Abstract
We discuss relevant aspects in two siblings with a neurodegenerative process of unclear aetiology who developed progressive dementia with global aphasia and hyperoral behaviour at the ages of 39 and 46 years and who died 6 and 5 years after disease onset. The cases were reported to the National Reference Center for TSE Surveillance in Göttingen, Germany. Detailed clinical examinations, CSF, blood samples, and copies of the important diagnostic tests (magnetic resonance imaging, electroencephalogram, laboratory tests) were obtained. Further neuropathological and genetic analyses were performed. Cerebral magnetic resonance imaging of both siblings showed prominent changes in signal intensity, especially in the left medial temporal cortex, but also the hippocampal formation. Neuropathological examination revealed spongiform changes, neuronal loss, and astrocytic gliosis, which are typical in Creutzfeldt–Jakob disease. However, no prion protein deposits were detectable by immunohistochemical analysis, Western blot, or PET blot, though abundant tau protein deposits were observed. A mutation in the coding region of the prion protein genes of both siblings was excluded. A detailed search of the literature revealed no other cases with a similar clinical and neuropathological appearance. While the disease aetiology remains unclear, the findings point to a neurodegenerative process and most likely a genetic disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Creutzfeldt–Jakob disease (CJD), a rare neurodegenerative disease, is the most common transmissible human spongiform encephalopathy. Sporadic CJD (sCJD), the most frequent form, is considered to account for about 85–90 % of human transmissible spongiform encephalopathies (TSE), while genetic CJD, which is associated with a mutation in the prion protein gene (PRNP), is found in about 10–15 % of European cases [9]. The most common mutations are D178N, E200K, and V210I [5, 6]. A definite diagnosis of sCJD requires histological or biochemical analysis of the brain tissue. Typical neuropathological changes are spongiform degeneration, neuronal loss, and astrocytic gliosis, as well as the accumulation of protease-resistant prion protein [8, 19].
Recently, a prion disease was reported in siblings who also lacked any mutation in the PRNP and a coincidental occurrence was discussed with regard to the cases presented in this study [20].
Here, we report on two of three siblings who developed progressive dementia with aphasia and hyperoral behaviour at the ages of 39 and 46 years, and who died within a few years after diagnosis. In both patients, cerebral magnetic resonance imaging (cMRI) showed predominant changes in signal intensity in both (left > right) temporal cortical regions. Neuropathological examination revealed spongiform degeneration, neuronal loss, and astrocytic gliosis in both siblings, mimicking Creutzfeldt–Jakob disease (CJD). However, no protease-resistant prion protein (PrPSc) was found in the brain tissue, nor was there evidence of a mutation in the coding region of the PRNP.
Case history of the sister
Clinical signs and symptoms
The first symptoms seen in the previously healthy patient occurred at the age of 39 years, when she slowly developed deficits in concentration, short-term memory, and spatial orientation. On first clinical neurological examination, cranial computerised tomography (CCT) and electroencephalogram (EEG) showed normal findings. When she developed depressive symptoms and, later in the disease, symptoms of anxiety, she was diagnosed with depression and an amnestic syndrome. In addition to developing progressive cognitive deficits, she had mild hypomimia and bradykinesia by the age of 40. The EEG demonstrated an almost rhythmic, sharp wave-like focus over the right temporal region, while CCT and brain scintigraphy were normal. Cerebrospinal fluid (CSF) analysis showed a mild pleocytosis with a leukocyte count of 7 cells/mm3, a normal total protein level, and absence of oligoclonal bands. No evidence of intracerebral IgG synthesis (IgG ratio 1.42, QAlb 3.09, IgG index 0.46), or a viral or bacterial infection was found. After high-dose intravenous prednisolone therapy, no cells were detected in the CSF, and a regression of the extrapyramidal symptoms and pathological EEG changes was observed. The patient’s memory deficits, however, continued to worsen. She had previously worked as a public school teacher, but then required care in a nursing home. At age 42, curative hysterectomy for ovarian carcinoma (T2b N1 MX) and postoperative chemotherapy were carried out. As the disease progressed, severe disorientation regarding place and time, as well as other memory deficits became increasingly apparent. Repeated CSF analyses revealed no pathological findings. However, cMRI showed a clear increase in signal intensity in the cortical areas of both temporal lobes (left more than right) (Fig. 1). At 43 years of age, the patient was completely disoriented, unresponsive, and had no spontaneous speech. In addition, urinary and stool incontinence, a reverse sleep/wake cycle, stereotypic behaviour, and symptoms of frontal lobe disinhibition such as bulimia, compulsion to collect objects, and hypersexuality developed.
