Abstract
The aim of this work is to examine the clinical findings of patients with taste disorders due to central lesions and also to study the central gustatory pathway in humans. We conducted a retrospective review of 13 patients with central taste disorders that visited Nihon University Itabashi Hospital. An additional 25 cases with central taste disorders previously reported in the literature were assessed in the study. We examined 38 patients with taste disorders due to central lesions. The sites of the central lesions and their frequencies, the laterality of taste disorders relative to the central lesions, and prognosis of taste disorders were studied. We identified the following taste-related regions in the central nervous system: the medulla, pons, midbrain, thalamus, internal capsule, putamen, corona radiata, and cerebral cortex. As for the laterality of the taste disorders, we observed more ipsilateral cases for lesions located from the medulla to the pons. We observed ipsilateral, contralateral, and bilateral cases for lesions located above the midbrain, but bilateral cases were more frequently detected. Taste disorders of 80% of the patients improved by 24 weeks. The prognoses of central taste disorders appeared to be good. We identified eight central regions supposed to be relate to taste disorders. From the laterality of the taste disorders relative to the central lesions, it was suggested that the central gustatory pathway ascends ipsilaterally from the medulla to the pons, branches at the upper pons, and then ascends bilaterally from the midbrain to the cerebral cortex.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The enjoyment of food cannot be replaced by other things and taste is one of its most important factors. A loss of taste sometimes makes it difficult to detect rotten foods, and reduces the joy of eating nutritious, tasteful foods. A loss of joy of eating among people with taste disorders leads to a loss of pleasure in social life to be obtained through eating or enjoying food together. In addition, taste disorders become a large factor for reduction in appetite to adversely affect health. In this manner, taste disorders inevitably raise wide-ranging issues.
From a clinical standpoint, the most common cause of taste disorders is impairment of the peripheral receptors, while taste disorders due to central lesions have only been reported on a few occasions [1]. In comparison to other sensory organs, such as visual and auditory, the human gustatory center is less well studied and there are many unknowns regarding the human gustatory center, including its pathway.
We examined the clinical findings of patients with taste disorders due to central lesions and investigated the gustatory center in humans. A total of 38 cases, including 13 cases of our own and 25 cases previously reported in the literature, were assessed in this study.
Subjects
The medical records of our cases included 13 patients (nine males and four females; 29–73 years old, mean 56 years) who visited the Department of Otolaryngology at Nihon University Itabashi Hospital, from 1997 to 2011, were reviewed after approval was obtained from the Research Review Board of Nihon University Itabashi Hospital. Three cases of those 13 patients were reported previously in 1999 [2]. There were nine patients with cerebral infarction (69%) and four patients with cerebral hemorrhage (31%). All patients were aware of the onset of their taste disorder (Table 1).
The other 25 cases were previously reported in the literature from 1983 to 2008 [3–17]. The three cases we have already reported [2] were not included in these patients. There were 14 males and 11 females aged 17–70 years (mean 50 years).
There were 38 cases in total consisting of 23 males (61%) and 15 females (39%). The primary diseases were 23 cases (60%) of cerebral infarction, nine cases (24%) of cerebral hemorrhage, four cases (10%) of multiple sclerosis, one case (3%) of brain tumor, and one case (3%) of head trauma. Cerebral infarction, cerebral hemorrhage, and multiple sclerosis were frequent, accounting for 94% of the cases.
Study method
The patients were primarily selected if their taste function was evaluated on the left and right sides of the tongue with taste tests, such as the filter paper disk test [18], electro-gustometry [18], or swabbing or dropping a taste solution on either side of the tongue.
The following taste tests were performed in the 38 patients: electro-gustometry in three patients (8%); filter paper disk test in three patients (8%); electro-gustometry and filter paper disk test in 13 patients (34%); and swabbing or dropping a taste solution in 13 patients (34%). For the remaining six patients (16%), a specific test method was not mentioned, but their taste function was evaluated.
In addition, patients were selected in whom the site of the responsible central lesion was identified. These lesions were solitary and unilateral as diagnosed by computed tomography (CT), magnetic resonance imaging (MRI). To summarize, the imaging performed for the evaluation of the lesional sites in the 38 patients was: CT in nine patients (24%); MRI in 17 patients (45%); and CT and MRI in 12 patients (31%).
Results
The sites of the central lesions and their frequency
The sites of the central lesions that caused a taste disorder were the medulla (three cases), pons (14 cases), midbrain (two cases), thalamus (three cases), internal capsule (one case), putamen (two cases), corona radiata (three cases), and cerebral cortex (ten cases)..
