Abstract
In this article scenarios have been developed, which simulate screening effects in ecological and cohort studies of thyroid cancer incidence among Ukrainians, whose thyroids have been exposed to 131I in the aftermath of the Chernobyl accident. If possible, the scenarios were based on directly observed data, such as the population size, dose distributions and thyroid cancer cases. Two scenarios were considered where the screening effect on baseline cases is either equal to or larger than that of radiation-related thyroid cancer cases. For ecological studies in settlements with more than ten measurements of the 131I activity in the human thyroid in May–June 1986, the screening bias appeared small (<19%) for all risk quantities. In the cohort studies, the excess absolute risk per dose was larger by a factor of 4 than in the general population. For an equal screening effect on baseline and radiation-related cancer (Scenario 1) the excess relative risk was about the same as in the general population. However, a differential screening effect (Scenario 2) produced a risk smaller by a factor of 2.5. A comparison with first results of the Ukrainian–US-American cohort study did not give any indication that a differential screening effect has a marked influence on the risk estimates. The differences in the risk estimates from ecological studies and cohort studies were explained by the different screening patterns in the general population and in the much smaller cohort. The present investigations are characterized by dose estimates for many settlements which are very weakly correlated with screening, the confounding variable. The results show that under these conditions ecological studies may provide risk estimates with an acceptable bias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Starting from 1990, thyroid cancer incidence increased markedly in the birth-year group 1968–1985 in areas, which were radioactively contaminated as a consequence of the accident at the Chernobyl nuclear power plant (NPP) in April 1986. This increase is analysed by epidemiological studies in order to estimate the health impact of the accident and to better understand thyroid cancer risk after incorporation of radioactive iodine. Recently, results of three types of epidemiological studies of thyroid cancer after Chernobyl have been published: case–control studies, cohort studies and ecological studies. All the three study types have merits and short-comings.
Case–control studies, which are not analysed here, easily control for confounders but typically Chernobyl studies (Davis et al. 2004; Cardis et al. 2005; Kopecky et al. 2006) have to cope with large dose uncertainties.
Screening, which is considered as the main potential confounding factor, is adequately controlled in cohort studies (Tronko et al. 2003, 2006; Stezhko et al. 2004). Every cohort member is screened for thyroid diseases by the same procedure. However, this intensive screening causes different excess risks per dose in the cohort and in the general population. Obviously, due to intensive screening the excess absolute risk per dose will be higher in the cohort than in the general population. Concerning the excess relative risk of thyroid cancer after external exposure to ionizing radiation, it was shown that the best estimate of age- and sex-adjusted risk decreased by a factor of 5 after the introduction of screening (Schneider et al. 1993). For this reason there is some concern that the excess relative risk per dose in the cohort study of thyroid cancer after the Chernobyl accident might well be smaller than in the general population.
Ecological studies (Ivanov et al. 2003, 2006; Jacob et al. 2006a; Likhtarov et al. 2006) have the advantage of large statistical power. Their disadvantage is the potential for a so-called ecological bias (see Wakefield 2004 for a recent summary). In studies of lung cancer risk after radon exposure, Lubin (1998, 2002) has demonstrated how a bias arises if smoking acts as a confounder. Compared to thyroid cancer there is a conceptual difference. Lung cancer is caused biologically by both radiation and smoking, whereas screening merely increases the number of reported thyroid cancer cases. For thyroid cancer after the Chernobyl accident an ecological bias may be caused especially by correlations between thyroid dose and screening. Nevertheless, both smoking and screening, if correlated with radiation dose, could operate as a confounder and are therefore treated here with the same mathematical framework.
In summary, the influence of screening on the results of risk estimates for thyroid cancer incidence after the Chernobyl accident is of major concern in both cohort and ecological studies. This questions the applicability of the study results e.g. for the planning of iodine prophylaxis in the case of a large nuclear accident.
There are at least four different aspects of screening after the Chernobyl accident:
-
dedicated screening programs (for a summary see Jacob et al. 2006b)
-
the introduction of ultra-sound examinations (Likhtarov et al. 2006)
-
an increased surveillance of the thyroid during regular medical examinations
-
the installation of a registry for thyroid cancer after the Chernobyl accident (Tronko et al. 1999; Kopecky et al. 2006).
Throughout this article screening is used as a synonym for increased case detection and reporting caused by these four aspects.