At one point, a generalized epileptic seizure with focal onset in the right hemisphere was observed. Follow-up cMRI showed a pronounced increase in cortical signal intensity in the absence of contrast medium uptake (Fig. 2). CCT was read as normal. To exclude potential metabolic (e.g. Wilson’s disease, thyroid disease, vitamin deficiency) and neoplastic/paraneoplastic causes of the symptoms, CT scans of the chest, abdominal ultrasound and different blood test were performed. No pathological findings were revealed. After occurrence of a limb-kinetic apraxia, hyperoral behaviour, and “central fever” up to 40 °C, the completely aphasic patient died at the age of 45 years.
Neuropathology and genetics
Macroscopic examination of the brain (unfixed weight 1,440 g) showed only mild arterial sclerosis in the arteries of Willis. Samples for histology were obtained according to BrainNet standard [1]. Histological analysis of the cerebral neocortex revealed widespread spongiform change in the neuropil. In addition, pronounced neuronal loss and astrocytic gliosis were seen. Marked spongiform changes accompanied by gliosis and neuronal loss were also found in the dentate gyrus and the pyramidal cell layer of the hippocampus, the subiculum, and in the entorhinal cortex. In the cerebellar cortex, the Purkinje cells were relatively well preserved but the Bergmann glia showed a proliferation. No indication of inflammatory changes or atypical cells was found. For immunohistochemical prion protein analysis, the tissue was pretreated by hydrolytic autoclaving (2 mM HCl). Neither immunohistochemistry (IHC) with the monoclonal antibody (mAb) Gö138 (epitope 144–155) nor paraffin-embedded tissue (PET) blot analysis with various anti-prion antibodies (mAb 12F10: epitope 153–163 [7], mAb 3F4: epitope 109–112 (kindly provided by Michael Beekes, Robert-Koch Institute, Berlin, Germany) and mAb Gö138 [8]) revealed any PrPSc deposits in the cerebral neocortex or cerebellum [8, 19]. However, abundant tau protein deposits were found in the hippocampal formation. The examined tissue appeared to be devoid of A-beta plaques with Bielschowsky′s silver staining. Molecular genetic analysis of DNA extracted from formalin-fixed brain sections was negative for a point or an insertion mutation in the PRNP [23]. The determination of the codon 129 polymorphism of the prion protein gene of the sister could not be realized due to the lack of sample material.
