Abstract
Necrotizing fasciitis (NF) is a life-threatening infection of soft tissues spreading along the fasciae to the surrounding musculature, subcutaneous fat and overlying skin areas that can rapidly lead to septic shock and death. Due to the pandemic increase of medical malpractice lawsuits, above all in Western countries, the forensic pathologist is frequently asked to investigate post-mortem cases of NF in order to determine the cause of death and to identify any related negligence and/or medical error. Herein, we review the medical literature dealing with cases of NF in a post-mortem setting, present a case series of seven NF fatalities and discuss the main ante-mortem and post-mortem diagnostic challenges of both clinical and forensic interests. In particular, we address the following issues: (1) origin of soft tissue infections, (2) micro-organisms involved, (3) time of progression of the infection to NF, (4) clinical and histological staging of NF and (5) pros and cons of clinical and laboratory scores, specific forensic issues related to the reconstruction of the ideal medical conduct and the evaluation of the causal value/link of any eventual medical error.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Necrotizing fasciitis (NF) is a rare but severe infection of soft tissues, usually related to bacterial invasion of the fascia, quickly spreading to muscles, subcutaneous fat and overlying skin areas, often leading to rapid death by multi-organ failure [1]. The first description of NF was reported by Hippocrates during the fifth century BC: “… many were attacked by the erysipelas all over the body when the exciting cause was a trivial accident or a very small wound” [2].
Although NF is a well-known disease since many centuries, and despite the obvious medical progress, it nowadays remains a considerable concern for practitioners in terms of diagnosis, prognosis and therapy. Indeed, NF is highly lethal (20–25% of cases), with an early diagnosis being the basis for a timely therapy and better outcome [3]. However, the non-specificity of symptoms at the time of presentation/admission together with the rapid development of septic shock and multi-organ failure (MOF) make a prompt clinical diagnosis usually very difficult [4]. Basing on the incidence, aetiology and micro-organisms involved, NF can be classified in four categories (Table 1). Various scoring systems basing on the combination of blood and clinical tests have been proposed for anticipating the diagnosis [5,6,7] among which the most used one is the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) [6].
Due to the fact that NF can lead to rapid death of also young and apparently healthy people, and that, above all in the Western countries, there has been a dramatic increase of denunciations and/or litigations (judicial and extra-judicial) for cases of presumed “malpractice or bad healthcare” [8], many cases of fatal NF have become of forensic interest. The forensic pathologist who performs the autopsy in these cases is asked to answer a number of cumbersome questions related to the time of onset of NF, the promptness of diagnosis, the correctness of therapy and the general life expectancy of the victim. Hence, knowledge and expertise of the post-mortem features of NF, including macroscopic and histological characteristics of soft tissue lesions, and of the clinical and instrumental tools utilized for the diagnosis, therapy and prognosis are of utmost importance when managing cases of alleged medical malpractice in a post-mortem scenario.
In the light of the above, the aims of our study were to review the recent scientific literature dealing with cases of NF in a post-mortem setting, to present a case series of seven NF fatalities and to discuss the main ante-mortem and post-mortem diagnostic challenges of this complex infectious disease.
Materials and methods
Review of the literature
Search 1—literature data from post-mortem investigations
A literature search in the electronic databases Pubmed, Scopus and Web of Science was conducted using a combination of free text protocols, as follows: “necrotizing fasciitis” AND (“post-mortem examination” OR “autopsy” OR “forensic pathology” OR “death” OR “fatal”). At the same time, filters such as full-text, “Article title, Abstract, Keywords” (Scopus database only), “Topic” (Web of Science database only), publication date from January 2000 to November 2017, humans and English language were activated resulting in more than 400 articles, which were submitted to the following criteria of inclusion:
-
Presentation of post-mortem cases investigated through (at least) an autopsy with or without histology and/or microbiology analyses.
-
Critical discussion on ante- and/or post-mortem issues related to the diagnosis and/or prognosis and/or therapy of NF.
The selected papers were analysed in full-text and the following data were extracted and included in an electronic database: first author’s name, Journal, year of publication, type of paper, number of cases presented, histopathology and microbiology findings, time delay between hospital admission and death.
Search 2—literature data on the LRINEC score
A second literature search was conducted in the electronic databases Pubmed, Scopus and Web of Science using the following free-text protocols: “necrotizing fasciitis” AND (score OR scale) AND (sensitivity OR specificity OR “diagnostic accuracy”). Similarly, to search 1, filters such as “Article title, Abstract, Keywords” (Scopus database only), “Topic” (Web of Science database only), full-text, publication date from January 2000 to November 2017, humans and English language were activated resulting in more than 30 articles. Only manuscripts discussing the diagnostic efficiency of the LRINEC or modified LRINEC scores were included. The following data were extracted from each article and registered in an electronic database: first author’s name, number of investigated cases, applied score cut-off and diagnostic efficiency of the score (i.e. sensitivity, specificity, positive predictive value, negative predictive value and area under the curve).
Case series
Cases were selected among forensic casework of the Institutes of Legal Medicine of the Universities of Padova and Verona (Italy) in the time frame 2006–2016, searching the reports for a diagnosis of “necrotizing fasciitis”. For each of the included cases, forensic autopsy was performed within 48 h after death. Multiple specimens were collected from internal organs and from the necrotizing fasciae and the surrounding tissues for histopathology and microbiology investigations. Samples of skin and subcutaneous tissues were stained with haematoxylin and eosin, periodic acid–Schiff (PAS), Giemsa and Gram.