Scenarios are developed here, which allow the quantification of the influence of screening on the thyroid cancer incidence after the Chernobyl accident. Thyroid cancer data, which are compatible with originally recorded data, are simulated. The simulated data are analysed according to simplified protocols as used in cohort and ecological studies. The aim of the present article is to assess the effect of screening on risk estimates and to relate the results attained in the two study types to the risk in the population. As a first step, only correlations between settlement-averages of
-
screening and baseline incidence without screening, and
-
screening and thyroid dose
are considered. As a further simplification, any dependence on sex, age and age-at-exposure is neglected.
Materials and methods
Both, the recent ecological studies (Jacob et al. 2006a; Likhtarov et al. 2006) and the Ukrainian–US-American cohort study (Tronko et al. 2003, 2006) are based on measurements of the 131I activity in the human thyroid, which have been performed during May–June 1986 (Likhtarov et al. 2005). The data set consists of more than 70,000 measured subjects. Cohort members have been selected from the measured subjects and one of the ecological studies (Jacob et al. 2006a) included only those settlements in which more than ten of such measurements had been performed. The scenarios developed here for the simulations are also based on the 131I measurements. For the birth-year group 1968–1985, thyroid cancer cases are considered which have been operated during 1990–2001.
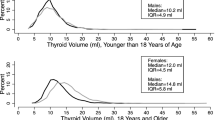
The simulated ecological study includes 605 settlements, where more than 10 measurements of the 131I content in the human thyroid have been measured during May–June 1986 (Fig. 1). The larger cities of Chernihiv and Zhytomyr are counted among the settlements which increases the total number to 607. The settlements j are located in the three highly contaminated Ukrainian oblasts (regions) k of Chernihiv, Kyiv (excluding Kyiv City) and Zhytomyr. The mean thyroid doses \(D_{jk}\) in the single settlements range from 0.025 to 6.5 Gy (Fig. 2). The mean doses \(D_k\) of the study population in oblast k are given in Table 1. The mean thyroid dose for the total study population \(D_{\rm{pop}}\) is 0.14 Gy.
Number of children and adolescents, and estimated arithmetic mean doses for 605 Ukrainian settlements (open circles), plus the cities of Chernihiv and Zhytomyr (filled circles) (Likhtarov et al. 2005)
The simulated cohort includes 11,571 subjects with birth year between 1968 and 1985 like the cohort of the Ukrainian–US-American study (Tronko et al. 2003). Members of the simulated cohort were sampled from the simulated population in the ecological study. The mean thyroid dose for the Ukrainian–US-American cohort D coh is 0.78 Gy. In order to make the results of the simulated ecological and cohort studies comparable, the follow-up in the cohort study was assumed to be 1990–2001. The actual follow-up in the Ukrainian–US-American study did not start before 1998.
Basic equations for the hazard and definition of two scenarios
The hazard for an unscreened subject i is defined by
where h 0 is the baseline hazard without screening, β the excess absolute risk per thyroid dose without screening, and D i the simulated thyroid dose. For a screened subject the hazard function is modelled by
where \(\eta_{\rm{sc}}\) is the excess relative baseline rate due to screening, and \(\kappa_{\rm{sc}}\) the excess relative radiation-induced rate due to screening.
The hazard for an individual i in a settlement j of an oblast k in the simulated ecological study is modelled as
where \(h_{0k}\) is the baseline hazard in oblast k. The individual excess relative rates \(\eta_{ijk}\) and \(\kappa_{ijk}\) of screened subjects are equal to \(\eta_{\rm{sc}}\) and \(\kappa_{\rm{sc}},\) respectively. For unscreened subjects they are zero.
The average baseline hazard without screening is
where \(N_k\) is the study population in oblast k, and \(N_{\rm{pop}}\) is the whole population of the ecological study.
Since the cohort members all originate from the settlements of the ecological study, it is assumed here for simplicity that the baseline rate without screening in the cohort is the same as the average baseline rate in the population.
The average excess relative rates due to screening in the population are given by
Then the baseline risk \(h_{0,pop},\) excess absolute risk per dose \(\beta_{\rm{pop}}\) and the excess relative risk per dose \(\gamma_{\rm{pop}}\) in the population are
All the subjects in the cohort have been screened. For simplicity, it is assumed that the excess relative rates, which quantify the screening effect, are the same for cohort members and for screened subjects of the general population. Then the hazard of all cohort members is given by (2).
Two scenarios are considered. In the first scenario it is assumed that screening has the same relative effect on spontaneous and on radiation-induced thyroid cancer hazard, thus \(\kappa_{\rm{sc}}\) equals \(\eta_{\rm{sc}}.\)
The second scenario is motivated by a thyroid cancer study at the Michael Reese Hospital in Chicago (Schneider et al. 1993). In this hospital screening was introduced in 1974. The best estimate of the age and sex adjusted excess relative risk after 1974 was by a factor of 5 smaller than before 1974. Motivated by this observation, for the second scenario \(\kappa_{\rm{sc}}/\eta_{\rm{sc}}=0.2\) is assumed. Note, that this is a ratio of excess relative rates, which does not imply a five-fold rise of the baseline rate.