Case history of the brother
Clinical findings
Five years after the sister’s onset of the disease the brother developed cognitive deficits. Since their adolescence they lived 200 km apart from each other with rare personal contact. After a 1-year history of progressive short-term memory deficits and spatial disorientation, the 47-year-old patient underwent neurological examination, which revealed normal clinical neurological findings. EEG, transcranial Doppler ultrasound, and T1- and T2-weighted cMRI were also unremarkable. At 48 years of age, the patient, who had until then worked as a numismatist, became unable to work due to concentration and sleep problems. Another cMRI examination showed slightly enlarged frontal sulci, but all other findings were normal for his age. A thorough neurological and psychiatric examination at age 49 revealed impaired orientation regarding time and place, concentration and attention deficits, and mild depression. The Mini-Mental State examination score was 25/30 points. No focal neurological deficits were found on examination. Comprehensive laboratory tests included screening for vasculitis and various viral infections, as well as CSF analysis, all of which were unremarkable. Cerebral MRI (T2-weighted images), however, demonstrated a bilateral increase in signal intensity in the region of the hippocampal formation, but no uptake of contrast medium. By the age of 51 years, his clinical symptoms had worsened, and the patient no longer recognized his family. His spontaneous speech was confined to stereotypic utterances. Global aphasia and echolalia were present. In addition, disinhibited exploration, hyperoral behaviour, and runaway tendencies were observed. Repeated CSF analyses revealed normal cell count (1/mm3), normal total protein level (311 mg/dl), normal IgG index (0.69) and absence of oligoclonal bands in CSF led to the detection of unspecific IgG autoantibodies against neuronal proteins. No 14-3-3 proteins were present, and the neuron-specific enolase (14 ng/ml; normal range <25 ng/ml), the Tau protein (412 pg/ml; normal range <450 pg/ml) and the beta-amyloid1-42—level (616 pg/ml; normal range >450 pg/ml) were just within normal range. The EEG showed low-amplitude mixed alpha/beta frequencies. A whole-body positron emission tomography (PET) scan and specific marker for tumour screening, complete blood count, electrolytes, renal, liver and thyroid values, vitamins, copper and ceruloplasmin revealed no pathological findings. However, [18F]-2-fluoro-2-deoxy-d-glucose (FDG) PET imaging revealed extensive glucose hypometabolism in the temporal region (left more than right) and in the left frontal region. Pronounced diffuse cortical increased signal with bitemporal focus and involvement of the entire hippocampus, partial bilateral involvement (left more than right) of the cortex in the frontobasal and medial temporooccipital regions, and mild involvement of the parietal cortex on the left side (Fig. 3) were seen on cMRI. Some weeks later, the patient died at 51 years of age because of staphylococcal sepsis.
Neuropathology and genetics
Histological analysis revealed marked spongiform changes in the form of small vacuoles in the cortical gray matter (Fig. 4a, b). Neuroanatomical sites had been taken according to BrainNet standard [1]. No large confluent vacuoles were seen. Parts of the cortex appeared larger than normal rather than smaller. The spongiform changes were most pronounced in the limbic cortex and less pronounced in the region of the visual cortex. In addition, moderate gliosis and slight to moderate neuronal loss were observed. Massive spongiform pathology, moderate gliosis, and moderate neuronal loss were also present in the archicortex of the hippocampal formation. Basal ganglia, thalamic nuclei, midbrain, brain stem, and cerebellum were almost unaffected by these changes. No prion protein deposits were detected by immunohistochemical analysis and PET blot with the antibodies named above. The routinely performed Western blot [21] with mAb 3F4 on frontal and occipital cortex samples, including several proteinase K concentrations, did not reveal a typical prion pattern (Fig. 5). Western blotting with mAb 1E4 (epitope 97–108) (abcam®, Cambridge, UK) with the same proteinase K concentrations confirmed the absence of a “protease-sensitive prionopathy” [3]. Additional Western blots using mAbs 12F10 and 3B5 (epitope 62–91) [7] were devoid of pathological prion protein (data not shown). Likewise, we could not detect prion aggregates with a membrane adsorption assay [21], which we use routinely in the National Reference Center for spongiform encephalopathies (Department of Neuropathology) and which comprises a sensitivity comparable to the PET blot (Wemheuer et al. to be published elsewhere).