Upon closer examination of the imaging, the lesions were observed in the dorsolateral medulla, the tegmentum of the pons, dorsolateral midbrain, ventral posteromedial and the ventral posterolateral nuclei of the thalamus, the posterior limb of the internal capsule, posterior corona radiata, parietal operculum, frontal operculum, and insular cortex of the cerebral cortex.
Laterality of the taste disorders relative to the central lesions
Table 2 shows the sites of the central lesions and laterality of the taste disorders in the tongue. From the medulla to the pons, 14 of 17 patients (82%) showed taste disorders ipsilateral to the central lesion. However, for lesions above the midbrain, the ipsilateral taste disorder in 21 cases has remarkably decreased to seven cases (33%). In addition, bilateral taste disorder in 21 cases has increased remarkably with ten patients (48%).
Treatments performed for central taste disorders
The treatments performed were known for 19 patients (50%). In those cases, the treatment was performed for the central lesions, but treatments aimed at improving the taste disorder were not performed. The treatments for the primary diseases were, in particular, the administration of thrombolytic or circulation-improving agents for cerebral infarctions and steroids for multiple sclerosis. Patients with underlying diseases, such as hypertension or diabetes, were treated accordingly for these conditions.
Prognosis of the central taste disorders
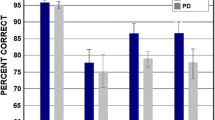
Follow-up observations of the taste disorders were conducted in 24 of the 38 patients (63%), in which an improvement was observed in 17 patients (71%) and no change was observed in seven patients (29%). The time to improvement was known in 15 patients and ranged from 1 to 48 weeks, with an average of 16 weeks. Taste disorders of seven patients (46%) improved by 8 weeks, ten patients (67%) improved by 12 weeks, and 12 patients (80%) improved by 24 weeks.
The causes of the central lesions and prognoses of the taste disorders
The frequency of improvement of the taste disorders and time to improvement were compared with regard to the primary disease. There was no significant overall relationship between the causes and time to improvement.
The prognoses of the primary diseases in the central nervous system were known in 24 of 38 patients (63%). Of these 24 patients, nine (38%) showed an improvement of the taste disorder with the improvement of the primary disease, two (8%) did not show an improvement of the primary disease or taste disorder, and three (13%) showed an improvement of the primary disease, but not of the taste disorder. The taste disorders showed a tendency to improve with the improvement of the primary diseases. The remaining ten patients (41%) showed an improvement of the taste disorder, but the prognoses of the primary diseases in the central nervous system were unknown.
Sites of the central lesions and prognoses of the taste disorders
The frequency of improvement of the taste disorders and the time to improvement were compared with regard to the location of the central lesions, however, there was no statistically significant relationship between them.
Age and prognoses of the central taste disorders
The frequency in the improvement of the taste disorders and time to improvement were compared with regard to age. However, no statistically significant relationship was detected between age and the frequency of improvement, nor between age and the time to improvement.
Discussion
Management of central taste disorders
From the results of this study, it was found that the prognoses of taste disorders due to central lesions were not related to the primary diseases, such as infarction or hemorrhage, the location of the lesion, or age. In 80% of the patients who showed an improvement of their taste disorder, this improvement was accompanied by the improvement of the primary disease. Therefore, treatment of the primary or underlying diseases is very important in the treatment of central taste disorders.
In patients who showed an improvement of their taste disorder, the taste disorder improved by 24 weeks in 80% of them. Among the patients who did not show an improvement by 24 weeks, there were three patients (20%) who showed an improvement of their taste disorder by 48 weeks. Therefore, it appears to be preferable to continue treatment for the primary diseases and conduct follow-up observations until 48 weeks, if possible.
Regions related to taste in the central nervous system
We suspect that the central lesion sites observed in this study are likely to be related to the gustatory center, i.e., the medulla, pons, midbrain, thalamus, internal capsule, putamen, corona radiata, and cerebral cortex.
As for the medulla, it is well known from animal experiments that the chorda tympani, glossopharyngeal, and vagus nerves enter the nucleus tractus solitarius in the dorsolateral medulla [19, 20]. We believe that the nucleus tractus solitarius is also an important part of the gustatory pathway in humans.
As for the pons, it has been confirmed that the central neural pathway from the medulla synapses in the rat parabrachial nucleus (PBN) [21, 22]; however, although the existence of the PBN has been inferred in humans, its details are not known.
The somatosensory nerves from the lips and tongue project into the ventral posteromedial nucleus in the thalamus, the posterior limb of the internal capsule, posterior corona radiata, and parietal operculum and insular cortex in the cerebral cortex. Therefore, there is a possibility that the central gustatory pathway travels in association with the somatosensory nerves.
