Abstract
The association between schizophrenia spectrum disorders (SSD) and violent behavior is complex and requires further research. The cognitive correlates of violent behavior, in particular, remain to be further investigated. Aims of the present study were to comprehensively assess the cognitive and clinical profile of SSD violent offenders and evaluate individual predictors of violent behavior. Fifty inmates convicted for violent crimes in a forensic psychiatry setting and diagnosed with SSD were compared to fifty non-offender patients matched for age, gender, education, and diagnosis. Offender and non-offender participants were compared based on socio-demographic, clinical, and cognitive variables using non-parametric testing to select potential predictors of violent behavior. Multivariate logistic regressions were then performed to identify individual predictors of violent behavior. Offender participants showed more school failures, higher prevalence of substance use, higher Clinical Global Impression Severity Scale (CGI-S) and Positive and Negative Syndrome Scale Excited Component (PANSS-EC) scores, worse working memory and better attention performance, higher Historical Clinical and Risk Management scale 20 (HCR-20) and Hare Psychopathy Checklist (PCL-R) scores in all subdomains and factors. School failures, higher PANSS-EC scores, worse working memory and processing speed, better attention performance, higher scores in HCR-20 Management subscale and the PCL-R “Callous” factor emerged as predictors of violent behavior. Better attentional performance was correlated with higher PCL-R “Callous” factor scores, worse cognitive performance in several domains with higher PCL-R “Unstable” factor scores. In conclusion, the present study highlights the importance of carefully assessing SSD patients with violent behavior in all clinical, cognitive, and behavioral aspects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
The association between severe mental illnesses and violent behavior is complex and represents a research topic of longstanding interest for its clinical, social, and public health repercussions [1, 2].
People living with severe mental illnesses are frequently victims of violence [3, 4]. In fact, violent victimization of people with severe psychiatric disorders is a frequent phenomenon, which carries a high risk of serious physical injuries; it also has an important negative impact on the quality of life and on the trajectory of the illness of victims, and is linked to stigma [5,6,7,8].
Some individual psychiatric disorders, however, are also associated with an increased relative risk of violent behavior [2, 9,10,11]. Individuals diagnosed with schizophrenia spectrum disorders (SSD) [12, 13] show a 6–10% prevalence of violent crime perpetration leading to arrest or conviction, which rises to more than 10% in people with substance use disorders [14, 15]. In fact, substance use represents the strongest single risk factor for violent behavior among people diagnosed with mental disorders [16, 17].
As violent crimes are events that could be preventable in some cases, identifying risk factors and clinical correlates in individuals living with mental disorders is of great relevance to recognize high-risk situation and implement preventive interventions and strategies. Beside substance use, male gender, low socio-economic status, homelessness, criminal history, parental violence, parental substance use, victimization, inpatient admission, previous self-harm and previous suicide attempts, all represent recognized risk factors for violence in subjects diagnosed with mental disorders [18,19,20,21]. Dynamic and modifiable factors include hostility, impulsivity and, particularly in psychotic disorders, lack of insight and treatment adherence and severe positive symptoms such as persecutory beliefs [22].
Alterations of cognitive performance are frequently observed in many psychiatric disorders and, in particular, those with higher violence risk such as SSD. Cognitive deficits represent one of the core features of SSD, with significant impairments in several neurocognitive domains as well as in social cognition performance [23,24,25,26], and cognitive deficits have been hypothesized as a risk factor for violent behavior in mental disorders. A meta-analysis conducted in 2014 and including 29 studies for a total of 4764 participants diagnosed with SSD [27] found that impaired global cognitive performance represents a significant predictor of violent aggression; however, a high degree of heterogeneity was observed, with single studies showing conflicting results. Moreover, important discrepancies were observed regarding individual cognitive domains: most analyses on single domains showed excessive heterogeneity or a non-significant effect of impaired cognitive performance, while, contrary to the expected, better motor functioning was associated with increased risk of violence.
