Abstract
Phobic postural vertigo is characterized by subjective imbalance and dizziness while standing or walking, despite normal values for clinical balance tests. Patients with phobic postural vertigo exhibit an increased high-frequency sway in posturographic tests. Their postural sway, however, becomes similar to the sway of healthy subjects during difficult balance tasks. Posturographic recordings of 30 s of quiet stance was compared to recordings of 30 s of quiet stance during a postural threat, which consisted of the knowledge of forthcoming vibratory calf muscle stimulation, in 37 consecutive patients with phobic postural vertigo and 24 healthy subjects. During quiet stance without the threat of forthcoming vibratory stimulation, patients with phobic postural vertigo exhibited a postural sway containing significantly more high-frequency sway than the healthy subjects. During the quiet stance with forthcoming vibratory stimulation, i.e., anticipation of a postural threat, the significant differences between groups disappeared for all variables except sagittal high-frequency sway. During postural threat, healthy subjects seemed to adopt a postural strategy that was similar to that exhibited by phobic postural vertigo patients. The lack of additional effects facing a postural threat among phobic postural vertigo patients may be due to an already maximized postural adaptation. Deviant postural reactions among patients with phobic postural vertigo may be considered as an avoidant postural response due to a constant fear of losing postural control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phobic postural vertigo (PPV) is a condition characterized by dizziness while standing or walking, despite normal values for clinical balance tests [3]. The postural behavior of patients with PPV has been investigated in several studies. When standing, these patients seem to invest more muscular energy in their posture, which leads to an increased high-frequency sway >0.1 Hz [7, 12]. Healthy subjects confronted with a postural threat, such as standing on a high platform, exhibit similar postural reactions [4]. However, when healthy subjects and PPV patients are presented with a difficult balance task, such as tandem stance on foam rubber with closed eyes, the differences between the populations disappear [15]. These results indicate that already during quiescent standing, PPV patients use a postural strategy that is normally used by healthy subjects during demanding balance tasks.
We have previously compared patients with PPV with healthy subjects in terms of the effect on posture of vibratory stimulation to the calf muscles [7]. The results suggest that PPV patients are more sensitive to proprioceptive disturbances and increase their sway more than healthy subjects under such conditions.
Brandt [3] hypothesized that PPV patients exhibit a decoupling of the efference copy signal, leading to a sensory mismatch between anticipated and actual motion. This decoupling may be caused by a constant anxious control of balance performance. Kapfhammer et al. [10] have also shown that obsessive–compulsive personality traits are overrepresented in the PPV population, indicating an overrepresentation of subjects with control behaviors.
Anxiety and avoidance behaviors are among the criteria for PPV. The link between specific fears and behavioral responses to those fears are at core of the understanding and psychological treatment of anxiety disorders [2]. Our clinical experiences during behavioral treatment of patients with PPV indicate that PPV patients misinterpret their spontaneous body sway as a sign of disequilibrium and, consequently, fear losing postural control [8]. It would appear that it may be possible to understand previously documented postural reactions within the context of such cognitive processes and to link these to postural behaviors.
Earlier studies have explored postural behaviors among PPV patients during quiet stance and under different sensory conditions [7, 12]. Our aim was to explore the effect of cognitive processes on postural performance by inducing a postural threat. We hypothesized that healthy subjects exposed to a postural threat would exhibit a postural sway similar to that seen in patients with PPV during quiet stance and that PPV patients would further increase their high-frequency sway during the time period they were anticipating a threat to their postural control.
