensive PT intervention involving gait training. No benefits were detected in clinical measures and on the level of confidence in balance performance (ABC scores).
Interpretation of findings
The present study demonstrates that the FOG burden, as measured quantitatively in laboratory settings, decreases in response to the motor learning-based intervention that was used in the present study. There is, however, a discrepancy between the objective improvements in the standardized gait trials and in the short FOG and festination assessment testing [31] in comparison to the non-significant changes in the subjective NFOG-Q scores, an assessment based on self-report. This discrepancy warrants addressing the likelihood that: (a) while the treatment improved gait performance (e.g., TUG and gait speed), and as a consequence decreased FOG propensity [11], it did not eliminate the symptom; (b) since the FOG symptom is so debilitating, the subjects might have the tendency to subjectively under estimate the improvements. A third possibility is that the longer and more intensive training is needed to impact the ingrained perceptions and to reduce freezing of gait propensity in the home environment, where multiple factors likely contribute to and predispose to FOG.
While improvements in TUG test are in agreement with the improvements in gait speed, the correlation between the improvements in TUG scores and the reduction in FOG duration and FOG frequency can be explained by the fact that FOG episodes, if they occur during the TUG testing, will cause lengthening of the TUG score. Thus, the improvement in FOG propensity will also contribute to the improvement in the TUG scores. The lack of correlation between the improvements in the FOG burden and the reductions in the UPDRS-III scores suggest that the latter are an independent consequence of the 6 week training program. The 4 weeks’ retention of many of the treatment gains is in agreement with earlier studies on the effects of motor learning in PD [26].
External cueing and motor learning
The study described here is, to our knowledge, the first to evaluate the use of procedural motor learning strategies for the training of patients with PD who suffer from freezing of gait (FOG) to avoid freezing and thus reduce the burden of this symptom. We aimed to equip the trainees with locomotion strategies so that they will be able to avert approaching FOG episodes. In other words, the study was designed to train the central nervous system to modify the gait pattern in situations that typically lead to FOG.
This study also introduces, what we believe is, a sophisticated use of external cueing in the form of RAS in order to alter the gait pattern in such a way that gait deterioration that typically lead to FOG will be averted.
Here we designed a protocol based on repeated training with RAS, so that the patients will learn to deploy the ‘freezing avoiding strategy’ even in the absence of external cueing. In this regard, it is important to keep in mind that all testing was conducted without the use of a metronome, RAS or cueing from any external source. In this sense, the patient’s ability to implicitly learn new strategies to avoid FOG were assessed, not his/her ability to apply RAS. This was presumably achieved by internally triggered improvements in stride length, rhythmicity and coordination that were effectively coupled to situations with high risk of FOG with the use of RAS. It might be possible that the ‘response’ involved, in part, investing more attention to walking, possibly to increasing stride length and to improving rhythmicity and coordination.
Sensory cuing is known to be effective for improving gait in PD (for review [38]). As technology progresses, cueing may be employed in two alternative ways: miniature devices that will be worn by the subjects and will provide a cue that will improve gait. Technological prototypes have been introduced for most sensory modalities, i.e., tactile [39], visual [22], and auditory [40, 41]. Alternatively, and based on the results of the present study, we propose to utilize a sensory cueing device as a ‘vehicle’ for a motor learning process which is aimed to alleviate freezing. That is, the intervention aims to generate an implicit coupling between conditions that are likely to provoke FOG episode, and the gait enhancements which can be utilized by sensory cuing. Thus, in the trained person, whenever the locomotion control deteriorates towards the “freezing zone” (c.f., [11]), or when the sensory-motor integrative system assesses that the current walking conditions will soon bring about a FOG episode, a response is automatically put forward and FOG episode is either averted or shortened.
Implications for treatment and future directions
The training program was quite complicated, involving changes of the training sites and foci (recall Fig. 1), instrumentations (i.e., earphones) and addressing simultaneously three gait features (i.e., scaling, rhythmicity and coordination). Some of the subjects had severe disease symptoms. Despite that, and based on the compliance and positive feedback of the patients, we feel confident that such a program can be passed on to the patients in an effective manner.
While different cueing ‘tricks’ as for how to be released from a FOG episode are often used by PD patients, to the best of our knowledge, no study has demonstrated that simply explaining to the subject who suffers from FOG to increase their step length, for example, or cue themselves to do so, is effective at reducing the likelihood that FOG will occur.