Laterality of the gustatory center
The laterality of the taste disorders relative to the central lesions was ipsilateral from the medulla to the pons in many cases [2–7, 10, 11]. Therefore, the pathway was considered more likely to ascend ipsilaterally up to the PBN in the upper pons in humans, similar to what is observed in rats and monkeys.
In this study, ipsilateral [12–14, 16], contralateral [2, 7], and bilateral taste disorders [3, 14–17] were observed for lesional sites located above the midbrain. In previous reports, it was hypothesized that the pathway crosses and ascends contralaterally above the midbrain [7] or that the taste information from the right side of the tongue projects to the left insular cortex via the right insular cortex [14]. However, it is difficult to explain the existence of cases with ipsilateral, contralateral, and bilateral taste disorders with lesional sites above the midbrain on the basis of these hypotheses. Therefore, we suggest that the gustatory pathway branches at the upper pons, and then ascends bilaterally above the midbrain to the cerebral cortex.
We previously used magnetoencephalography (MEG) to measure the magnetic field in the brain induced by taste by stimulating only one side of the chorda tympani nerve in a patient whose right chorda tympani nerve was unavoidably severed during surgery for right middle ear cholesteatoma [23]. The response was almost simultaneously observed in the bilateral primary gustatory area of the cerebral cortex by stimulation of one side of the chorda tympani nerve [23]. In that study, the difference between the left and right primary response to taste was 3 ms. The conduction time in the corpus callosum of the visual, auditory, and somatosensory nerves was 14–20 ms [24–29]. Therefore, we believe that the bilateral cerebral cortex response observed by MEG in our study was not caused by crossing of the corpus callosum, but suggested that one side of the peripheral taste stimuli simultaneously projects to both sides of the cerebral cortex. This observation supports the idea that the gustatory pathway branches along the way and ascends bilaterally, as described above.
Central gustatory pathway
Studies on the gustatory centers of animals are advanced in comparison to humans, and it is now known that the central gustatory pathway differs among animal species.
The central gustatory pathway in rats ascends from the rostral part of the nucleus tractus solitarius in the medulla to the PBN ipsilaterally [21, 22]. It then branches and ascends bilaterally to the thalamic taste area [30] and projects to the insular cortex in the bilateral cerebral cortex [31].
The central gustatory pathway in the Macaque monkey ascends from the rostral part of the nucleus tractus solitarius in the medulla to the parvocellular part of the ventral posteromedial nucleus in the ipsilateral thalamus [32]. It then projects to the ipsilateral frontal operculum near the lateral sulcus of the cerebral cortex and insular cortex [33, 34]. The central gustatory pathway of the squirrel monkey is similar to that of the Macaque monkey, but the cortical gustatory area is located slightly more rostral than in the Macaque monkey [35, 36].
As for the central gustatory pathway in humans, it is known that the chorda tympani and glossopharyngeal nerves enter the ipsilateral nucleus tractus solitarius in the medulla and ascend to the pons [37], but the pathway above the midbrain remains unclear and is only inferred from physiological studies and cases with central lesions [23, 38–41]. In patients with taste disorders due to central lesions, there are many cases with ipsilateral taste disorders in which the lesional sites are located from the medulla to the pons, as described in the "Results" section for laterality [2–7, 10, 11]. Therefore, it appears likely that it ascends ipsilaterally, similar to the central gustatory pathway in rats and monkeys.
For lesions located above the midbrain, we observed ipsilateral, contralateral, and bilateral cases of taste disorders. In this regard, along with the study results of the primary gustatory area by MEG [23], the pathway is likely to branch along the way and ascend bilaterally higher than the midbrain.
If it is assumed that the central gustatory pathway branches along the way and projects to the bilateral primary gustatory areas, taste disorders would not occur in cases with unilateral central lesions and the incidence of central gustatory disorders would be very low. In fact, the incidence of central taste disorders is very low with clinically defined taste disorders observed in 1.7% of patients [1]. As mentioned above, the central gustatory pathway is likely to branch and bilaterally ascend higher than the midbrain; however, cases with taste disorders caused by a unilateral lesion above the midbrain have been reported [2, 7, 12–14, 16]. It has been reported that two-thirds of nerve fibers ascending from the PBN ascend ipsilaterally and the remaining one-third ascend contralaterally in rats [42]. If it is assumed that there is also a predominance in the central gustatory pathway in humans as in rats, then taste disorders could be caused by unilateral lesions.