Pathological changes in the brother. Pathological changes in the temporal cortex and hippocampus (a, b): dense spongiform changes throughout all cortical layers, nerve cell loss, but little gliosis can be seen in the temporal cortex (a H/E, bar = 500 μm; b H/E, bar = 50 μm). With the PET blot abundant distinct tau deposits are detectable in the hippocampus and temporal cortex from the brother [c mAb AT8 (Thermo Scientific, Schwerte, Germany), bar = 1 mm], but not in a tau-negative case (d cingulate gyrus, mAb AT8, bar = 1 mm)
Western blot of the frontal cortex sample of the brother with mAb 3F4. Frontal cortex of the brother (#2) is devoid of pathological prion protein as demonstrated here by Western blotting with mAb 3F4 (1:3,000). Several concentrations of proteinase K (PK) were used to digest the physiological prion protein visible in lane 3. As positive controls frontal cortex samples of two CJD cases were used: one homozygous at codon 129 (PRNP) for methionine and displaying prion type 1 (MM1), and the second with methionine/valine at codon 129 and prion type 2 (MV2) according to Parchi [15]
Furthermore the RT-QuIC (real-time quaking-induced conversion) analysis was seeded with CSF derived from the brother, a negative control and a positive (sCJD) control. The method reproduces a template-directed conformational change of PrPC to PrPSc. Using 10,000 rfu (relative fluorescence units) at 90 h, the analysis revealed a negative RT-QuIC response comparable to a non-prion disease control (Fig. 6). The RT-QuIC analysis has a sensitivity of >90 % and a specificity of approximately 98 % [10].
RT-QuIC analysis from CSF of the brother. Real-time quaking-induced conversion response from CSF seeded reactions. RT-QuIC analysis from CSF samples (LP 1 and 2) derived from the brother showed a negative RT-QuIC-response comparable to control patients without prion disease. A positive control (RT-QuIC reaction seeded with CSF from a sCJD patient) is also shown. Each point represents the mean thioflavin T fluorescence signal of three replicates
Pronounced reactive astrocytic and microglial gliosis were present in the cortical areas affected by spongiform degeneration. Abundant tau protein deposits were found in the hippocampal formation (PET blot; Fig. 4c). With immunhistochemical staining methods we found few diffuse A-beta plaques, cerebral amyloid angiopathy and single neuritic plaques corresponding to CERAD classification A [12], i.e., the lowest grading, in the cortex (mAb 6E10, Calbiochem, Germany). Molecular genetic analysis of the PRNP using the SSCP (single-strand conformational polymorphism) technique and direct sequencing showed no mutation in the coding region [23]. The full genomic sequencing of the PRNP (2 exons and 13 kb intron, 4,666,882–4,682,236 nt, chromosome 20; Reference sequence: CCDS Database CCDS13080.1) revealed only six known single nucleotide polymorphisms (SNP) within the intron without evidence to be pathogenic (rs35519959 C/T, rs1931969 G/T, rs6116471 A/G, rs4815729 A/G, rs6052769 G/T, rs6107515G/T; www.ncbi.nlm.nih.gov/SNP). To investigate whether the brother has a duplication of the PRNP gene, genomic DNA was subjected to Southern blot analysis [18]. The latter showed a ~10.3 kb single genomic fragment upon digestion of the brother DNA sample with BamHI restriction enzyme and a ~5.8 kb single genomic fragment using EcoRI restriction enzyme. These results indicate that there is no genomic duplication of PRNP.
At codon 129 of the prion protein gene, homozygosity for methionine was found. From the patient DNA sample, all coding exons and the adjacent intron regions of the MAPT (microtubule-associated protein tau) -gene were amplified by PCR and sequenced with corresponding primers [17]. A mutation in the MAPT-gene could be excluded.
Family history
In addition to the siblings described in this case report, there is a 52-year-old brother who is healthy so far. Another brother died as a young adult in a car accident. The parents died in an avalanche accident at 40 years of age. The father did not have any siblings, while the mother had three brothers. One brother died young in the war. The two other brothers, 73 and 71 years of age, respectively, do not have memory deficits. The grandparents on the mother’s side died at an old age (grandmother at 87, grandfather at 80 years of age). They were not known to have had dementia, nor were the grandparents on the father’s side (grandmother died at 80 years of age, grandfather died young in the war).