Method
The study groups comprised 37 consecutive patients with PPV (17 men and 20 women, mean age 49 years, age range 31–64 years) and 24 healthy subjects (12 men and 12 women, mean age 38 years, age range 24–49 years). Posturographic data from the PPV patients were gathered from a clinical database in which data from all patients examined at our balance clinic are stored. Data from some of the patients as well as data from the group of healthy subjects have been used in previous studies [7]. The diagnosis of PPV was based on the criteria described by Brandt [3] (Table 1), as evaluated during a clinical neurological and otoneurological examination. The findings in caloric tests and tests of subjective visual horizontal and vertical vestibular-evoked myogenic potentials, voluntary eye movements, posturography and pure-tone audiometry were non-diagnostic for any specific otoneurological disorder. All patients had normal results for neuro-radiological examinations of the brain by either computerized tomography scan or magnetic resonance imaging.
The healthy subjects were screened for vestibular deficits by clinical assessment, including presence of normal vestibulo-ocular reflex in the head impulse test and the absence of spontaneous and headshaking nystagmus in videonystagmoscopy.
The posturographic test procedure followed our clinical routine protocol. This protocol consist of:
-
1)
120 s of quiet stance with eyes open;
-
2)
120 s of quiet stance with eyes closed;
-
3)
205 s of vibratory stimulation to the calf muscles with eyes open preceded by 30 s of quiet stance; and
-
4)
205 s of vibratory stimulation to the calf muscles with eyes closed preceded by 30 s of quiet stance.
In this study we used data from the first 30 s of registration 1 and compared these to the 30 s when test subjects were standing with silent vibrators in registration 3, anticipating the onset of vibration. All test subjects were naive to the test procedure and to the vibratory stimulation. Accordingly, the difference between the two test conditions was only induced by the verbal instruction of forthcoming stimulation described in detail below. Recordings of the manipulation of sensory input, such as closing of eyes or vibratory stimulation, have not been included in this study as the focus of our research were the cognitive processes.
During the quiet stance, test subjects stand on a force platform with feet at an open angle of 30° and arms crossed over the chest. During the vibratory stimulation condition, patients stand quietly, with cylindrical vibrators (0.06 m in length and 0.01 m in diameter) mounted onto the gastrocnemius muscles of each leg by elastic straps. Patients stand quietly for 30 s before the actual vibratory stimulation begins.
Patients and healthy subjects alike were first given an introduction to the overall test situation, including the fact that test recordings would be performed during the different experimental conditions. The test subjects were then asked to stand erect, but not at attention, on the force platform. After the two quiet stance conditions, the test subjects were asked to rest in a chair as which time they were informed about the next measurement, which would include vibratory stimulation, by means of the following instruction: “Now I want you to stand on the platform again, but this time those cylinders will give you a vibrating sensation on your calf muscles, and you will experience a push”. The subjects then stood on the force platform, and vibrators were mounted to their legs. The subjects were told that the vibration would start after a short while and that the test manager was standing behind them for safety reasons.
Body sway was recorded as forces and torques from the feet acting in the lateral and sagittal plane on a force platform equipped with strain gauges. Postural performance was measured as torque variance, which reflects the mechanical energy acting on the force platform. As this measurement is influenced by the subject’s height and weight, data were normalized by the squared weight and squared height of the subject. Data were multiplied by 1000 for representational purposes. Three components of the recorded body movement were quantified for the lateral and sagittal plane separately: total torque variance, torque variance <0.1 Hz and torque variance >0.1 Hz. Investigations were performed in accordance with the Helsinki Declaration, and the study protocol was approved by the Ethics Committee of Lund University Hospital (LU 131-02).
Non-parametric tests were used since the data were not normally distributed. The Wilcoxon test for paired comparisons was used to analyze within-group differences between the two test conditions, and the Mann–Whitney test for independent samples was used to compare the results between populations. A P value of <0.05 was considered statistically significant.