Next, if the central gustatory pathway branches and ascends bilaterally, the question is: at what level does the branching occur? Since the central gustatory pathway is considered to ascend ipsilaterally from the nucleus tractus solitarius of the medulla to the PBN in the upper pons [4, 5], it is believed that the central gustatory pathway basically branches at the PBN or above the PBN. Considering the results of this study, we propose the central gustatory pathway shown in Fig. 1.
However, we identified one case with a contralateral taste disorder caused by a medullary lesion. We also identified one case with a bilateral taste disorder and one case with a contralateral taste disorder caused by a pontine lesion. In rats, other than the central gustatory pathway that ascends ipsilaterally from the rostral part of the nucleus tractus solitarius of the medulla to the PBN [21, 22], then branches and ascends bilaterally to the thalamic gustatory area [30], and projects to the bilateral insular cortex of the cerebral cortex [31], the presence of a pathway connecting the bilateral PBNs in the upper pons [43] and a bilateral pathway from the nucleus tractus solitarius to the PBN [44] have been reported. However, it cannot be determined whether these pathways exist in humans. If it is assumed that these pathways are present, contralateral and bilateral taste disorders can be caused by lesions in the medulla or pons.
There are still many unknowns about the central gustatory pathway in humans, therefore, further investigations are needed. If physiological studies, such as a study on the reaction to taste stimulation in the deep part of the brain, especially from the brain stem to around the diencephalon, or histological studies, including autopsy, are conducted, there will be great advances in our understanding of the central gustatory pathway.
References
Hamada N, Endo S, Tomita H (2002) Characteristics of 2,278 patients visiting the Nihon University Hospital Taste Clinic over a 10-year period with special reference to age and sex distribution. Acta Otolaryngol 546:7–15
Onoda K, Ikeda M (1999) Gustatory disturbance due to cerebrovascular disorder. Laryngoscope 109:123–128
Green TL, McGregor LD, King KM (2008) Smell and taste dysfunction following minor stroke: a case report. Can J Neurosci Nurs 30:10–13
Goto N, Yamamoto T, Kaneko M, Tomita H (1983) Primary pontine hemorrhage and gustatory disturbance: clinicoanatomic study. Stroke 14:507–511
Nakajima Y, Utsumi H, Takahashi H (1983) Ipsilateral disturbance of taste due to pontine hemorrhage. J Neurol 229:133–136
Uesaka Y, Nose H, Ida M, Takagi A (1998) The pathway of gustatory fibers of the human ascends ipsilaterally in the pons. Neurology 50:827–828
Lee BC, Hwang SH, Rison R, Chang GY (1998) Central pathway of taste: clinical and MRI study. Eur Neurol 39:200–203
Sunada I, Akano Y, Yamamoto S, Tashiro T (1995) Pontine haemorrhage causing disturbance of taste. Neuroradiology 37:659
Hoshino S, Hayashi A, Tamaoka A, Shoji S (1999) Bilateral gustatory disturbance caused by a unilateral pontine lesion. Neurology 53:1160–1161
Combarros O, Sánchez-Juan P, Berciano J, De Pablos C (2000) Hemiageusia from an ipsilateral multiple sclerosis plaque at the midpontine tegmentum. J Neurol Neurosurg Psychiatry 68:796
Landis BN, Leuchter I, San Millán Ruíz D, Lacroix JS, Landis T (2006) Transient hemiageusia in cerebrovascular lateral pontine lesions. J Neurol Neurosurg Psychiatry 77:680–683
Johnson TM (1996) Ataxic hemiparesis and hemiageusia from an isolated post-traumatic midbrain lesion. Neurology 47:1348–1349
Combarros O, Miró J, Berciano J (1994) Ageusia associated with thalamic plaque in multiple sclerosis. Eur Neurol 34:344–346
Pritchard TC, Macaluso DA, Eslinger PJ (1999) Taste perception in patients with insular cortex lesions. Behav Neurosci 113:663–671
Cereda C, Ghika J, Maeder P, Bogousslavsky J (2002) Strokes restricted to the insular cortex. Neurology 59:1950–1955
Kim JS, Choi S (2002) Altered food preference after cortical infarction: Korean style. Cerebrovasc Dis 13:187–191
Mathy I, Dupuis MJ, Pigeolet Y, Jacquerye P (2003) Bilateral ageusia after left insular and opercular ischemic stroke. Rev Neurol 159:563–567
Tomita H, Ikeda M, Okuda Y (1986) Basis and practice of clinical taste examinations. Auris Nasus Larynx 13(Suppl. I):1–15