Discussion
Both siblings had a spongiform encephalopathy and died of the disease, but no abnormal PrPSc aggregates were detectable on neuropathological and biochemical examination. A mutation in the coding region of the prion protein gene was excluded. We summarized the clinical and diagnostic characteristics of the siblings in Table 1. A detailed search of the literature showed no other cases with similar clinical and neuropathological findings. The diagnosis of the patients reported here is not clear in all detail. Similarities of clinical and pathological features presented by both patients led to the assumption of a genetic disorder. Based on the spongiform changes in the cortex that were found post mortem, a prion disease was discussed. However, no PrPSc deposits were detected and no mutation was found in the PRNP. In addition, these two cases clearly differ from CJD cases in terms of clinical neurological symptoms (see below) and supplementary diagnostic findings (e.g., 14-3-3 protein negative, no increased signal of the basal ganglia, no periodic sharp wave complexes in the EEG).
With 39 and 46 years of age, the onset of the disease in our two patients was earlier compared to a median age of 66 years observed in sCJD patients [5]. The clinical symptoms of sCJD, which, according to the classification criteria [22, 24, 25], are characterized by rapidly progressive dementia with less than 2 years of duration and a neurological multisystem disorder with symptoms such as myoclonus or cerebellar ataxia, were not met at any time during the disease process in contrast to the reported siblings with a prion disease who also lacked any mutation in the PRNP [20]. Both siblings slowly developed memory deficits, especially short-term memory deficits, and spatial disorientation. After 4 and 5 years, respectively, the condition of the two patients deteriorated rapidly, resulting in complete disorientation, global aphasia, and echolalia. Later in the disease both patients showed disinhibited exploration, hyperoral behaviour, and the tendency to escape.
The disease duration in our patients (5 and 6 years, respectively) is considerably longer than in sCJD patients (6 months on average) [16]. This still holds even for young sCJD patients below 50 years of age, whose disease duration is 16 months on average [2]. Frequently, patients with familial prion diseases present an early onset of the disease and longer disease duration. Moreover, the clinical symptoms are less specific and the technical diagnostic tests are less sensitive in these patients compared to sCJD [5], but the presence of a mutation in the coding region of the PRNP of either sibling was excluded using SSCP analysis, or direct DNA sequencing [14, 23]. Furthermore in case of the brother a full genomic sequence analysis of the PRNP (specific for a 15,354 bp sequence) revealed only six known single nucleotide polymorphisms (SNP) within the intron without evidence to be pathogenic.
Recently, an analysis of variably protease-sensitive prionopathy cases without mutations in the PRNP open reading frame were published [26], but the clinical symptoms in the codon 129-MM subgroup with 71 years at disease onset (mean), a progressive motor decline with cerebellar and extrapyramidal symptoms and myoclonus and no signal changes in the MRI are not similar to our cases.
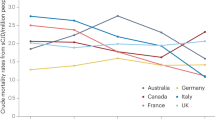
The cMRI has been included in the classification criteria for CJD [24]. Characteristic MRI lesion patterns include hyperintense signals in the basal ganglia (in particular in the caudate nucleus and putamen) and in the cortex (temporal–parietal–occipital) [11, 24]. The MRI findings of both siblings showed comparable changes with an increase in signal intensities especially in the left temporal cortical region. A comparison of the siblings’ follow-up MRI scans not only suggests that they had the same disease, but also that the changes observed originated from the cortex of the medial temporal lobe and hippocampal formation. In addition, there was no uptake of contrast medium that could have indicated inflammatory or neoplastic diseases. Although the changes seen on MRI may suggest a wide range of differential diagnoses, epileptic, ischemic, neoplastic, or inflammatory diseases can be excluded based on clinical disease course, CSF analyses, EEGs, and neuropathological findings.