Neuronal plasticity due to exercise is seen in changes in cortical excitability and representation in PD and in other neurological conditions [42–46]. We tested the effects of a 6-week training program, which is not a long period from motor learning or exercise perspective, that followed a rigorous protocol. For practical implementation, the duration of each treatment and the total number of treatments sessions may be adjusted and adding periodic “boosting” sessions should be considered, perhaps based on additional data and follow-up studies. A potential future approach for treating FOG in PD may be based on self-administered training that will be incorporated in the daily living activities of PD patients. This future training can involve externally cued assisted motor learning that will be individually tailored to the patient, based on the specific circumstances relevant to this individual, for example, what are the typical FOG ‘triggers’ for a particular subject, what is the compliance with different modalities of external cueing and what is the specific progress in training suitable for a trainee. During the laboratory stage of training, we focused on turning and narrow passages as FOG ‘triggers’. The method can be easily adjusted to the ‘start hesitation’ and ‘reaching destination’ types [37]. Still, it is important to keep in mind that freezing during turning is the most common type of FOG.
The subjects were trained and tested during the “ON” state. Most patients, however, have more FOG difficulties in the “OFF” state, so any future strategy would also need to address the more severe situation. We are optimistic that many of the gains observed in the “ON” condition will also be seen during wearing “OFF” and “OFF”. Clearly, however, this needs to be directly studied.
We did not exclude subjects with low scores on the MoCA. The one subject with relatively low score (i.e., 14), did gain from the treatment (e.g., FOG frequency reduced from 0.33 to 0.10 episodes per 10 m). Thus, since we assume that implicit motor learning is the mechanism by which improvements are gained, it is suggested that subjects that can follow the basic instructions of the therapist are suitable to participate, even if they do have cognitive impairments.
Limitations
This study has several limitations. It is an open label study and some contribution of the placebo effect cannot be ruled out. A similar group of PD subjects with FOG that would have undergone a similar exposure program but without strategy training could have been useful to address this effect. We suggest, however, that any placebo effect is minimal and does not fully explain the observed improvements. The impression of both trainers and participants was that the improvements were gradual during the course of training. This time course is consistent with the expected effects of a progressive motor leaning protocol. In addition, it is important to mention that while the initial, baseline examination was done prior to the subject’s knowledge that he/she will be trained with RAS, in the POST examination (and later in the 4W examination), the subjects were actually ‘deprived’ from the assistive measure that had been used during the course of their training. Therefore, a potential placebo linked to the RAS might be expected to lose its potency when subjects were examined after the training in the absence of RAS.
There was also considerable variability between subjects with respect to the efficacy of the treatment. Thus, one challenge is to understand which type of PD patient will benefit from the intervention. Due to the relatively small number of participants, exploring sub-types of persons with PD and their ability to benefit from the treatment was limited.
We believe that motivation is an important factor. The trainers also reported that the ability to utilize external RAS for pacing and coordinating gait varies between the participants. It remains to be determined if this impacts the level of improvement with respect to FOG.
While this study provides support for the feasibility and for the potential clinical utility, it also raises questions related to both basic and applied science. First, the results need to be further confirmed in a larger cohort, and in a different design in which a potential placebo effect can be addressed. In addition, since FOG is an elusive symptom at times during the routine clinic visits, or visits to the gait laboratory, the testing of efficacy should include home monitoring of FOG burden as a key outcome measure [40, 41, 47].