Thus, in this scenario the effect of screening on baseline cases is more pronounced than for radiation-induced cases. This would occur if the increase of the incidence rate is mainly due to the detection of occult thyroid cancer cases, and if radiation-induced thyroid cancer cases are less often occult in the observation period than baseline cancer cases. Thyroid cancer cases are called occult, if the tumour stops growth at a certain stage and therefore does not cause any health consequences. Autopsy studies suggest that occult thyroid cancers are found in about 10% of the general population (Fransilla et al. 1986; Lang et al. 1988). In the light of this discussion, the first scenario would imply that the number of occult cancers, detected by screening, is small and does not influence the risk estimates.
Data on thyroid cancer incidence rates
Baseline rates
The baseline incidence rate, i.e., the incidence rate of cases which were not associated with radiation, increases with attained age a (Whelan et al. 2003). In the contaminated area, the baseline rate also increased as a function of calendar year y, because screening added a significant number of cases after the accident. Jacob et al. (2006b) estimated the time-dependent baseline rate \(\lambda_{0k}(y,\,a,\,s)\) in three groups of Ukrainian and Belarusian oblasts with high, middle and low thyroid cancer incidence as a function of calendar year y, age attained a and sex s . The functional form of \(\lambda_{{0}k}(y,\,a,\,s)\) is determined by eight parameters which have been estimated with Poisson regression. To group the oblasts, two values for the baseline incidence rate were calculated by subtracting the radiation-induced incidence with an assumed excess relative risk of 10 Gy−1 from the total incidence rate. The two values were chosen such that each group included approximately the same number of oblasts. The Chernihiv and Kyiv oblasts belonged to the group of high incidence, while the Zhytomyr oblast belonged to the group of medium incidence.
It is assumed here that the oblast-specific results of Jacob et al. (2006b) also apply to the study settlements. The baseline rate averaged over calendar year, age group and sex in the study settlements in oblast k can then be assessed by
where b denotes the birth year, s = 1 stands for males, and s = 2 for females (Table 1).
Assuming that the period 1986–1989 corresponds to a period without screening, the average excess relative rate of the baseline cases in oblast k due to screening during 1990–2001 is given by
The attained age \(y-b\) has been fixed to 18 years to exclude the influence of an ageing cohort. Hence, the effect of screening is determined by the ratio of two baseline rates, averaged over follow-up periods with and without screening, for a cohort with members of both sexes at age 18.
As a result, the excess relative increase of the baseline rate due to screening in Chernihiv and Kyiv oblasts is assessed to be about 1.5, and in Zhytomyr oblast about 0.6. Thus, there is an unexpected negative correlation between screening and thyroid dose (Table 1). This might be due to the fact that the screening intensity decreases with increasing distance from the Chernobyl NPP. Compared to the oblasts of Kyiv and Chernihiv, in Zhytomyr oblast includes more highly contaminated settlements further away from the NPP (Fig. 1). This asymmetry could explain both the lower excess relative increase in Zhytomyr and the negative correlation with exposure, respectively.
For the whole study population an excess relative baseline rate, \(\eta_{\rm{pop}},\) of 1.1 is obtained corresponding to an increase of the baseline incidence rate due to screening by a factor 2.1.
Population data and total rates
The USSR-wide census in 1989 (USSR 1991) has been used to determine the population \(N_{jk}\) in settlement j of oblast k. The oblast-specific populations \(N_{k}\) are given in Table 1. The total study population \(N_{\rm{pop}}\) was 347,022 subjects, including about 80,000 subjects in each of the larger towns Zhytomyr and Chernihiv. The majority of settlements consists of small villages with about 100 children and adolescents (Fig. 2).
In the study population and for the period 1990–2001, a total number \(n_{\rm{pop}}\) of 215 cancer cases were reported to the Thyroid Cancer Registry established at the Ukrainian Institute of Endocrinology and Metabolism of the Academy of Medical Sciences (Tronko et al. 1999, 2003). Assuming that the total thyroid cancer hazard in the study population is given by the incidence rate during the observation time Δt of 12 years
a value of 5.2 cases per 105 PY is obtained.
A second screening in the cohort gives information on the thyroid cancer incidence rate among Ukrainians, who are screened for thyroid diseases: 21 new cancer cases were found among the 11,571 cohort members in a 2.5-year period starting in 2001. Thus, the total incidence rate in the Ukrainian–US-American cohort h UA was 73 cases per 105 PY.