Spongiform changes, gliosis, and neuronal loss did not differ in their morphological appearance from CJD changes. In CJD, too, spongiform degeneration may be pronounced, while gliosis and neuronal loss are less pronounced. Since the basal ganglia were unaffected (in neuropathological investigation and cMRI), it is not likely that the siblings had one of the known forms of CJD. Whenever marked spongiform changes are seen in the cortex of patients with CJD, the anterior striatum and putamen are also severely affected. In addition, cerebellum, midbrain, and brainstem were inconspicuous, except for the presence of mild gliosis in the pons region. Typical prion protein deposits were not detectable by immunohistochemical analysis, PET blot, Membrane Adsorption Assay or Western blot, but abundant tau protein deposits were present. Additionally, the RT-QuIC response was comparable to a nonprion disease control [10]. Patients suffering from Klüver–Bucy syndrome, which is caused by bilateral temporal lobe damage, present signs of frontal disinhibition such as hyperoral behaviour and memory deficits [4]. The clinical signs and symptoms of the patients presented here resemble those seen in frontotemporal dementia, which is defined by personality changes, apathy, and signs of frontal disinhibition such as hyperoral behaviour, impoverishment of speech and, later in the disease, development of dementia. After disease onset, mostly in the fifth decade, the disease progresses over a period of about 8 years, and in 40–50 % of these patients, the family history is positive [13]. The MAPT-gene analysis of the siblings offered no mutation.
In the two cases reported here, the disease aetiology remains unclear, but the findings support the assumption of a neurodegenerative process and most likely a genetic disease. As only the brother, but not the sister presented with few A-beta deposits in the cortex, we assume that these did not influence the clinical presentation. From a neuropathological point of a view, the disease is most likely to be classified as “familial tau-related spongiform encephalopathy”.
References
Alafuzoff I, Thal DR, Arzberger T, Bogdanovic N, Al-Sarraj S, Bodi I, Boluda S, Bugiani O, Duyckaerts C, Gelpi E, Gentleman S, Giaccone G, Graeber M, Hortobagyi T, Hoftberger R, Ince P, Ironside JW, Kavantzas N, King A, Korkolopoulou P, Kovacs GG, Meyronet D, Monoranu C, Nilsson T, Parchi P, Patsouris E, Pikkarainen M, Revesz T, Rozemuller A, Seilhean D, Schulz-Schaeffer W, Streichenberger N, Wharton SB, Kretzschmar H (2009) Assessment of beta-amyloid deposits in human brain: a study of the BrainNet Europe Consortium. Acta Neuropathol 117:309–320
Boesenberg C, Schulz-Schaeffer WJ, Meissner B, Kallenberg K, Bartl M, Heinemann U, Krasnianski A, Stoeck K, Varges D, Windl O, Kretzschmar HA, Zerr I (2005) Clinical course in young patients with sporadic Creutzfeldt–Jakob disease. Ann Neurol 58:533–543
Gambetti P, Dong Z, Yuan J, Xiao X, Zheng M, Alshekhlee A, Castellani R, Cohen M, Barria MA, Gonzalez-Romero D, Belay ED, Schonberger LB, Marder K, Harris C, Burke JR, Montine T, Wisniewski T, Dickson DW, Soto C, Hulette CM, Mastrianni JA, Kong Q, Zou WQ (2008) A novel human disease with abnormal prion protein sensitive to protease. Ann Neurol 63:697–708
Góscínski I, Kwiatkowski S, Polak J, Orlowiejska M, Partyk A (1997) The Kluver–Bucy syndrome. J Neurosurg Sci 41:269–272