A comprehensive analysis of ante-mortem data, including clinical records and anamnestic data collected from the relatives of the deceased, was performed focusing on the diagnostic and prognostic key elements. The medical conduct of each case was analysed following the logical steps provided by the Guidelines of the International Academy of Legal Medicine (IALM) [9].
The following key points were highlighted and synthetized in a synoptic table, including the clinical picture of the patient; time intervals between first medical consult and death, appearance of local NF skin lesions and death, and septic shock and death; main therapeutic maneuvers; timing in which the LRINEC or modified LRINEC scores turned positive (retrospective calculation), and post-mortem data.
Results
Review of the literature
Search 1
Thirty-eight (38) papers dealing with NF in a post-mortem setting fulfilled the inclusion criteria and thus were included in the investigation [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. Among these, 32 (84.2%) were case reports, 3 (7.9%) case series, 2 (5.3%) original articles, and 1 (2.6%) was a review. The extracted data are summarized in Table A (Online Resource 2). In summary, a total of 183 post-mortem NF cases were investigated, with histology investigation (at least haematoxylin and eosin) described in 92.1% of the selected papers. Special stains, such as Gram stain and Van Gieson, were performed in 23.7% of the included investigations. Post-mortem microbiology was described in 81.6% of the selected papers, with group A β-haemolytic streptococcus (GAS) identified in 36.8%, followed by Clostridium species (15.8%), E. Coli (10.5%) and Vibrio vulnificus (10.5%).
Search 2
Twenty-three (23) papers [6, 48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70] fulfilled the inclusion criteria of the second literature search specifically dealing with the diagnostic efficiency of the LRINEC score for diagnosing NF (Table B - Online Resource 3). Among these 21 (91.3%) were original articles (20 retrospective studies and 1 prospective study), 1 was a review (4.3%) and 2 (8.7%) were commentaries. In all the included investigations, the LRINEC score was calculated at hospital admission with the cut-off for positivity generally set at 6 (range between 2 and 9). Sensitivity ranged between 22 and 94%, specificity between 36 and 94%, positive predictive between 20 and 93%, and negative predictive between 83 and 99%.
Case series
The circumstantial, clinical and post-mortem data (autopsy, histology and microbiology) of the seven (7) analysed cases are summarized in Table 2. Sex was fairly equally distributed (57% females; 43% male) with age ranging between 25 and 50 years. At first medical consultation, in the majority of cases (case 1, 3, 4, 6 and 7; 71.4%), the patient complained of traumatic pain, while in the remaining cases (case 2 and 5; 28.6%), only pain, without any recent trauma, was reported. A tentative diagnosis was achieved in 85% of cases, with NF never included among these, not even as an alternative hypothesis (i.e. differential diagnosis). After hospital admittance, all patients received antibiotics associated in 57.1% with non-steroidal anti-inflammatory drugs (NSAIDs) and surgical debridement in the remaining cases (42.9%). After the appearance of skin injuries or septic shock, NF was diagnosed in two cases (case 5 and 7; 28.6%). The retrospective calculation of the LRINEC score performed by the authors evidenced positivity only a few hours before sepsis (Table 2). The cause of death was always multi-organ failure (MOF) confirmed at histology. Basing on microbiology, five cases (case 1, 3, 4, 5 and 6) were classified as type II (71.4%), among which four sustained by group A β-haemolytic streptococcus (GAS) and one by Staphylococcus aureus, and two NFs were classified as type I (case 2 with E. Coli and Staphylococcus haemolyticus and case 7 with mixed bowel flora-derived bacteria). Type II cases with the presence of GAS displayed a fulminant progression to MOF and death occurred at less than 12 h from septic shock with MOF.
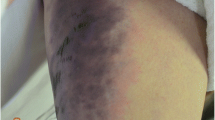
In all cases, histology showed interstitial oedema (Fig. 1—Online Resource 1), necrosis (Fig. 1B—Online Resource 1) and haemorrhagic infiltration (Fig. 1C—Online Resource 1) along the subcutaneous fasciae, with areas characterized by predominant neutrophil inflammation alternating with bacterial colonies (Fig. 1C–D—Online Resource 1), which can be better revealed through the use of special stains, such as Giemsa (Fig. 1E—Online Resource 1) or PAS. The surrounding vessels were filled with neutrophil granulocytes and bacteria, while the inflammatory reaction was minimal or absent in the epidermis, subcutaneous adipose tissue (Fig. 1F—Online Resource 1) and underlying muscles. The thoracic and abdominal organs were characterized by non-specific signs of sepsis and shock.
Discussion
Although the incidence of NF is quite limited (about 0.40 cases per 100,000 population), the pandemic increase of litigations due to medical malpractice implicated a rise in NF cases of virtual forensic interest [9]. In the vast majority of these cases, the forensic pathologist is asked to answer a number of cumbersome questions, including the reconstruction of the pathological features of the disease, the identification of any medical errors and their eventual causal value in causing the death. To this end, it is crucial to reconstruct also the prognosis quoad vitam of each case using objective data.
Origin of soft tissue infection
Micro-organisms leading to NF infection usually reach the fascia through a discontinuation of the skin (generally caused by a trauma) producing a continuum between the external environment and the subcutaneous tissue. Indeed, the origin of NF has been attributed to a heterogeneous set of traumas (even trivial in their entity), such as varicella skin lesions [20], penetrating or blunt trauma, surgery, colonic perforation [37], intestinal hernia [46], needle stick injuries [13, 14, 23], tattoos [16, 43], childbirth [47], burns, toothpick injuries, insect bites, injuries from stingrays [10] and/or rectal mucosal injuries related to temperature measurements [25].