Conflicting results can also be found in more recent literature, with some studies reporting that cognitive impairment does indeed represent a predictor of violent behavior in SSD [28, 29] and others reporting a better cognitive performance in violent patients [30].
These discrepancies suggest that a better characterization of the relationship between cognitive functioning and violence represents an issue that requires further investigation. Moreover, greater insight on this topic could provide further understanding of violence risk conditions, with potential research and real-world clinical implications. It could also provide opportunities to optimize treatment of people living with SSD and enhance violent acts prevention.
Conviction represents the most official and robust measure of violent outcomes as it overcomes recall-bias, inter-rater variability, and the risk of missing outcomes measurements [2]: in this context, offender SSD patients with better character in forensic contexts could provide valuable clinical insight.
Aims
The primary aim of the present study was to assess the cognitive profile, as well as clinical, impulsivity, aggression, and psychopathy correlates of offenders diagnosed with SSD (offender participants, OP), compared to non-offenders participants (non-OP) matched for age, gender, education, and diagnosis.
Secondary aim was to identify individual cognitive and clinical predictors belonging to the OP group, and to assess the clinical correlates of cognitive characteristics that emerged as significantly different in OP and non-OP. In fact, the primary hypothesis of this study is that OP might show a different cognitive profile, as well as higher levels of aggression risk and psychopathy.
Materials and methods
Sample
For the present study, 50 inmates convicted for violent crimes and enrolled in the Residences for the Execution of Security Measures in Castiglione delle Stiviere, Mantova, Italy were recruited from June 2018 to June 2020.
Inclusion criteria were: age between 18 and 65 years; main diagnosis of SSD according to the DSM- 5 criteria.
Exclusion criteria were: diagnosis of substance use disorder; main diagnosis of intellectual disability; presence of severe or neurodegenerative organic pathologies.
Non-OP were recruited in the same period and with the same inclusion and exclusion criteria among the patients of the Mental Health centers of the Spedali Civili Hospital in Brescia, Italy. They were matched on a 1:1 basis with OP for age, gender, education, and diagnosis.
Patients were informed about the study and were invited to participate through a written and signed consent form. The study was carried out in accordance with the Code of Ethics of the World Medical Association and the Declaration of Helsinki. The protocol was approved by the Ethical Committee of Brescia (Project Identification Code NP3060). All precautions were taken for the management of sensitive data, and participants were not given monetary compensation for their involvement in the study.
Measures
Socio-demographic information (age, gender, years of education, number of school failures, marriage status, work situation) was collected through a specific data collection form.
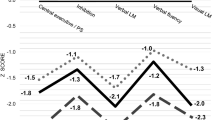
To provide a comprehensive assessment of the cognitive profile, participants were evaluated through the Brief Assessment of Cognition in Schizophrenia (BACS) [31], the Trail Making Test (TMT) [32] and the Stroop Color–Word Test (STROOP) [33]. Test performances were attributed to different cognitive domains according to previous meta-analytic literature [34, 35]: TMT-A: processing speed; TMT-B: working memory; TMT-B–A: executive functions; STROOP errors: attention; STROOP time: processing speed; BACS Word Recall: verbal memory; BACS Digit Sequencing: working memory; BACS Token Motor Task: processing speed; BACS Category Instances: fluency; BACS Symbol Coding: processing speed; BACS Tower of London: executive functions. Raw scores were corrected for age and education and equivalent scores were included in the analyses. Social cognition was assessed with the Facial Emotion Identification Test (FEIT) [36], and the percentage of correct answers was included in the analyses.
The clinical assessment included an evaluation of the severity of psychopathological condition with the Clinical Global Impression Severity Scale (CGI-S) [37] and the Excited Component of the Positive and Negative Syndrome Scale (PANSS-EC) [38, 39].
Impulsivity was assessed through the administration of the Barratt Impulsiveness Scale (BIS-11) [40] and the Iowa Gambling Task (IGT) [41]; aggressiveness was assessed with the Modified Overt Aggression Scale (MOAS) [42], the risk of violent relapse with the Historical Clinical and Risk Management scale 20 (HCR-20) [43] and the level of psychopathy with the Hare Psychopathy Checklist (PCL-R) [44].