References
Giladi N, Kao R, Fahn S (1997) Freezing phenomenon in patients with parkinsonian syndromes. Mov Disord 12(3):302–305
Giladi N, McDermott MP, Fahn S, Przedborski S, Jankovic J, Stern M et al (2001) Freezing of gait in PD: prospective assessment in the DATATOP cohort. Neurology 56(12):1712–1721
Macht M, Kaussner Y, Moller JC, Stiasny-Kolster K, Eggert KM, Kruger HP et al (2007) Predictors of freezing in Parkinson’s disease: a survey of 6,620 patients. Mov Disord 22(7):953–956
Nieuwboer A, Giladi N (2013) Characterizing freezing of gait in Parkinson’s disease: models of an episodic phenomenon. Mov Disord 28(11):1509–1519
Nutt JG, Bloem BR, Giladi N, Hallett M, Horak FB, Nieuwboer A (2011) Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol 10(8):734–744
Hausdorff JM, Schaafsma JD, Balash Y, Bartels AL, Gurevich T, Giladi N (2003) Impaired regulation of stride variability in Parkinson’s disease subjects with freezing of gait. Exp Brain Res 149(2):187–194
Iansek R, Huxham F, McGinley J (2006) The sequence effect and gait festination in Parkinson disease: contributors to freezing of gait? Mov Disord 21(9):1419–1424
Nieuwboer A, Dom R, De Weerdt W, Desloovere K, Fieuws S, Broens-Kaucsik E (2001) Abnormalities of the spatiotemporal characteristics of gait at the onset of freezing in Parkinson’s disease. Mov Disord 16(6):1066–1075
Plotnik M, Giladi N, Balash Y, Peretz C, Hausdorff JM (2005) Is freezing of gait in Parkinson’s disease related to asymmetric motor function? Ann Neurol 57(5):656–663
Plotnik M, Giladi N, Hausdorff JM (2008) Bilateral coordination of walking and freezing of gait in Parkinson’s disease. Eur J Neurosci 27(8):1999–2006
Plotnik M, Giladi N, Hausdorff JM (2012) Is freezing of gait in Parkinson’s disease a result of multiple gait impairments? Implications for treatment. Parkinsons Dis 2012:459321
Bloem BR, Hausdorff JM, Visser JE, Giladi N (2004) Falls and freezing of gait in Parkinson’s disease: a review of two interconnected, episodic phenomena. Mov Disord 19(8):871–884
Sheffield JK, Jankovic J (2007) Botulinum toxin in the treatment of tremors, dystonias, sialorrhea and other symptoms associated with Parkinson’s disease. Expert Rev Neurother 7(6):637–647
Fasano A, Herzog J, Seifert E, Stolze H, Falk D, Reese R et al (2011) Modulation of gait coordination by subthalamic stimulation improves freezing of gait. Mov Disord 26(5):844–851
Stolze H, Klebe S, Poepping M, Lorenz D, Herzog J, Hamel W et al (2001) Effects of bilateral subthalamic nucleus stimulation on parkinsonian gait. Neurology 57(1):144–146
Tommasi G, Lopiano L, Zibetti M, Cinquepalmi A, Fronda C, Bergamasco B et al (2007) Freezing and hypokinesia of gait induced by stimulation of the subthalamic region. J Neurol Sci 258(1–2):99–103
van Nuenen BF, Esselink RA, Munneke M, Speelman JD, van Laar T, Bloem BR (2008) Postoperative gait deterioration after bilateral subthalamic nucleus stimulation in Parkinson’s disease. Mov Disord 23(16):2404–2406
Frazzitta G, Pezzoli G, Bertotti G, Maestri R (2013) Asymmetry and freezing of gait in parkinsonian patients. J Neurol 260(1):71–76
Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD (2000) Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord 6(3):165–170
Lo AC, Chang VC, Gianfrancesco MA, Friedman JH, Patterson TS, Benedicto DF (2010) Reduction of freezing of gait in Parkinson’s disease by repetitive robot-assisted treadmill training: a pilot study. J Neuroeng Rehabil 7:51
Ustinova K, Chernikova L, Bilimenko A, Telenkov A, Epstein N (2011) Effect of robotic locomotor training in an individual with Parkinson’s disease: a case report. Disabil Rehabil Assist Technol 6(1):77–85
Van Gerpen JA, Rucker CT, Matthews M, Saucier MA (2012) Lifting the “FOG” with laser generated visual-cueing. Neurologist 18(5):298–301
Velik R, Hoffmann U, Zabaleta H, Marti Masso JF, Keller T (2012) The effect of visual cues on the number and duration of freezing episodes in Parkinson’s patients. Conf Proc IEEE Eng Med Biol Soc 2012:4656–4659
Rochester L, Nieuwboer A, Baker K, Hetherington V, Willems AM, Chavret F et al (2007) The attentional cost of external rhythmical cues and their impact on gait in Parkinson’s disease: effect of cue modality and task complexity. J Neural Transm 114(10):1243–1248
Cubo E, Leurgans S, Goetz CG (2004) Short-term and practice effects of metronome pacing in Parkinson’s disease patients with gait freezing while in the ‘on’ state: randomized single blind evaluation. Parkinsonism Relat Disord 10(8):507–510
Mirelman A, Maidan I, Herman T, Deutsch JE, Giladi N, Hausdorff JM (2011) Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? J Gerontol A Biol Sci Med Sci 66(2):234–240