Hamilton RB, Norgren R (1984) Central projections of gustatory nerves in rat. J Copm Neurol 222:560–577
Beckstead RM, Norgren R (1979) Central distribution of the trigeminal, facial, glossopharyngeal and vagus nerves in monkey. J Comp Neurol 184:455–472
Norgren R, Leonard CM (1971) Taste pathways in rat brainstem. Science 173:1136–1139
Norgren R, Leonard CM (1973) Ascending central gustatory pathways. J Comp Neurol 150:217–237
Onoda K, Kobayakawa T, Ikeda M, Saito S, Kida A (2005) Laterality of human primary gustatory cortex studied by MEG. Chem Senses 30:657–666
Andreassi JL, Okamura H, Stern M (1975) Hemispheric asymmetries in the visual cortical evoked potential as a function of stimulus location. Psychophysiology 12:541–546
Ledlow A, Swanson JM, Kinsbourne M (1978) Differences in reaction times and average evoked potentials as a function of direct and indirect neural pathways. Ann Neurol 3:525–530
Rugg MD, Lines CR, Milner AD (1984) Visual evoked potentials to lateralized visual stimuli and the measurement of interhemispheric transmission time. Neuropsychologia 22:215–225
Terasaki O, Okazaki M (2002) Transcallosal conduction time measured by visual hemifield stimulation with face images. Neuroreport 13:97–99
Mononen LJ, Seitz MR (1977) An AER analysis of contralateral advantage in the transmission of auditory information. Neuropsychologia 15:165–173
Gott PS, Hughes EC, Binggeli RL (1985) Interhemispheric transmission: assessment with vibratory somatosensory evoked potentials. Int J Neurosci 27:121–130
Ganchrow D, Erickson RP (1972) Thalamocortical relations in gustation. Brain Res 36:298–305
Yamamoto T, Kawamura Y (1977) Physiological characteristics of cortical taste area. In: Le Magnen J, MacLeod P (eds) Olfaction and taste VI. Information Retrieval, London, pp 257–264
Beckstead RM, Morse JR, Norgren R (1980) The nucleus of the solitary tract in the monkey: projections to the thalamus and brain stem nuclei. J Comp Neurol 190:259–282
Pritchard TC, Hamilton RB, Morse J, Norgren R (1986) Projections from thalamic gustatory and lingual areas in the monkey, Macaca fascicularis. J Comp Neurol 244:213–228
Ogawa H, Ito S, Nomura T (1985) Two distinct projection areas from tongue nerves in the frontal operculum of macaque monkey as revealed with evoked potential mapping. Neurosci Res 2:447–459
Benjamin RM, Burton H (1968) Projection of taste nerve afferents to anterior opercular-insular cortex in squirrel monkey (Saimiri sciureus). Brain Res 7:221–231
Benjamin RM, Emmers R, Blomquist AJ (1968) Projection of tongue nerve afferents to somatic sensory area I in squirrel monkey (Saimiri sciureus). Brain Res 7:208–220
Nageotte J (1906) The pars intermedia or nervus intermedius of Wrisberg, and the bulbopontine gustatory nucleus in man. Rev Neurol Psychiar 4:473–488
Börnstein WS (1940) Cortical representation of taste in man and monkey. I. Functional and anatomical relations of taste, olfaction and somatic sensibility. Yale J Biol Med 12:719–736
Motta G (1959) The cortical taste centers. Bull Sci Med (Bologna) 131:480–493
Kobayakawa T, Endo H, Ayabe-Kanamura S, Kumagai T, Yamaguchi Y, Kikuchi Y, Takeda T, Saito S, Ogawa H (1996) The primary gustatory area in human cerebral cortex studied by magnetoencephalography. Neurosci Lett 212:155–158
Murayama N, Nakasato N, Hatanaka K, Fujita S, Igasaki T, Kanno A, Yoshimoto T (1996) Gustatory evoked magnetic fields in humans. Neurosci Lett 210:121–123
Ogawa H, Akagi T (1978) Afferent connections to the posteromedial ventral nucleus from the pons and the rostral medulla in the rat. Kumamoto Med J 31:54–62
Spector AC (1995) Gustatory function in the parabrachial nuclei: implications from lesion studies in rats. Rev Neurosci 6:143–175
Williams JB, Murphy DM, Reynolds KE, Welch SJ, King MS (1996) Demonstration of a bilateral projection from the rostral nucleus of the solitary tract to the medial parabrachial nucleus in rat. Brain Res 737:231–237
Acknowledgments
No grant support.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Onoda, K., Ikeda, M., Sekine, H. et al. Clinical study of central taste disorders and discussion of the central gustatory pathway. J Neurol 259, 261–266 (2012). https://doi.org/10.1007/s00415-011-6165-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6165-z