NF may also develop following a trauma without any evidence of skin discontinuation (e.g. a bruise) or in the absence of any trauma at all, especially in subjects displaying pre-existing favouring conditions [29], such as advanced age [41], diabetes mellitus [19], rheumatoid arthritis [24, 34], chronic renal failure, peripheral vascular disease, alcoholic liver cirrhosis [29], liver disease [22], malignancy [12, 15], myelotoxic chemotherapy and/or malnutrition. In such cases, it was hypothesized that the responsible micro-organisms colonize an extra-cutaneous body district, spread through the blood to a site of dermatic inflammation (such as an hematoma or bruise) and cause the NF infection.
In the presented cases, a previous trauma was anamnestically reported in five out of seven cases (71.4%). Among these, in only one occasion (case 7, motorcycle crash), a discontinuation of the skin was medically ascertained. There are two plausible explanations for this finding: (a) the skin lesions were truly absent in four out of five cases of NF and (b) the clinicians failed to describe the skin discontinuations because they were trivial and/or clinically insignificant. Even in this latter hypothesis, the autopsy might not be conclusive because of the overlaying NF necrosis and/or because of their healing (in our case series, skin discontinuations at autopsy were evident only in case 7).
In case 2, the infection was probably related to gut microbiota spreading to the surrounding soft tissues through a myelodysplastic lesion of the intestinal wall [27].
From a medico-legal point of view, it is crucial to examine the entire body (including inner organs) without restricting the search to soft tissues, in order to identify the most probable origin of the infection. Indeed, if the primary cause of the infection is a trauma related to a human action (e.g. physical assault, car accident, etc.), the legal subject of that action could face the juridical consequences of the NF-related death (e.g. manslaughter or unintentional killing). Nonetheless, the forensic pathologist should also be aware of the fact that, regardless of the thoroughness of the search, not always might the origin of the infection be identified with strong forensic evidence.
Micro-organisms responsible of the infection
As widely reported in the literature, NF can be classified into different types basing on the results of the ante- and/or post-mortem cultures (Table 1) [4].
For a proper identification of the micro-organism(s) involved, the forensic pathologist should examine any clinical microbiology data and collect peripheral blood and necrotizing tissues during autopsy, which should be performed as soon as possible after the exitus in order to limit the invasion of tissues by saprophytic bacterial flora. The identification of the micro-organisms involved in the necrosis can be crucial for determining the prognosis of the disease, and for evaluating the correctness of the medical interventions (e.g. antibiotic therapy, surgical debridement). It is well-known, indeed, that type II NFs, especially in the presence of group A β-haemolytic streptococcus (GAS), exhibit a rapid clinical progression to septic shock and death (about 70% of cases) despite any medical/surgical treatment or intensive supportive care [21].
In our case series, 5 (five) cases were classified as type II (71.4%), among which four sustained by group A β-haemolytic streptococcus (GAS) and one by Staphylococcus aureus, and two NFs were classified as type I (one with E. Coli and Staphylococcus haemolyticus and the other with mixed bowel flora-derived bacteria). Type II cases with the presence of GAS displayed a fulminant progression to MOF and death occurred at less than 12 h from septic shock with MOF.
Diagnosis, time of onset and progression of the infection to NF
In sporadic cases, with a still unclear etiopathogenesis, soft tissue infections can evolve to NF [71]. The identification of the moment in which a generally benign soft tissue infection progresses to NF is a cumbersome task.
Clinical diagnosis and staging
Generally, NF is divided into three clinical phases:
-
a)
During the first 24 h (i.e. early phase, progression of the infection to NF), pain out of proportion is generally reported in the site of a minor trauma or local skin infection. Possible adjunctive findings are erythema and/or induration of the skin.
-
b)
During the next 2–4 days (i.e. intermediate phase), signs of clinical toxicity, such as fever, dehydration confusion, dizziness, diarrhea, nausea, vomiting, weakness and malaise, might appear. The painful area displays “hard signs” of NF, such as swelling, purplish rash or blisters with “dish-wash” purulent or hemorrhagic fluid, local emphysema and gas formation under the skin. Pain grows and is clearly disproportionate with respect to the skin lesion/s.
-
c)
After 4–6 days, septic shock and multiple organ dysfunction syndrome (i.e. late phase) appear and are accompanied by cardiac shock, tachycardia, hypotension, rise of the white blood cell count, acidosis, coagulopathy, changes of mental status and weakness [3].
Considering a typical clinical course, symptoms and hard signs of NF should develop several days before multi-organ failure, allowing to rise the suspect of NF. However, in the acute and fulminant forms, the infection spreads systemically very quickly with premature signs and symptoms of severe septic shock. As a matter of fact, in all of the seven cases herein presented, NF developed with a fulminant course with hard signs appearing only contextually to septic shock, followed by rapid death, occurring within 24 h from sepsis. Therefore, the forensic pathologist examining fatal cases of NF in an ex-post condition must be very cautious while clinically staging NF.