Heinemann U, Krasnianski A, Meissner B, Varges D, Kallenberg K, Schulz-Schaeffer WJ, Steinhoff BJ, Grasbon-Frodl EM, Kretzschmar HA, Zerr I (2007) Creutzfeldt–Jakob disease in Germany: a prospective 12-year surveillance. Brain 130:1350–1359
Kovács GG, Puopolo M, Ladogana A, Pocchiari M, Budka H, Van Duijn C, Collins S, Boyd A, Guilivi A, Coulthart M, Delasnerie-Laupretre N, Brandel JP, Zerr I, Kretzschmar H, de Pedro-Cuesta J, Calero-Lara M, Glatzel M, Aguzzi A, Bishop M, Knight R, Belay G, Will R, Mitrova E (2005) Genetic prion disease: the EUROCJD experience. Hum Genet 118:166–174
Krasemann S, Groschup MH, Harmeyer S, Hunsmann G, Bodemer W (1996) Generation of monoclonal antibodies against human prion proteins in PrP0/0 mice. Mol Med 2:725–734
Kretzschmar HA, Ironside JW, DeArmond SJ, Tateishi J (1996) Diagnostic criteria for sporadic Creutzfeldt–Jakob disease. Arch Neurol 53:913–920
Ladogana A, Puopolo M, Croes EA, Budka H, Jarius C, Collins S, Klug GM, Sutcliffe T, Giulivi A, Alperovitch A, Delasnerie-Laupretre N, Brandel J-P, Poser S, Kretzschmar H, Rietveld I, Mitrova E, de Pedro-Cuesta J, Martinez-Martin P, Glatzel M, Aguzzi A, Knight R, Ward H, Pocchiari M, van Duijn CM, Will RG, Zerr I (2005) Mortality from Creutzfeldt–Jakob disease and related disorders in Europe, Australia, and Canada. Neurology 64:1586–1591
McGuire LI, Peden AH, Orrú CD, Wilham JM, Appleford NE, Mallinson G, Andrews M, Head MW, Caughey B, Will RG, Knight RS, Green AJ (2012) Real time quaking-induced conversion analysis of cerebrospinal fluid in sporadic Creutzfeldt–Jakob disease. Ann Neurol 2:278–285
Meissner B, Kallenberg K, Sanchez-Juan P, Krasnianski A, Heinemann U, Varges D, Knauth M, Zerr I (2008) Isolated cortical signal increase on MR imaging as a frequent lesion pattern in sporadic Creutzfeldt–Jakob disease. Am J Neuroradiol 29:1519–1524
Montine TJ, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Dickson DW, Duyckaerts C, Frosch MP, Masliah E, Mirra SS, Nelson PT, Schneider JA, Thal DR, Trojanowski JQ, Vinters HV, Hyman BT (2012) National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol 123:1–11
Neary D, Snowden J, Mann D (2005) Frontotemporal dementia. Lancet Neurol 4:771–780
Orita M, Iwahana H, Kanazawa H, Hayashi K, Sekiya T (1989) Detection of polymorphisms of human DNA by gel electrophoresis as single-strand conformation polymorphisms. Proc Natl Acad Sci USA 86:2766–2770
Parchi P, Castellani R, Capellari S, Ghetti B, Young K, Chen SG, Farlow M, Dickson DW, Sima AAF, Trojanowski JQ, Petersen RB, Gambetti P (1996) Molecular basis of phenotypic variability in sporadic Creutzfeldt–Jakob disease. Ann Neurol 39:767–778
Pocchiari M, Poupolo M, Croes EA, Budka H, Gelpi E, Collins S, Lewis V, Sutcliffe T, Guilivi A, Delasnerie-Laupretre N, Brandel JP, Alperovitch A, Zerr I, Poser S, Kretzschmar H, Ladogana A, Rietvald I, Mitrova E, Martinez-Martin P, de Pedro-Cuesta J, Glatzel M, Aguzzi A, Cooper S, Mackenzie J, Van Duijn C, Will R (2004) Predictors of survival in sporadic Creutzfeldt–Jakob disease and other human transmissible spongiform encephalopathies. Brain 10:2348–2359
Rizzu P, Van Swieten JC, Joosse M, Hasegawa M, Stevens M, Tibben A, Niermeijer MF, Hillebrand M, Ravid R, Oostra BA, Goedert M, van Dujin CM, Heutink P (1999) High prevalence of mutations in the microtubule-associated protein tau in a population study of frontotemporal dementia in the Netherlands. Am J Hum Genet 64:414–421
Southern EM (1975) Detection of specific sequences among DNA fragments separated by gel electrophoresis. J Mol Biol 98:503–517