Results
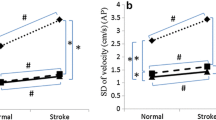
The inter-group comparison for quiet stance confirmed earlier results, with PPV patients demonstrating significantly higher torque variance, especially high-frequency sway >0.1 Hz (Table 2) [7, 12]. During the 30 s of postural threat prior to the vibratory stimulation, the significant differences between the groups disappeared for all parameters except for high-frequency anterior–posterior sway, for which the level of significance decreased (Table 2). Within-group comparisons revealed that among the healthy subjects, anticipation significantly increased torque variance in the total lateral sway (Z = −1.814, P = 0.031) and high-frequency lateral sway (Z = −2.403, P = 0.016). No significant effects of anticipation were observed within the PPV population, although there was a tendency toward decreased torque variance.
Discussion
We found that posturographic differences between healthy subjects and patients with PPV decreased during anticipation of a postural threat. Our results extend the findings of Querner et al. [15] who showed that PPV patients, compared to healthy subjects, have increased sway activity during quiet stance, but their postural behavior becomes similar to that of healthy subjects when exposed to a more challenging postural task. Thus, the postural strategy adopted by healthy subjects when confronted by both actual and verbally mediated postural threats seems to be used by PPV patients in a wider range of circumstances.
Recording of the anticipation of threat was always performed after recording of quiet stance, which may have affected the outcome systematically. However, as the order was the same for the two study groups it does not seem plausible that it would result in the differences between groups being systematically smaller. Furthermore, the test conditions conducted first, i.e., quiet stance, measures an activity that is performed several times each day, and it seems unlikely that these conditions would affect the results of latter test condition. A randomized test order might even increase the risk for bias, as repeated vibratory calf muscle stimulations induce processes of postural adaptation [5, 6]. In this study, we did not want to explore the effect of sensory stimulation. However, sensory stimulation (vibration) or deprivation (eyes closed condition) does belong in our clinical routine protocol. This routine protocol is fully described here in order to allow a full evaluation of the experimental set up although the actual stimulations performed are irrelevant in terms of the purpose of our investigation. The PPV population was older than the healthy population, and it has been well documented that balance performance deteriorates with age. However, it seems unlikely that this difference would systematically influence the effect of the anticipation of the threat. Rather, older persons seem in general to be less confident of their balance performance which would instead affect the results in the opposite direction.
Contrary to our hypothesis, during the anticipation of a postural threat, the PPV patients did not increase their high-frequency sway relative to their sway under normal conditions. One possible explanation is that these patients already have adjusted postural control to threats to a maximum, and so it is not physically possible to make any further adjustments. When there is a real postural threat, they may actually be distracted from this strategy. Confronted with a postural threat, healthy subjects co-contract their calf muscles [4]. It may be that PPV patients also adopt a postural strategy based on co-contractions of calf muscles, which would make differences between populations smaller.
Postural reflexes are susceptible to classical conditioning [11], and posturographic recordings are affected by attentional as well as cognitive factors [1, 14] and by verbal instructions [16, 17]. Operant conditioning, stepwise learning by experiential consequences and anticipatory adjustments of postural control are important components of postural behavior as, for example, when we open a door and adjust our posture to the assumed weight of the door. Patients with PPV may use this capacity of human cognitive functioning to make anticipatory posture adjustments due to a fear of falling or losing control in the absence of any actual sensory stimulus that would be a prerequisite for the behavior. Thus, the increase in the high-frequency sway found in PPV patients [7, 12] may be considered to be an anxious avoidant behavior during standing. This postural strategy consumes more muscular energy, and both muscular tension and fatigue sensitizes muscle spindles [9, 13]. Such a process may explain the sensitivity to vibratory proprioceptive stimulation previously described for PPV patients [7].
Misinterpretations and avoidance behaviors of interceptions are at core of the understanding of panic disorder [2]. According to this theory, efforts to take control of feared sensations induce increased sensitivity to these sensations. Hence, PPV might similarly be understood as a misinterpretation of, and sensitivity to spontaneous body sway, fear of losing postural control and the consequent induction of avoidant postural behaviors.