Even if NF is a clinical diagnosis, radiological imaging can contribute to its assessment especially regarding the extension of the disease and the occurrence of complications [72]. Ultrasound, demonstrating fascial thickening and fluid collection, is mainly useful in paediatric patients [73, 74]. Plain radiographs play a marginal role since findings like soft-tissue thickening and opacity may mimic those of cellulitis. Furthermore, gas in the soft tissue, which is considered a characteristic feature, is rarely shown [73]. Soft-tissue air and fluid in the deep fascia, even if inconstant, are well identified at computed tomography (CT) [72, 74]. CT can also reveal thickening and enhancement of the fascia, lymphadenopathy and severe complications such as vascular rupture [73]. Magnetic resonance imaging (MRI) because of its intrinsic high soft tissue contrast is especially suitable for diagnosing NF. Indeed, high signal intensity in the fluid sensitive sequences along the deep fascia, in particular the deep intermuscular fascia, is an easily detected key diagnostic finding [74, 75].
Potential utility of LRINEC for an early diagnosis and clinical staging of NF
Numerous scoring systems based on the combination of blood tests and clinical data have been proposed aiming at anticipating the clinical diagnosis of NF. Among these, the LRINEC score, recently improved to the modified LRINEC, which considers also clinical variables, is the most widely used one.
The Laboratory Risk Indicator for Necrotizing Fascitis (LRINEC) is a robust scoring system driven from six routinely performed laboratory tests, including C-Reactive Protein, total white cell count per cubic millimetre, haemoglobin, sodium, creatinine and glucose, which is used to early distinguishing NF from the other severe soft tissue infections [6]. Different cut-offs have been used to stratify the patients into different risk categories for NF, which corresponded to a probability of developing NF and to related statistical parameters such as sensitivity, specificity, positive and negative predictive values, reported in Table B (Online Resource 3).
The performance of the LRINEC for anticipating the diagnosis of NF has been widely discussed in the literature. Our review showed meaningfully different values of sensitivity and specificity of the LRINEC score for diagnosing NF, mainly depending on the characteristics of the analysed population [6, 48,49,50,51, 53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70]. The common denominator of these studies was a pre-selection of the included cases, which, at least in our opinion, caused an increase of the reported diagnostic efficiency of the score.
In our case series, the LRINEC score was only retrospectively calculated, since the clinicians never used it. In the majority of cases, the score turned positive only a few hours before septic shock (Table 2). The only exception was case 7, where the score tested positive 9 h before the appearance of skin lesions and about 2 days before septic shock. Notwithstanding, in about 70% of cases (1, 2, 4, 6 and 7), the score turned positive some hours before the appearance of any visible skin lesions. On that point, however, it must be kept in mind that the applicability of the score is strictly related to the presence of any detectable signs of soft tissue infection (i.e. local lesions) [6]. Therefore, in a forensic setting, the LRINEC score should be used with extreme caution for the evaluation of the correctness of the medical conduct and always interpreted in relation to the presence of any visible signs of local infection.
Histological diagnosis and staging
Histology must be mandatory for a definitive post-mortem diagnosis of NF, through the detection of dermal inflammation or necrosis associated to the presence of bacterial colonies. In the early stages of the disease, only dermal oedema and polymorphonuclear infiltration into the dermis are observed. During the intermediate stages, haemorrhages and angiothrombosis of the penetrating fascial vasculature are evident. Finally, in the later stages, all tissue layers can show various degrees of necrosis [3]. Differential diagnosis with more frequent soft tissue infections is usually requested. The depth of involvement, as well as the degree of connective tissue degeneration and necrosis, is much greater in NF than in other forms of cellulitis [76]. In our case series, we observed that the epidermis was moderately affected, notwithstanding the advanced stage of the disease; this could be connected to the fact that the infective and inflammatory process spreads horizontally along the subcutaneous fasciae, only later invading the surrounding adipose tissue, which is well represented in the hypodermis, thereby acting as an initial barrier to the infective process.
Along the subcutaneous fascia, the inflammation process is often modest and localized, while the bacterial colonies may not be very apparent when utilizing the H&E stain; consequently, it is necessary to search for the presence of bacteria using special stains, such as Giemsa or PAS, in order to diagnose NF and identify the cause of death.
Based on the above described microscopic features, as confirmed by our case series (see Figure 1, Online Resource 1 for details), only an approximate dating of the chronological stage of NF is possible. On the other hand, it is well-known that the precise estimation of the time of onset of the inflammatory reaction is based on the progressive appearance of inflammatory cells and capillary proliferation (granulation tissue). Unfortunately, the inflammatory reaction is poor in the early and middle stages of NF. Therefore, any attempt at dating based on histopathological data, including immuno-histochemical markers, would seem questionable.
Specific medico-legal issues of the reported cases
As stated by the recent international IALM Guidelines on the methods of ascertainment and criteria of evaluation of cases of suspected medical malpractice, the very first step of the medico-legal evaluation process foresees the identification of the clinical features and the reconstruction of the pathological pathways that connect the initial, intermediate and final stages of the investigated disease [9]. As previously discussed, the uncertainties related to the identification of the origin of the soft tissue infection, the micro-organisms involved, the timing of progression to NF, the staging of the disease, the rapidity of its evolution to systemic infection and multi-organ failure make a trustworthy reconstruction of the chain of events often problematic.