Determination of scenario-dependent parameters
In the Appendix it is shown that
Thus, any correlations between \(\eta_k\) and \(h_{0}k,\) and between \(\kappa_k\) and \(D_k\) could possibly play an important role in the risk determination. According to (10), the excess absolute risk per dose without screening, β, in the first scenario corresponds to 0.79 cases per 104 PY Gy, while in the second scenario β corresponds to 1.34 cases per 104 PY Gy.
The total hazard in the Ukrainian–US-American cohort study may be written as
where A is a factor expressing the ageing of the cohort from the observation period of the present study (1990–2001) to the second screening period of the Ukrainian–US-American cohort study. For A a value of 1.8 was obtained from
Equation 12 may be solved for \(\eta_{\rm{sc}}\) :
The resulting values for \(\eta_{\rm{sc}}\) are 7.6 for Scenario 1, and 13.6 for Scenario 2.
Finally, for the ecological study, the fraction of individuals who have been screened is determined according to
Table 2 summarizes the parameter values used in the two scenarios.
Simulation of individual thyroid dose and health status
Thyroid dose
For each individual i in settlement j in oblast k, a thyroid dose \(D_{ijk}\) was sampled from a lognormal distribution with average value \(D_{jk}\) (Fig. 2), as derived by Likhtarov et al. (2005), using a geometrical standard deviation of 2.8.
For the simulated cohort members were sampled from the simulated population in the ecological study in such a way that the distribution of cohort members in five dose groups and their average dose is the same as in the Ukrainian–US-American study (Table 3).
Health status
In the simulation of the cohort study, all cohort members were assumed to have been screened. In the simulation of the ecological study, the individual screening status is sampled at random for each oblast k according to the screening probability \(z_k.\)
For the cohort studies the health status was determined from the individual hazard of (2) with the probability
while for the ecological studies it was determined with
using the hazard of (3) (Kalbfleisch and Prentice 1980).
The probability of (15) or (16) was compared with a random number P, which was evenly distributed between 0 and 1. If \(P_{\rm{coh},i} \geq P\) or \(P_{ijk} \geq P\) a tumour case was assigned to the individual. Competing risks were not considered because they were small for subjects below age 31 which was the average age of the birth cohort 1968 in the year 2001.
Statistical analysis
For the simulation of the ecological study, means of the thyroid dose and incidence rates in the 607 settlements were calculated from the simulated data for the 347,022 members of the study population. Poisson regressions of these data were performed with a simple excess absolute risk model
and with a simple excess relative risk model
where \(\hat{h}_{0 {\rm {eco}}},\; \hat{\beta}_{\rm{eco}}\hbox{ and } \hat{\gamma}_{\rm{eco}}\) were fit parameters.
Poisson regressions were performed for the 11,571 cohort members in the dose groups given in Table 3 with the excess absolute risk model
and with the excess relative risk model
where \(\hat{h}_{0 {\rm coh}}\), \(\hat{\beta}_{\rm{ coh}}\) and \(\hat{\gamma}_{\rm{coh}}\) are fit parameters.
These regressions produce best estimates and confidence bands of the risk coefficients. The simulation has been repeated 1,000 times with different random numbers, in order to determine the distributions of the best estimates.
Results
Ecological study
According to the risk parameters derived with the underlying models, the number of thyroid cancer cases in the population of the simulated ecological studies is about the same in both scenarios. The distribution of the thyroid cancer cases in the 1,000 simulations yielded an average of 214 cases with a 95% frequency band of (185, 243). This corresponds well to a Poisson distribution with an expectation value close to the number of 215 cases, which have been observed in the study areas during 1990–2001.
The median values of risk estimates in the simulated ecological studies reproduce the ‘true’ model values in the study population quite well (Table 4). For all risk quantities, the difference is less than 20% for both scenarios. The largest ecological bias of 19% is found in Scenario 2 for the median value \(\hat{\gamma}_{\rm{eco}}\) of the estimated excess relative risk per dose. This bias can still be considered as moderate. It is the net result of correlations between baseline risk, screening and dose.
Risk estimates in single ecological studies may deviate considerably from the true values in the underlying model. In most of the simulations, the baseline hazard is correctly estimated within 30%, the excess absolute risk per dose within a factor of 1.5, and the excess relative risk per dose within a factor of 2. The results obtained for the two scenarios are quite similar.