All subscales of the HCR-20 were included in the analyses. The PCL-R items were included in the analyses divided in two factors as defined by factor analysis conducted by the original scale authors: a factor describing the selfish, callous, and remorseless use of others (Factor 1 or “Callous”) and a factor describing chronically unstable and antisocial lifestyle or social deviance (Factor 2 or “Unstable”) [45]. Given their association with aggressive behavior and violent outcomes, these items were considered as more violence related [2].
All the assessments were carried out by trained physicians who were not involved in the usual care process of participants.
Statistical analyses
OP and non-OP groups were compared regarding all socio-demographic, clinical, cognitive, aggression, impulsivity, and risk of violent relapse parameters using Mann–Whitney U tests and χ2-tests for continuous and categorical variables, respectively. Only non-parametric analyses were used as all continuous variables had a non-normal distribution (all Shapiro–Wilk tests had p < 0.001). These univariate exploratory analyses were conducted to select potential predictors for the regression analyses [46].
Variables that emerged as significantly different in the univariate between-groups comparisons were introduced as potential predictors in multivariate binary logistic regression models conducted to separately identify socio-demographic and clinical, cognitive, and violence-related individual predictors of violent offence, allowing to assess which variables could explain the largest proportion of between-group variance. This approach was adopted considering the exploratory nature of the study to avoid using a single regression model in which strongly violence-related parameters would mask other significant variables, leading to type II errors. All regression analyses were conducted using a backward approach. Multicollinearity between individual predictors was assessed and was considered significant if the variance inflation factor (VIF) exceeded 4.0 [47]. As the number of potential predictors introduced in each regression model was lower than one for every ten observed subjects, which is recommended for logistic regressions according to conservative estimates [48, 49], the number of the included predictors was considered appropriate.
Post-hoc analyses were conducted to explore potential correlations between potential predictors’ variables in the whole sample using Spearman’s rho correlation test to better understand the relationships between different explored factors.
All analyses were conducted using the statistical software SPSS version 15.0 (SPSS Inc., Chicago, IL, USA, 2005); p values < 0.05 (two tailed) were considered significant.
Results
Sample characteristics and between-groups comparisons
The total sample, composed by 100 participants (50 OP and 50 non-OP) diagnosed with SSD was characterized by a mean age of 37.81 (± 11.06) years, the presence of 14 (14%) female subjects, and a mean education of 12.16 (± 2.88) years. As OP and non-OP were matched at recruitment regarding age, gender, and education, as well as diagnosis, no difference regarding these parameters could be observed.
A higher number of school failures, (p = 0.002), a higher prevalence of lifetime substance use (p = 0.024), and a more overall severe clinical condition (p = 0.002) and more severe excitatory symptoms (p < 0.001) were observed in OP (see Table 1).
OP showed a significantly worse performance in working memory domain as measured by the TMT-B test (p = 0.037) and in processing speed domain as measured by the Stroop test time (p = 0.026) and BACS Token Motor Task (p < 0.001); they also showed a better performance regarding attention domain as measured by Stroop Test errors (p < 0.001; for more details, see Table 2).
OP also showed higher scores in all HCL-20 subscales and PCL-R factor scores (all p < 0.001; for more details, see Table 3).
Predictors of violent offence
As regards the multivariate regression analyses, the number of school failures (p = 0.007) and the severity of excitatory symptoms (p < 0.001) emerged as socio-demographic and clinical individual predictors of belonging to the OP group (for more details, see Table 4).
Better attentive performance as measured by the Stroop Test errors (p = 0.003) and worse performance in speed of processing as measured by the Stroop Test time (p = 0.025) and BACS Token Motor test (p = 0.024) emerged as individual cognitive predictors (for more information, see Table 5).