In order to determine if a specific disorder was clinically recognizable at a given time, firstly, it is fundamental to identify the exact moment in which the disease commenced. As observed in our case series, in the majority of cases (5 cases; 71.4%), neither in an ex-ante (i.e. only with circumstantial and clinical data) nor in an ex-post perspective (i.e. integrating clinical and post-mortem data) was it possible to identify the exact timing of progression of the soft tissue infection to NF. In four out of the seven reported cases (57.1%), patients referred to the emergency room complaining of post-traumatic pain (car, motorcycle or bicycle crash), whereas in the remaining three cases, pain was attributed by the physician to a gastrointestinal (case 2) or neuronal (cases 5 and 6) disorder. Was it correct? To answer this question, the medico-legal expert should be able to reconstruct the signs and symptoms truly exhibited by the patient in that specific moment and evaluate if those signs were clearly attributable to NF. As can be seen in Table 2, local lesions generally appeared at less than 24 h from septic shock and death. Integrating clinical data, laboratory and post-mortem data, in an ex-post perspective, the absence of a clinical diagnosis of NF or a slight diagnostic and/or therapeutic delay would be identifiable in five out of seven cases. A timely diagnosis followed by surgical debridement was indeed possible only for the two cases not related to GAS infection (cases 5 and 7).
As well-known, in order to entail any criminal and/or civil responsibility, a medical error must be causally related to the death or personal injury/damage suffered by the patient [9, 77]. In cases of NF, in order to evaluate the causal value and link between a supposed diagnostic/therapeutic error and the loss (e.g. death, personal injury, etc.), it is essential to define the prognosis of the disease. In general, NF mortality rate is around 20–25%. In forensic medicine, however, the probability of death (and more extensively the prognosis) must be reconstructed for each specific case under investigation.
As a general trend, when unequivocal cutaneous signs of NF become evident, mortality estimates are very high due to the presence of concurrent signs of septic shock, which may be considered the “point of no return” for NF infections. Regarding our case series, although in five cases the diagnosis and surgical therapy could have been anticipated of a few yours, those diagnostic and therapeutic delays were not causally related to the subsequent death.
Conclusion
In a clinical setting, the presence of visible skin lesions are essential to consider additional diagnostic tests, such as clinical scores (e.g. LRINEC), radiology and microbiology, and to perform a rapid medical and/or surgical therapy. Data from our case series suggest that pain out of proportion is often not enough to pose a timely suspect of NF. Indeed, pain, although intense, is a non-specific symptom usually attributable to alternative tentative diagnoses, such as trauma, gastrointestinal or neurological disorders.
Forensic autopsy and histology, including special stains (such as Giemsa or PAS), are mandatory to reach a definitive post-mortem diagnosis of NF. However, due to the fact that the inflammatory reaction is poor in the early and middle stages of the disease, even after histology and microbiology, the origin of the infection and the staging of the disease might remain unknown or not forensically proven. Therefore, the medico-legal expert must reconstruct the pathological features of the disease and the ideal medical conduct without any precise data on the timing of appearance of unequivocal signs of NF, except for the reports of the assisting physicians. In our case series, signs and symptoms clearly attributable to NF were medically reported almost in coincidence with signs and symptoms of septic shock followed by death within 24 h. If a diagnostic/therapeutic error or delay is identified, the forensic expert must evaluate the causal value link of that error with the patient’s loss (i.e. personal injury or death) and thus be capable of reconstructing the prognosis of NF in the specific case under investigation. Different, independent predictors of mortality should be used keeping in mind, however, that different scores can give slightly divergent results and that “ex-post” retrospective calculations must be interpreted with extreme caution. The reconstruction of the ideal medical conduct, indeed, must always be performed in an “ex ante” viewpoint, that is identifying oneself with the physician who assisted the patient in that specific clinical setting and time condition. The difficult assignment of the forensic pathologist dealing with cases of suspected medical malpractice is even harder in cases of NF because the expert will have to display great humility and often admit the impossibility to answer the questions of the prosecutor because of uncertainties and/or lack of evidence.
References
Wilson B (1952) Necrotizing fasciitis. Am Surg 18:416–431
Descamps V, Aitken J, Lee MG (1994) Hippocrates on necrotising fasciitis. Lancet 344:556