Besides the best estimates of the risk values, each of the 1,000 simulated studies provided also uncertainty bands. The averages of the 95% uncertainty bands (results not shown) were very close to the 95% frequency bands of the best estimates given in Table 4. The largest difference was found in Scenario 1 for the upper limit of the confidence band for \(\hat{\gamma}_{\rm{eco}}.\) In the distribution of the 1,000 best estimates, this value was 12.8 Gy−1, while the average of the 1,000 upper limits of the uncertainty bands was 13.7 Gy−1. Thus, the uncertainty band of a risk parameter from Poisson regression was indeed a good estimate for the width of the simulated parameter distribution.
Cohort study
The expectation values of the number of thyroid cancer cases in the simulated cohort studies was 88 in Scenario 1 and 80 in Scenario 2. The distributions of the thyroid cancer cases in the 1,000 simulations corresponded closely to a Poisson distribution with these expectation values.
Several of the median values of risk estimates in the simulated cohort studies differ considerably form the risk values in the underlying model for the general population (Table 5). For Scenario 1, the baseline incidence rate in the simulated cohort and the excess absolute risk per dose are about a factor of 4 higher than in the simulated general population. The median value of the estimated excess relative risk per dose, however, is in the cohort quite close to the corresponding value in the population.
For Scenario 2, the differential screening effect for spontaneous and radiation-related thyroid cancers results in an excess relative risk per dose in the cohort lower by a factor of 2.5, when compared to the corresponding value in the population.
Concerning the excess absolute risk per unit dose, the simulated cohort studies have shown a considerable statistical power. The 95% frequency ranges of the estimated values are quite small, e.g. from 4.8 to 8.4 per 104 PY Gy in Scenario 1. However, the statistical power is lower for the baseline incidence rate, and consequently also for the excess relative risk per dose. In Scenario 1 the uncertainty band for the excess relative risk per dose spans one order of magnitude (from 2.4 to 31 Gy−1).
Comparison of the two study types
Compared to the simulated ecological studies, the excess absolute risk per dose in the simulated cohort studies is larger and has a broader distribution (Fig. 3). This finding is about the same in both scenarios.
Frequency distributions of best estimates of the excess absolute risk per dose. \(\beta_{\rm{pop}}\) indicates the excess absolute risk per dose in the underlying model for the general population, \(\hat{\beta}_{\rm{eco}}\) indicates the median value of the best estimates in the simulated ecological studies, and \(\hat{\beta}_{\rm{coh}}\) indicates the median value of the best estimates in the simulated cohort studies
While the results of the two study types for the excess relative risk per dose agree quite well in Scenario 1 (Fig. 4, upper panel), in Scenario 2 the corresponding estimate in the cohort study is by a factor of 3 lower than in the ecological study. In absolute terms this difference between the values of Tables 4 and 5 amounts to 4.9 Gy−1 . It can be divided into a contribution from the ecological bias of 1.2 Gy−1 plus a contribution of 3.7 Gy−1 from the difference between the excess relative risk in the cohort and in the general population (Fig. 4, lower panel).
Frequency distributions of best estimates of the excess relative risk per dose. \(\gamma_{\rm{pop}}\) indicates the excess relative risk per dose in the underlying model for the general population, \(\hat{\gamma}_{\rm{eco}}\) indicates the median value of the best estimates in the simulated ecological studies, and \(\hat{\gamma}_{\rm{coh}}\) indicates the median value of the best estimates in the simulated cohort studies
Discussion
Screening scenarios
In the present article, scenarios have been developed, which simulate ecological and cohort studies on thyroid cancer incidence among Ukrainians, whose thyroids were exposed to 131I during childhood and adolescence. Efforts were made to base the scenarios on directly observed data, that reflect the populations, dose distributions and thyroid cancer cases in published ecological (Jacob et al. 2006a) and cohort (Tronko et al. 2006) studies, and on estimates of baseline incidence rates and their regional and temporal dependencies as derived from register data (Jacob et al. 2006b).
The screening scenarios exhibit within the study area a negative correlation between the excess relative rate due to screening and thyroid dose. In contrast, a positive correlation between the number of ultra-sound examinations in the total area of the oblast and the average dose in the study population has been reported (Likhtarov et al. 2006). Although the number of ultra-sound examinations need not necessarily be the dominating factor for the screening effect during the study period of 1990–2001, this apparent discrepancy deserves further exploration.