Finally, the HCR-20 Risk Management subscale (p = 0.002) and the PCL-R “Callous” factor emerged as individual predictors in the last multivariate regression model (p = 0.031). This model explained the largest portion of between-group variance (Cox–Snell R2 = 0.692, Nagelkerke R2 = 0.923; for more details, see Table 6).
Post-hoc analyses
Post-hoc correlation analyses highlighted several significant correlations between cognitive and violence-related variables in the whole sample: of particular interest, better attentive performance in the Stroop Test errors is correlated with higher scores in all HCR subscales, in both PCL-R factors and negatively, as expected, with the BIS-11 Attention subscale, and worse performance in several cognitive domains is correlated with higher score in PCL-R “Unstable” factor (more details in Table 7).
Discussion
In the present study, 50 patients diagnosed with SSD and convicted for violent crimes and 50 non-offender participants matched for age, gender, education, and diagnosis were compared on a wide array of cognitive, clinical, impulsivity, aggression, and psychopathy characteristics. Predictors of belonging to the violent offenders participants subgroup were also assessed for each category of characteristics.
OP showed a larger prevalence of lifetime substance use: this finding was expected as substance use represents the most prominent predictor of violent behavior in people living with mental disorders [14, 16]. They also showed a higher number of school failures: this can, on one hand, be considered an indirect proxy of worse cognitive functioning, a factor that is better explained in the dedicated analyses; however, it can also be considered a marker of greater general adversity during childhood, including social and economic difficulties, a less supportive home environment, or the presence of undiagnosed neurodevelopmental disorders, such as attention deficit hyperactivity disorder (ADHD) or oppositional defiant disorder (ODD), which are correlated with both a higher number of school failures in childhood and to a higher risk of committing offences in in adulthood [50, 51]. Regarding clinical variables, offender participants showed higher CGI-S and PANSS-EC scores, corresponding to a more severe clinical condition; this finding is also in line with previous literature [2, 22].
As regards cognitive abilities, OP were characterized by an overall worse cognitive functioning, highlighted by a significantly worse performance in the working memory domain, as measured by the TMT-B, and a significantly worse performance in the processing speed domain, as measured by the BACS Token Motor Task and the Stroop Test time.
However, OP also showed a better attentive performance, as measured by the Stroop Test errors.
These results could be due to the high level of cognitive heterogeneity showed by people with SSD and violent behavior, as reported in the most recent and comprehensive systematic review and meta-analysis on this topic that highlighted a high level of heterogeneity both within and between studies [27]. Moreover, previous studies report that patients convicted in forensic settings could participate in cognitive tests with greater engagement, resulting in better scores when compared to controls [52].
However, it can also be hypothesized that patients with SSD convicted for violent crimes could show a peculiar cognitive profile, and that some patients with specific clinical correlates could show an overall better cognitive performance or a better performance in some specific domains. Concerning factors that are more closely correlated with violent outcomes, OP showed significantly higher scores in all HCL-20 subscales and all PCL-R factor, which represents an expected outcome.
A higher number of school failures and a higher score on the PANSS-EC emerged as socio-demographic and clinical predictors of belonging to the OP group. Worse performance at the Stroop Test time and worse performance at the BACS Token Motor Task, both measuring processing speed, and better Stroop error performance emerged as individual cognitive predictors. This result highlights the importance of this factor, pointing out that specific cognitive correlates might also predict important and distal outcomes such as violent behavior and suggesting that a thorough assessment of cognitive abilities is warranted in people with SSD, not only in the perspective of implementing specific treatments and to better personalize the rehabilitation program [53,54,55,56] but also, potentially, to increase the prevention of violent acts.
Higher scores on the HCR-20 Risk Management subscale and the PCL-R “Callous” factor also emerged as individual predictors of violent behavior, confirming the importance of using both instruments in the assessment of forensic patients.
Moreover, this regression model explained the largest portion of the variance. This was an expected result: on one hand, this finding remarks the importance of psychopathic and aggressive traits in determining violent behavior, but on the other, it confirms the need to design separate regression models when taking into account different categories of variables, including cognitive and socio-demographic characteristics, as potential predictors of violence.