Roje Z, Matic D, Librenjak D, Dokuzovic S, Varvodic J (2011) Necrotizing fasciitis: literature review of contemporary strategies for diagnosing and management with three case reports: torso, abdominal wall, upper and lower limbs. World J Emerg Surg 6:46
Morgan MS (2010) Diagnosis and management of necrotising fasciitis: a multiparametric approach. J Hosp Infect 75:249–257
Murphy G, Markeson D, Choa R, Armstrong A (2013) Raised serum lactate: a marker of necrotizing fasciitis? J Plast Reconstr Aesthet Surg 66:1712–1716
Wong CH, Khin LW, Heng KS, Tan KC, Low CO (2004) The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 32:1535–1541
Wall DB, Klein SR, Black S, de Virgilio C (2000) A simple model to help distinguish necrotizing fasciitis from nonnecrotizing soft tissue infection. J Am Coll Surg 191:227–231
Ferrara SD (2013) Medical malpractice and legal medicine. Int J Legal Med 127(3):541–543
Ferrara SD, Baccino E, Bajanowski T et al (2013) Malpractice and medical liability. European Guidelines on Methods of Ascertainment and Criteria of Evaluation. Int J Legal Med 127:545–557
Rutty GN, Busuttil A (2000) Necrotizing fasciitis: reports of three fatal cases simulating and resulting from assaults. Am J Forensic Med Pathol 21:151–154
Callister ME, Wall RA (2001) Descending necrotizing mediastinitis caused by group a streptococcus (serotype M1T1). Scand J Infect Dis 33:771–772
Francque SM, Van Laer C, Struyf N, Vermeulen P, Corthouts B, Jorens PG (2001) Perforating oesophageal carcinoma presenting as necrotizing fasciitis of the neck. Eur J Gastroenterol Hepatol 13:1261–1264
McGuigan CC, Penrice GM, Gruer L et al (2002) Lethal outbreak of infection with Clostridium novyi type A and other spore-forming organisms in Scottish injecting drug users. J Med Microbiol 51:971–977
Finn SP, Leen E, English L, O'Briain DS (2003) Autopsy findings in an outbreak of severe systemic illness in heroin users following injection site inflammation: an effect of Clostridium novyi exotoxin? Arch Pathol Lab Med 127:1465–1470
Abella BS, Kuchinic P, Hiraoka T, Howes DS (2003) Atraumatic Clostridial myonecrosis: case report and literature review. J Emerg Med 24:401–405
Porter CJ, Simcock JW, MacKinnon CA (2005) Necrotising fasciitis and cellulitis after traditional Samoan tattooing: case reports. J Inf Secur 50:149–152
Muldrew KL, Simpson JF, Stratton CW, Tang YW (2005) Molecular diagnosis of necrotizing fasciitis by 16S rRNA gene sequencing and superantigen gene detection. J Mol Diagn 7(5):641–645
Yang Z, Lavelle JC, Reilly SD (2006) A 51-year-old man with acute dyspnea and leg swelling. Lab Med 37:611–612
Matsubara K, Mikamo H, Numa M, Yamamoto G, Kusano H, Takamine Y (2006) Three fatal cases of invasive serotype VI group B streptococcal infection. J Inf Secur 53:e139–e142
Hidalgo-Carballal A, Suarez-Mier MP (2006) Sudden unexpected death in a child with varicella caused by necrotizing fasciitis and streptococcal toxic shock syndrome. Am J Forensic Med Pathol 27:93–96
Batalis NI, Caplan MJ, Schandl CA (2007) Acute deaths in nonpregnant adults due to invasive streptococcal infections. Am J Forensic Med Pathol 28:63–68
Muldrew KL, Miller RR, Kressin M, Tang YW, Stratton C (2007) Necrotizing fasciitis from Vibrio vulnificus in a patient with undiagnosed hepatitis and cirrhosis. J Clin Microbiol 45:1058–1062
Dunbar NM, Harruff RC (2007) Necrotizing fasciitis: manifestations, microbiology and connection with black tar heroin. J Forensic Sci 52:920–923
Sugimoto T, Nakazawa J, Yomoda M et al (2007) Necrotizing fasciitis resulting from Escherichia coli in a patient with chronic rheumatoid arthritis. APLAR J Rheumatol 10:57–59
Christensen RD, Pysher TJ, Christensen SS (2007) Case report: perianal necrotizing fasciitis in a near-term neonate. J Perinatol 27:390–391
Bono G, Argo A, Zerbo S, Triolo V, Procaccianti P (2008) Cervical necrotizing fasciitis and descending necrotizing mediastinitis in a patient affected by neglected peritonsillar abscess: a case of medical negligence. J Forensic Legal Med 15:391–394
Tajiri T, Tate G, Akita H, Ohike N, Masunaga A, Kunimura T, Mitsuya T, Morohoshi T (2008) Autopsy cases of fulminant-type bacterial infection with necrotizing fasciitis: group A (beta) hemolytic Streptococcus pyogenes versus Vibrio vulnificus infection. Pathol Int 58:196–202
Akamine M, Miyagi K, Uchihara T, Azuma M, Yara S, Higa F, Haranaga S, Tateyama M, Matsuzaki A, Nakayama T, Fujita J (2008) Necrotizing fasciitis caused by Pseudomonas aeruginosa. Intern Med 47(6):553–556
Tajiri T, Tate G, Miura K, Masuda S, Ohike N, Kunimura T, Mitsuya T, Morohoshi T (2008) Sudden death caused by fulminant bacterial infection: background and pathogenesis of Japanese adult cases. Intern Med 47:1499–1504
Loughnan BA, Grover M, Nielsen PB (2010) Maternal death due to extended spectrum beta-lactamase-producing E. coli: a warning for the future? Int J Obstet Anesth 19:327–330
Sugiyama T, Kobayashi T, Nagao K, Hatada T, Wada H, Sagawa N (2010) Group A streptococcal toxic shock syndrome with extremely aggressive course in the third trimester. J Obstet Gynaecol Res 36:852–855
Radovan K, Ilic G, Antovic A, Banovic LK, Miroslav M, Marina D (2011) Rapidly fatal necrotizing fasciitis: report of three cases. Rom J Legal Med 19:95–100