Hausdorff JM, Lowenthal J, Herman T, Gruendlinger L, Peretz C, Giladi N (2007) Rhythmic auditory stimulation modulates gait variability in Parkinson’s disease. Eur J Neurosci 26(8):2369–2375
Nieuwboer A, Baker K, Willems AM, Jones D, Spildooren J, Lim I et al (2009) The short-term effects of different cueing modalities on turn speed in people with Parkinson’s disease. Neurorehabil Neural Repair 23(8):831–836
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P et al (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23(15):2129–2170
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I et al (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699
Ziegler K, Schroeteler F, Ceballos-Baumann AO, Fietzek UM (2010) A new rating instrument to assess festination and freezing gait in Parkinsonian patients. Mov Disord 25(8):1012–1018
Nieuwboer A, Rochester L, Herman T, Vandenberghe W, Emil GE, Thomaes T et al (2009) Reliability of the new freezing of gait questionnaire: agreement between patients with Parkinson’s disease and their carers. Gait Posture 30(4):459–463
Morris S, Morris ME, Iansek R (2001) Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Phys Ther 81(2):810–818
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148
Peto V, Jenkinson C, Fitzpatrick R, Greenhall R (1995) The development and validation of a short measure of functioning and well being for individuals with Parkinson’s disease. Qual Life Res 4(3):241–248
Powell LE, Myers AM (1995) The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci 50A(1):M28–M34
Schaafsma JD, Balash Y, Gurevich T, Bartels AL, Hausdorff JM, Giladi N (2003) Characterization of freezing of gait subtypes and the response of each to levodopa in Parkinson’s disease. Eur J Neurol 10(4):391–398
Lim I, van Wegen E, de Goede C, Deutekom M, Nieuwboer A, Willems A et al (2005) Effects of external rhythmical cueing on gait in patients with Parkinson’s disease: a systematic review. Clin Rehabil 19(7):695–713
Winfree KN, Pretzer-Aboff I, Hilgart D, Aggarwal R, Behari M, Agrawal SK (2013) The effect of step-synchronized vibration on patients with Parkinson’s disease: case studies on subjects with freezing of gait or an implanted deep brain stimulator. IEEE Trans Neural Syst Rehabil Eng 21(5):806–811
Bachlin M, Plotnik M, Roggen D, Giladi N, Hausdorff JM, Troster G (2010) A wearable system to assist walking of Parkinson’s disease patients. Methods Inf Med 49(1):88–95
Bachlin M, Plotnik M, Roggen D, Maidan I, Hausdorff JM, Giladi N et al (2010) Wearable assistant for Parkinson’s disease patients with the freezing of gait symptom. IEEE Trans Inf Technol Biomed 14(2):436–446
Fisher BE, Wu AD, Salem GJ, Song J, Lin CH, Yip J et al (2008) The effect of exercise training in improving motor performance and corticomotor excitability in people with early Parkinson’s disease. Arch Phys Med Rehabil 89(7):1221–1229
Forrester LW, Hanley DF, Macko RF (2006) Effects of treadmill exercise on transcranial magnetic stimulation-induced excitability to quadriceps after stroke. Arch Phys Med Rehabil 87(2):229–234
Liepert J (2006) Motor cortex excitability in stroke before and after constraint-induced movement therapy. Cogn Behav Neurol 19(1):41–47
Petzinger GM, Fisher BE, Van Leeuwen JE, Vukovic M, Akopian G, Meshul CK et al (2010) Enhancing neuroplasticity in the basal ganglia: the role of exercise in Parkinson’s disease. Mov Disord 25(Suppl 1):S141–S145
Petzinger GM, Fisher BE, McEwen S, Beeler JA, Walsh JP, Jakowec MW (2013) Exercise-enhanced neuroplasticity targeting motor and cognitive circuitry in Parkinson’s disease. Lancet Neurol 12(7):716–726
Tripoliti EE, Tzallas AT, Tsipouras MG, Rigas G, Bougia P, Leontiou M et al (2013) Automatic detection of freezing of gait events in patients with Parkinson’s disease. Comput Methods Programs Biomed 110(1):12–26
Acknowledgments
We thank the persons who volunteered to participate for their time and effort, and Dr. Anat Mirelman for her input. This study was funded in part by the Michael J. Fox Foundation for the Research of Parkinson’s disease, and by the European Union—Seventh Framework Programme (FP7/2007-2013) under grant agreement n°288516 (CuPiD project).
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical statements
This study has been approved by the Human Studies Committee of Tel Aviv Sourasky Medical Center, and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Plotnik, M., Shema, S., Dorfman, M. et al. A motor learning-based intervention to ameliorate freezing of gait in subjects with Parkinson’s disease. J Neurol 261, 1329–1339 (2014). https://doi.org/10.1007/s00415-014-7347-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7347-2