Schulz-Schaeffer WJ, Tschoke S, Kranefuss N, Drose W, Hause-Reitner D, Giese A, Groschup MH, Kretzschmar HA (2000) The paraffin-embedded tissue blot detects PrP(Sc) early in the incubation time in prion diseases. Am J Pathol 156:51–56
Webb TE, Pal S, Siddique D, Heaney DC, Linehan JM, Wadsworth JD, Joiner S, Beck J, Wroe SJ, Stevenson V, Brandner S, Mead S, Collinge J (2008) First report of Creutzfeldt–Jakob disease occurring in 2 siblings unexplained by PRNP mutation. J Neuropathol Exp Neurol 67:838–841
Wemheuer WM, Benestad SL, Wrede A, Schulze-Sturm U, Wemheuer WE, Hahmann U, Gawinecka J, Schutz E, Zerr I, Brenig B, Bratberg B, Andreoletti O, Schulz-Schaeffer WJ (2009) Similarities between forms of sheep scrapie and Creutzfeldt–Jakob disease are encoded by distinct prion types. Am J Pathol 175:2566–2573
WHO (1998) Human transmissible spongiform encephalopathies. Wkly Epidemiol Rec 47:361–365
Windl O, Giese A, Schulz-Schaeffer W, Zerr I, Skworc K, Arendt S, Oberdieck C, Bodemer M, Poser S, Kretzschmar HA (1999) Molecular genetics of human prion diseases in Germany. Hum Genet 105:244–252
Zerr I, Kallenberg K, Summers DM, Romero C, Taratuto A, Ladogana A, Schuur M, Haik S, Collins SJ, Jansen GH, Stokin GB, Pimentel J, Hewer E, Collie DA, Smith P, Varges D, Heinemann U, Meissner B, Roberts H, Brandel JP, Van Dujin CM, Pocchiari M, Begue P, Cras P, Will RG, Sanchez-Juan P (2009) Updated clinical diagnostic criteria for sporadic Creutzfeldt–Jakob disease. Brain 132:2659–2668
Zerr I, Pocchiari M, Collins S, Brandel JP, de Pedro Cuesta J, Knight RSG, Bernheimer H, Cardone F, Delasnerie-Lauprêtre N, Cuadrado Corrales N, Ladogana A, Fletcher A, Bodemer M, Awan T, Ruiz Bremón A, Budka H, Laplanche JL, Will RG, Poser S (2000) Analysis of EEG and CSF 14–3-3 proteins as aids to the diagnosis of Creutzfeldt–Jakob disease. Neurology 55:811–815
Zou WQ, Puoti G, Xiao X, Yuan J, Qing L, Cali I, Shimoji M, Langeveld JP, Castellani R, Notari S, Crain B, Schmidt RE, Geschwind M, DeArmond SJ, Cairns NJ, Dickson D, Honig L, Torres JM, Mastrianni J, Capellari S, Giaconne G, Belay ED, Schonberger LB, Cohen M, Perry G, Kong Q, Parchi P, Tagliavini F, Gambetti P (2010) Variably protease-sensitive prionopathy: a new sporadic disease of the prion protein. Ann Neurol 68:162–172
Acknowledgments
This study was supported by grants of the Robert Koch-Institute through funds of the Federal Ministry of Health (grant 1369-341) and DZNE, Göttingen to IZ. We thank M. Schumacher, MD (University of Freiburg) and M. Heller, MD (University of Kiel) for providing MRI images and all physicians who reported suspect cases to the National Reference Center for TSE in Göttingen, Germany for providing pertinent data and biological specimens. Special thanks to P. Gambetti, MD (Case Western Reserve University, Cleveland) for the valuable comments and suggestions as well as J. Ehrlich and M. Schneider-Dominco (University of Göttingen) for their assistance in the data management and editing of the manuscript.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standards
All human studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Varges, D., Schulz-Schaeffer, W.J., Wemheuer, W.M. et al. Spongiform encephalopathy in siblings with no evidence of protease-resistant prion protein or a mutation in the prion protein gene. J Neurol 260, 1871–1879 (2013). https://doi.org/10.1007/s00415-013-6897-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-013-6897-z