Heinze S, Puschel K, Tsokos M (2011) Necrotizing fasciitis with fatal outcome: a report of two cases. Forensic Sci Med Pathol 7:278–282
Iwata K, Arinuma Y, Nakayama H, Nogi S, Futami H, Takaoka H, Hashimoto A, Shimada K, Komiya A, Matsui T, Saito I, Tohma S (2011) An autopsy case of necrotizing fasciitis with rapidly progressive purpura caused by hemolytic streptococcal infection in a patient with rheumatoid arthritis. Mod Rheumatol 21:669–672
Reinders JSK, Schuurman JP, de Vries JPPM, Biemond-Moeniralam HS, Vlaminckx BJM, Wille J (2011) Severe necrotizing soft tissue disease. Netherlands. J Crit Care 15:212–217
van der Oord BM, Hol C, Manten B (2011) An exceptional case of streptococcal toxic shock syndrome. Netherlands. J Crit Care 15:27–29
Reisman JS, Weinberg A, Ponte C, Kradin R (2012) Monomicrobial Pseudomonas necrotizing fasciitis: a case of infection by two strains and a review of 37 cases in the literature. Scand J Infect Dis 44:216–221
Kiratisin P, Leelaporn A, Sangruchi T (2012) Vibrio vulnificus septicemia in Thailand: a 12-year case series and report of two fatal massive rhabdomyolysis cases. Asian. Biomedicine 6:495–502
Tajiri T, Tate G, Masunaga A, Mitsuya T, Miura K, Masuda S, Kunimura T, Morohoshi T (2012) Autopsy cases of fulminant bacterial infection in adults: clinical onset depends on the virulence of bacteria and patient immune status. J Infect Chemother 18:637–645
Suzuki H, Hikiji W, Shigeta A, Fukunaga T (2013) An autopsy case of a homeless person with unilateral lower extremity edema. Leg Med (Tokyo) 15:209–212
Cope TE, Cope W, Beaumont DM (2013) A case of necrotising fasciitis caused by Serratia marsescens: extreme age as functional immunosuppression? Age Ageing 42:266–268
Fernando DM, Kaluarachchi CI, Ratnatunga CN (2013) Necrotizing fasciitis and death following an insect bite. Am J Forensic Med Pathol 34:234–236
Hourmozdi JJ, Hawley DA, Hadi CM, Tahir B, Seupaul RA (2014) Streptococcal necrotizing myositis: a case report and clinical review. J Emerg Med 46:436–442
Wu YE, Baras A, Cornish T, Riedel S, Burton EC (2014) Fatal spontaneous Clostridium septicum gas gangrene: a possible association with iatrogenic gastric acid suppression. Arch Pathol Lab Med 138:837–841
Vongpaisarnsin K, Tansrisawad N, Hoonwijit U, Jongsakul T (2015) Pseudomonas aeruginosa septicemia causes death following liposuction with allogenic fat transfer and gluteal augmentation. Int J Legal Med 129:815–818
Yonekura S, Kodama M, Murano S, Kishi H, Toyoda A (2016) Richter's type of incarcerated obturator hernia that presented with a deep femoral abscess: an autopsy case report. Am J Case Rep 17:830–833
Rellinger EJ, Craig BT, Craig-Owens LD, Pacheco MC, Chung DH, Danko ME (2016) Clostridium sordellii necrotizing omphalitis: a case report and literature review. J Pediatr Surg Case Rep 10:35–38
Wang TL, Hung CR (2004) Role of tissue oxygen saturation monitoring in diagnosing necrotizing fasciitis of the lower limbs. Ann Emerg Med 44:222–228
Wong CH, Wang YS (2005) The diagnosis of necrotizing fasciitis. Curr Opin Infect Dis 18:101–106
Wong CH (2005) Tissue oxygen saturation monitoring in diagnosing necrotizing fasciitis of the lower limb: a valuable tool but only for a select few. Ann Emerg Med 45:461–462 author reply 2-3
Wong CH, Khin LW (2005) Clinical relevance of the LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score for assessment of early necrotizing fasciitis. Crit Care Med 33:1677
Wang TL (2005) In reply. Ann Emerg Med 45:462–463
Su YC, Chen HW, Hong YC, Chen CT, Hsiao CT, Chen IC (2008) Laboratory risk indicator for necrotizing fasciitis score and the outcomes. ANZ J Surg 78:968–972
Thomas AJ, Meyer TK (2012) Retrospective evaluation of laboratory-based diagnostic tools for cervical necrotizing fasciitis. Laryngoscope 122:2683–2687
Liao CI, Lee Y-K, Su Y-C, Chuang C-H, Wong C-H (2012) Validation of the laboratory risk indicator for necrotizing fasciitis (LRINEC) score for early diagnosis of necrotizing fasciitis. Tzu Chi Med J 24:73–76
Chao WN, Tsai SJ, Tsai CF, Su CH, Chan KS, Lee YT, Ueng KC, Lin DB, Chen CC, Chen SC (2012) The Laboratory Risk Indicator for Necrotizing Fasciitis score for discernment of necrotizing fasciitis originated from Vibrio vulnificus infections. J Trauma Acute Care Surg 73:1576–1582
Swain RA, Hatcher JC, Azadian BS, Soni N, De Souza B (2013) A five-year review of necrotising fasciitis in a tertiary referral unit. Ann R Coll Surg Engl 95:57–60
Bozkurt O, Sen V, Demir O, Esen A (2015) Evaluation of the utility of different scoring systems (FGSI, LRINEC and NLR) in the management of Fournier's gangrene. Int Urol Nephrol 47:243–248
Hodgins N, Damkat-Thomas L, Shamsian N, Yew P, Lewis H, Khan K (2015) Analysis of the increasing prevalence of necrotising fasciitis referrals to a regional plastic surgery unit: a retrospective case series. J Plast Reconstr Aesthet Surg 68:304–311
Sandner A, Moritz S, Unverzagt S, Plontke SK, Metz D (2015) Cervical necrotizing fasciitis—the value of the laboratory risk indicator for necrotizing fasciitis score as an indicative parameter. J Oral Maxillofac Surg 73:2319–2333
Borschitz T, Schlicht S, Siegel E, Hanke E, von Stebut E (2015) Improvement of a clinical score for necrotizing fasciitis: ‘pain out of proportion’ and high CRP levels aid the diagnosis. PLoS One 10:e0132775