References
Andersson G, Yardley L, Luxon L (1998) A dual-task study of interference between mental activity and control of balance. Am J Otol 19:632–637
Barlow DH (2001) Clinical handbook of psychology. Guilford Press, New York
Brandt T (1996) Phobic postural vertigo. Neurology 46:1515–1519
Carpenter MG, Frank JS, Silcher CP, Peysar GW (2001) The influence of postural threat on the control of upright stance. Exp Brain Res 138:210–218. doi:10.1007/s002210100681
Fransson PA, Tjernstrom F, Hafstrom A, Magnusson M, Johansson R (2002) Analysis of short- and long-term effects of adaptation in human postural control. Biol Cybern 86:355–365. doi:10.1007/s00422-001-0305-y
Fransson PA, Hafstrom A, Karlberg M, Magnusson M, Tjader A, Johansson R (2003) Postural control adaptation during galvanic vestibular and vibratory proprioceptive stimulation. IEEE Trans Biomed Eng 50:1310–1319. doi:10.1109/TBME.2003.819851
Holmberg J, Karlberg M, Fransson PA, Magnusson M (2003) Phobic postural vertigo: body sway during vibratory proprioceptive stimulation. Neuroreport 14:1007–1011. doi:10.1097/00001756-200305230-00020
Holmberg J, Karlberg M, Harlacher U, Rivano-Fischer M, Magnusson M (2006) Treatment of phobic postural vertigo: a controlled study of cognitive-behavioral therapy and self-controlled desensitization. J Neurol 253:500–506. doi:10.1007/s00415-005-0050-6
Johansson H, Sojka P (1991) Pathophysiological mechanisms involved in genesis and spread of muscular tension in occupational muscle pain and in chronic musculoskeletal pain syndromes: a hypothesis. Med Hypotheses 35:196–203. doi:10.1016/0306-9877(91)90233-O
Kapfhammer HP, Mayer C, Hock U, Huppert D, Dieterich M, Brandt T (1997) Course of illness in phobic postural vertigo. Acta Neurol Scand 95:23–28. doi:10.1111/j.1600-0404.1997.tb00063.x
Kolb FP, Lachauer S, Maschke M, Timmann D (2002) Classical conditioning of postural reflexes. Pflugers Arch 445:224–237. doi:10.1007/s00424-002-0892-z
Krafczyk S, Schlamp V, Dieterich M, Haberhauer P, Brandt T (1999) Increased body sway at 3.5–8 Hz in patients with phobic postural vertigo. Neurosci Lett 259:149–152. doi:10.1016/S0304-3940(98)00917-3
Ledin T, Fransson PA, Magnusson M (2004) Effects of postural disturbances with fatigued triceps surae muscles or with 20% additional body weight. Gait Posture 19:184–193. doi:10.1016/S0966-6362(03)00061-4
Maki BE, McIlroy WE (1996) Influence of arousal and attention on the control of postural sway. J Vestib Res 6:53–59. doi:10.1016/0957-4271(95)00014-3
Querner V, Krafczyk S, Dieterich M, Brandt T (2000) Patients with somatoform phobic postural vertigo: the more difficult the balance task, the better the balance performance. Neurosci Lett 285:21–24. doi:10.1016/S0304-3940(00)01008-9
Riley MA, Stoffregen TA, Grocki MJ, Turvey MT (1999) Postural stabilization for the control of touching. Hum Mov Sci 18:795–817. doi:10.1016/S0167-9457(99)00041-X
Shea CH, Wulf G (1999) Enhancing motor learning through external-focus instructions and feedback. Hum Mov Sci 18:553–571. doi:10.1016/S0167-9457(99)00031-7
Acknowledgments
This study was supported by grants from The Swedish Research Council (2004-4656) and the Council for Medical Health Care in South Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holmberg, J., Tjernström, F., Karlberg, M. et al. Reduced postural differences between phobic postural vertigo patients and healthy subjects during a postural threat. J Neurol 256, 1258–1262 (2009). https://doi.org/10.1007/s00415-009-5110-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5110-x