Best estimates of risk values
The result of the simulated ecological studies for the excess absolute risk per dose of 1.8 per 104 PY Gy agrees well with published results of 1.53 (1.19, 1.88) per 104 PY Gy for Ukrainian settlements (Likhtarov et al. 2006) and of 2.66 (2.19, 3.13) per 104 PY Gy for Belarusian and Ukrainian settlements, where the estimate for Belarus was by a factor of 1.36 higher than the estimate for Ukraine (Jacob et al. 2006a). Also in very good agreement are the estimates from the ecological study of Ivanov et al. (2006) in the Russian oblast of Bryansk: in the follow-up period 1991–2001 an excess absolute risk of 1.8 (1.0, 2.9) per 104 PY Gy was found for girls between 0 and 14 years. For boys the result was 2.0 (1.1, 3.0) per 104 PY Gy.
Published ecological studies for settlements with measurements of the 131I activity in the human thyroid resulted in estimates of the excess relative risk per dose of 8.0 (4.6, 14.7) Gy−1 in the Ukraine (Likhtarov et al. 2006), and of 18.9 (11.1, 26.7) Gy−1 in Belarus and Ukraine, where the estimate for Belarus was by a factor of 1.64 larger in Belarus than in Ukraine (Jacob et al. 2006a). The Ukrainian–US-American cohort study (Tronko et al. 2006) resulted in a value of 5.3 (1.7, 28) Gy−1 for thyroid cancer prevalence in the first screening period 1998–2000. All three studies are consistent with an excess relative risk per dose in the Ukrainian settlements of about 10 Gy−1 which was assumed by Jacob et al. (2006b) to determine baseline rates. The Russian study (Ivanov et al. 2006) reports a compatible risk estimate for girls. For boys, however, the risk was much higher, possibly due to the low number of cases.
The results of the present simulations of ecological studies and of the cohort study in Scenario 1 are also consistent with a value of 10 Gy−1 . The result of the simulated cohort study in Scenario 2, however, is markedly lower. It is of particular interest that the results of the simulated cohort study in Scenario 1 and of the Ukrainian–US-American study are practically the same. Thus, if a future analysis of the incidence of the Ukrainian–US-American cohort confirms the results for the prevalence, then the present simulation study does not give any indication that a differential effect of screening on baseline and on radiation-induced thyroid cancer cases influences the relative risk estimate in the cohort study.
Uncertainty ranges
Thyroid cancer is a rare disease. Correspondingly, a cohort study on thyroid cancer needs to be very large. Although the Ukrainian–US-American study is quite large, uncertainty ranges of relative risk estimates are about one order of magnitude. Similar ranges were observed in the simulated cohorts with some 80 cancer cases. Increasing the number of cases to more than 200 in the ecological studies reduces the uncertainty ranges up to a factor of 3, mainly due to a reduction of the upper bound.
Case–control studies have not been analysed in the present paper but their results deserve to be cited. Although case–control studies can control for confounders, their main weakness in the field of thyroid cancer after the Chernobyl accident is the large uncertainty of the individual dose estimates. Usually, these estimates are not based on individual measurements, and in many cases measurements of the 131I activity in the human thyroid have even not been performed for other residents of the investigated settlements. These large dose uncertainties may have been one reason for the contradicting results, which have been obtained in case–control studies. For example, an estimate of the excess relative risk per dose of 1.65 (0.10, 3.20) Gy−1 was obtained by Davis (2004), and an estimate of 49 (5, 1151) Gy−1 by Kopecky (2006). Estimates that are more in line with results of other studies have been reported in a case–control study of Cardis et al. (2005). However, corrections for the large dose uncertainties still need to be performed here.
Conclusions
The simulations presented in this paper address two important issues for risk studies of thyroid cancer that are being performed more than 20 years after the Chernobyl accident.
-
The size of a bias in ecological studies, which is caused by uncontrolled confounders such as screening, has been assessed.
With the given study design the ecological bias is negligible, if occult cancers played no role, like in screening Scenario 1. Even if a substantial number of occult thyroid cancers were found (Scenario 2), the bias remained moderate with a relative deviation from the population-wide risk of up to 19%. There might be ecological biases due to screening distributions other than those simulated in the present paper, or due to other confounding variables, such as the supply with stable iodine (Cardis et al. 2005; Shakhtarin et al. 2003). It is noteworthy, however, that central relative risk estimates of the ecological studies in settlements with measurements of the 131I activity of the human thyroid agree quite well with the result for the simulated cohort study of the first scenario, with the preliminary result of the Ukrainian–US-American cohort study and with the average of the risk estimates obtained in the various case–control studies.
-
The results of recent cohort studies (Tronko et al. 2003, 2006; Stezhko et al. 2004) and ecological studies (Ivanov et al. 2006; Jacob et al. 2006a; Likhtarov et al. 2006) have been put into perspective and the different risk estimates have been explained. Due to a more intensive screening, the excess absolute risk per dose in a cohort was larger by some factor 3–4, when compared to the risk in the population. The excess relative risk was more sensitive to the differential effect of screening on spontaneous and radiation-related thyroid cancer cases. However, the concern that this effect may influence the estimate of the excess relative risk has not been supported by the present simulation study.