Kincius M, Telksnys T, Trumbeckas D, Jievaltas M, Milonas D (2016) Evaluation of LRINEC scale feasibility for predicting outcomes of Fournier gangrene. Surg Infect 17:448–453
Putnam LR, Richards MK, Sandvall BK, Hopper RA, Waldhausen JH, Harting MT (2016) Laboratory evaluation for pediatric patients with suspected necrotizing soft tissue infections: a case-control study. J Pediatr Surg 51:1022–1025
Burner E, Henderson SO, Burke G, Nakashioya J, Hoffman JR (2016) Inadequate sensitivity of laboratory risk indicator to rule out necrotizing fasciitis in the emergency department. West J Emerg Med 17:333–336
Tan JH, Koh BT, Hong CC et al (2016) A comparison of necrotising fasciitis in diabetics and non-diabetics: a review of 127 patients. Bone Joint J 98-B:1563–1568
Bechar J, Sepehripour S, Hardwicke J, Filobbos G (2017) Laboratory risk indicator for necrotising fasciitis (LRINEC) score for the assessment of early necrotising fasciitis: a systematic review of the literature. Ann R Coll Surg Engl 99:341–346
Neeki MM, Dong F, Au C, Toy J, Khoshab N, Lee C, Kwong E, Yuen H, Lee J, Ayvazian A, Lux P, Borger R (2017) Evaluating the laboratory risk indicator to differentiate cellulitis from necrotizing fasciitis in the emergency department. West J Emerg Med 18:684–689
Narasimhan V, Ooi G, Weidlich S, Carson P (2017) Laboratory Risk Indicator for Necrotizing Fasciitis score for early diagnosis of necrotizing fasciitis in Darwin. ANZ J Surg 87:1062
Zemplenyi K, Lopez B, Sardesai M, Dillon JK (2017) Can progression of odontogenic infections to cervical necrotizing soft tissue infections be predicted? Int J Oral Maxillofac Surg 46:181–188
El-Menyar A, Asim M, Mudali IN, Mekkodathil A, Latifi R, Al-Thani H (2017) The laboratory risk indicator for necrotizing fasciitis (LRINEC) scoring: the diagnostic and potential prognostic role. Scand J Trauma Resusc Emerg Med 25:28
Poeze M, Greve JWM, Ramsay G (1996) Necrotizing Fasciitis. In: Vincent J-L (ed) Yearbook of intensive care and emergency medicine. Springer, Berlin, pp 533–541
Chaudhry AA, Baker KS, Gould ES, Gupta R (2015) Necrotizing fasciitis and its mimics: what radiologists need to know. Am J Roentgenol 204:128–139
Fugitt JB, Puckett ML, Quigley MM, Kerr SM (2004) Necrotizing fasciitis. Radiographics 24:1472–1476
Malghem J, Lecouvet FE, Omoumi P, Maldague BE, Vande Berg BC (2013) Necrotizing fasciitis: contribution and limitations of diagnostic imaging. Joint Bone Spine 80:146–154
Hayeri MR, Ziai P, Shehata ML, Teytelboym OM, Huang BK (2016) Soft-tissue infections and their imaging mimics: from cellulitis to necrotizing fasciitis. Radiographics 36:1888–1910
Patterson JW (2013) Infectious diseases, including infestations and parasitic diseases. In: Patterson JW (ed) Practical skin pathology: a diagnostic approach. Elservier Saunders, Philadelphia, pp 251–314
Ferrara SD, Baccino E, Boscolo-Berto R et al (2016) Padova charter on personal injury and damage under civil-tort law : medico-legal guidelines on methods of ascertainment and criteria of evaluation. Int J Legal Med 130:1–12
Author information
Authors and Affiliations
Corresponding author
Additional information
Paolo Fais and Alessia Viero have equally contributed to the manuscript and should be both considered first authors. They are both Members of the International Academy of Legal Medicine (IALM); Alessia Viero is less than 35 years-old and belongs to the IALM Youth Section.
Electronic supplementary material
Fig. 1 – Electronic Source 1
Histological pattern of necrotizing fasciitis characterized by: interstitial oedema (A, EE 100×), necrosis (B, EE 100×), haemorrhagic infiltration (C, EE 400×), and bacterial colonies (C, EE 400× - D, EE 200× – E, Giemsa 200×) along the subcutaneous fasciae. The inflammatory reaction is minimal or absent in the subcutaneous fat tissues (F, EE 200×). (GIF 422 kb)
Table A - Electronic Source 2
Literature data from internationally published papers dealing with post-mortem cases of NF investigated through (at least) an autopsy with or without histology and/or microbiology analyses are here summarized. For each included manuscript, the classification used by the Journal (paper type), the number of cases investigated (cases), the type of histology (histopathology) and microbiological investigations (microbiology) performed are presented. The last column reports the time frame (in hours) between medical consultation/hospital admission and death. (DOCX 38 kb)
Table B - Electronic Source 3
Literature data on the diagnostic efficiency of LRINEC. For each included manuscript, first author, year of publication, number of investigated cases, type of investigation, cut-off used for the LRINEC score, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and area under the curve (AUC) are reported. (DOCX 29 kb)
Rights and permissions
About this article
Cite this article
Fais, P., Viero, A., Viel, G. et al. Necrotizing fasciitis: case series and review of the literature on clinical and medico-legal diagnostic challenges. Int J Legal Med 132, 1357–1366 (2018). https://doi.org/10.1007/s00414-018-1838-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-018-1838-0