To conclude, the detailed dose estimates for many settlements with a weak correlation to screening as the confounding variable provided favourable conditions for the present ecological studies to produce risk estimates with an acceptable bias. Ecological studies explore the mean population-wide risk using aggregate data for a large part of the exposed population. The scope of cohort studies is different: what is the risk for a much smaller part of the population under a regime of very intense screening? They are better suited to quantify the actual radio-biological risk. But it was shown that care must be taken when transferring this risk to the general population.
References
Cardis E, Kesminiene A, Ivanov V, Malakhova I, Shibata Y, Khrouch V, Drozdovitch V, Maceika E, Zvonova I, Williams D (2005) Risk of thyroid cancer after exposure to 131I in childhood. J Natl Cancer Inst 97:724–732
Davis S, Stepanenko V, Rivkind N, Kopecky KJ, Voillequé P, Shakhtarin V, Parshkov E, Kulikov S, Lushnikov E, Abrosimov A, Troshin V, Romanova G, Doroschenko V, Proshin A, Tsyb A (2004) Risk of thyroid cancer in the Bryansk oblast of the Russian Federation after the Chernobyl power station accident. Radiat Res 162:241–248
Franssila KO, Harrach HR (1986) Occult papillary carcinoma of the thyroid in children and young adults. Cancer 58:715–719
Ivanov VK, Gorski AI, Maksioutov MA, Vlasov OK, Godko AM, Tsyb AF, Tirmarche M, Valenty M, Verger P (2003) Thyroid cancer incidence among adolescents and adults in the Bryansk region of Russia following the Chernobyl accident. Health Phys 84(1):46–60
Ivanov VK, Gorski AI, Tsyb AF, Maksioutov MA, Tumanov KA, Vlasov OK (2006) Radiation-epidemiological studies of thyroid cancer incidence among children and adolescents in the Bryansk oblast of Russia after the Chernobyl accident (1991–2001 follow-up period). Radiat Environ Biophys 45(1):9–16
Jacob P, Bogdanova TI, Buglova E, Chepurniy M, Demidchik Y, Kenigsberg J, Meckbach R, Schotola C, Shinkarev S, Tronko MD, Ulanovsky A, Vavilov S, Walsh L (2006a) Thyroid cancer risk in areas of Ukraine and Belarus affected by the Chernobyl accident. Radiat Res 165:1–8
Jacob P, Bogdanova TI, Buglova E, Chepurniy M, Demidchik Y, Gavrilin Y, Kenigsberg J, Kruk J, Schotola C, Shinkarev S, Tronko MD, Vavilov S (2006b) Thyroid cancer among Ukrainians and Belarussians, who were childrens or adolescents at the time of the Chernobyl accident. J Radiol Prot 26:51–67
Kalbfleisch JD, Prentice RL (1980) The statistical analysis of failure time data. Wiley, New York
Kopecky KJ, Stepanenko V, Rivkind N, Voillequé P, Onstad L, Shaktarin V, Parshkov E, Kulikov S, Lushnikov E, Abrosimov A, Troshin V, Romanova G, Doroschenko V, Proshin A, Tsyb A, Davis S (2006) Childhood thyroid cancer, radiation dose from Chernobyl, and dose uncertainties in Bryansk oblast, russia: a population-based case control study. Radiat Res 166:367–374
Lang W, Borrush H, Bauer L (1988) Occult carcinomas in the thyroid. Evaluation of 1020 sequential autopsies. Am J Clin Pathol 90:72–76
Likhtarov I, Kovgan L, Vavilov S, Chepurny M, Bouville A, Luckyanov N, Jacob P, Voillequé P, Voigt G (2005) Post-Chernobyl thyroid cancers in Ukraine. Report 1: estimation of thyroid doses. Radiat Res 163:125–136
Likhtarov L, Kovgan L, Vavilov S, Chepurny M, Ron E, Lubin J, Bouville A, Tronko N, Bogdanova T (2006) Post-Chernobyl thyroid cancers in Ukraine, Report 2: risk analysis. Radiat Res 166:375–386
Lubin JH (1998) On the discrepancy between epidemiologic studies in individuals of lung cancer and residential radon and Cohen’s ecologic regression. Health Phys 75(1):4–20
Lubin JH (2002) The potential for bias in Cohen’s ecological analysis of lung cancer and residential radon. J Radiol Prot 22:141–148
Schneider AB, Ron E, Lubin J, Stovall M, Gierlowski TC (1993) Dose–response relationships for radiation-induced thyroid cancer and thyroid nodules: evidence for the prolonged effect of radiation on the thyroid. J Clin Endocrinol Metab 77:362–369
Shakhtarin V, Tsyb A, Stepanenko V, Orlov M, Kopecky K, Davis S (2003) Iodine deficiency, radiation dose, and the risk of thyroid cancer among children and adolescents in the Bryansk region of Russia following the Chernobyl power station accident. Int J Epidemiol 32:584–591
Stezhko VA, Buglova EE, Danilova LI, Drozd VM, Krysenko NA, Lesnikova NR, Minenko VF, Ostapenko VA, Petrenko SV, Polyanskaya ON, Rzheutski VA, Tronko MD, Bobylyova OO, Bogdanova TI, Ephstein OV, Kairo IA, Kostin OV, Likhtarev IA, Markov VV, Oliynik VA, Shpak VM, Tereshchenko VP, Zamotayeva GA, Beebe GW, Bouville AC, Brill AB, Burch JD, Fink DJ, Greenebaum E, Howe GR, Luckyanov NK, Masnyk IJ, McConnell RJ, Robbins J, Thomas TL, Voillequé PG, Zablotska LB (2004) A cohort study of thyroid cancer and other thyroid diseases after the Chernobyl accident: objectives, design and methods. Radiat Res 161:481–492. Chornobyl Thyroid Diseases Study Group of Belarus, Ukraine, and the USA
Tronko MD, Bogdanova TI, Komisarenko IV, Epshtein OV, Likhtaryov IA, Markov VV, Oliynyk VA, Tereshchenko VP, Shpak VM, Voillequé P (1999) Thyroid carcinoma in children and adolescents in Ukraine after the Chernobyl accident: statistical data and clinicomorphic characteristics. Cancer 86:149–156
Tronko MD, Bobylyova OO, Bogdanova TI, Epshtein OV, Likhtaryov IA, Markov VV, Oliynyk VA, Tereshchenko VP, Shpak VM, Beebe G, Bouville A, Brill A, Burch D, Fink D, Greenebaum E, Howe G, Luckyanov N, Masnyk I, McConnell R, Robbins J, Thomas T, Voillequé P (2003) Thyroid gland and radiation (Ukrainian–American thyroid project). In: Shibata Y, Yamashita S, Watanabe M, Tomonaga M (eds) Radiation and humankind. Elsevier, Amsterdam, vol 1258, International Congress Series, pp 91–104. Proceedings of the 1st Nagasaki symposium of the international consortium for medical care of Hibakusha and radiation life science, Nagasaki, Japan, 21–22 February 2003
Tronko MD, Howe GR, Bogdanova TI, Bouville AC, Epstein OV, Brill AB, Likhtarev IA, Fink DJ, Markov VV, Greenebaum E, Olijnyk VA, Masnyk IJ, Shpak VM, McConnell RJ, Tereshchenko VP, Robbins J, Zvinchuk OV, Zablotska LB, Hatch M, Luckyanov NK, Ron E, Thomas TL, Voillequé PG, Beebe GW (2006) A cohort study of thyroid cancer and other thyroid diseases after the Chernobyl accident: thyroid cancer in Ukraine detected during first screening. J Natl Cancer Inst 98:897–903
USSR (1991) The USSR 1989 census: the age-by-sex population distribution of the UkSSR. The UkSSR Ministry of Statistics Publication, Kiev
Wakefield J (2004) A critique of statistical aspects of ecological studies in spatial epidemiology. Environ Ecol Stat 11:31–54
Whelan SL, Ferlay J, Teppo L, Thomas DB (2003) Cancer incidence in five continents. International Agency for Research on Cancer, Lyon, vol VIII. IARC Scientific Publications No. 156
Acknowledgments
This work has been supported by the German Federal Minister of Environment, Nature Preservation and Reactor Safety and the German Federal Office of Radiation Protection under contract no. StSch 4299.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Summation of (3) and division by \(N_{\rm{pop}}\) yield
the thyroid cancer risk in the general population. With
and with \(\eta_{ijk}\) and \(\kappa_{ijk}\) being independent of i and j, it follows
With
and with the definition of \(h_0\) (4), (23) may be rewritten as
Solving this equation for β yields
Rights and permissions
About this article
Cite this article
Kaiser, J.C., Jacob, P., Blettner, M. et al. Screening effects in risk studies of thyroid cancer after the Chernobyl accident. Radiat Environ Biophys 48, 169–179 (2009). https://doi.org/10.1007/s00411-009-0211-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-009-0211-6