Lastly, correlation analyses conducted in the whole sample show that a worse cognitive performance in several domains appears to be associated with a higher score in the PCL-R “Unstable” factor, whereas a better attentive performance is correlated, alongside a lower BIS-11 attentional impulsivity sub-scale score, with a higher score in PCL-R “Callous” factor. This represents a very interesting finding, suggesting that a better cognitive performance could identify patients who are more prone to callousness, manipulation and, perhaps, premeditating violent acts. On the contrary, cognitive deficits appear to identify those patients with more marked emotional instability, which could in turn be more prone to violent outbursts.
These results are particularly interesting because they could at least partly explain the heterogeneity reported in previous literature regarding cognitive characteristics of offenders diagnosed with SSD, highlighting a cognitive profile that is globally worse compared to non-offender patients but showing peculiarities that are worthy of further research.
Future studies should investigate whether it could be possible to identify distinct categories of patients on the basis of these characteristics: one characterized by callous aspects, with a globally less impaired cognitive profile and a better performance in some specific domains, and one characterized by aspects of impulsivity and instability with more prominent cognitive deficits.
Identifying characteristic profiles could have a positive impact not only to better characterize individual patients, but also in the development and implementation of personalized rehabilitation interventions. In fact, patients with more severe cognitive impairment could have consistent benefits from integrating pharmacological therapy and cognition-oriented treatments, including cognitive remediation and physical exercise [26, 35, 57,58,59], while other behavioral and pharmacological approaches could be more effective in other patients. Moreover, the feasibility and efficacy of a cognitive remediation intervention in a forensic setting have been already investigated in previous studies, showing promising results [60,61,62]. This could produce substantial benefits for the clinical condition as well as on functional outcomes of patients but also, at least partially, help in avoiding and preventing acts of violence.
Another interesting perspective for future studies could be to assess the impact of cognitive characteristics on different type of offenders diagnosed with SSD: better defining the cognitive correlates of early and late starters, which show several behavioral, clinical, and personality traits differences [63], could further improve the possibility to personalize treatment and prevention strategies.
This study presents a series of strengths. Patients were recruited in real-world setting and the sample can be considered quite representative of the population of individuals diagnosed with SSD and convicted in forensic settings. The assessment comprised a wide array of well-validated tools, considering also different test for several cognitive domain and including an evaluation of social cognition performance. Conducting separate analyses for different categories of variables and including sub-scales and factors of several assessment tools allowed to carefully evaluate a series of nuances in the participants’ cognitive, clinical, and behavioral profile.
The main limitation of the present study is represented by the small sample size, which did not allow to better identify and define categories of patients. Moreover, comparisons between hypothetical categories could not be performed, again for the small size of the sample: the fact that this could, at least in part, explain the observed heterogeneity and the between-variables correlations could represent an interesting perspective that has to be further explored in future studies. Another limitation is that overall SSD symptoms severity was only assessed with the PANSS-EC; a more comprehensive assessment using the full PANSS or, even better, using more recent and accurate tools for positive and negative symptoms severity assessment [64] could provide useful insight and should be considered in future studies.
In conclusion, the present study highlights the importance of carefully assessing people living with SSD with violent behavior in all clinical, cognitive, and behavioral aspects. In particular, assessing cognitive performance could provide interesting insights both in a research and in a clinical perspective. In fact, a careful assessment of all these variables could considerably help in the definition and implementation of personalized rehabilitation programs, which could be more effective both in improving patients’ clinical conditions and help in avoiding and preventing violent behaviors.
Data availability
The original contributions presented in the study are included in the article. Further inquiries are available upon reasonable request to the corresponding author.
References
Caruso R, Antenora F, Riba M et al (2021) Aggressive behavior and psychiatric inpatients: a narrative review of the literature with a focus on the European experience. Curr Psychiatry Rep 23:29. https://doi.org/10.1007/s11920-021-01233-z
Whiting D, Lichtenstein P, Fazel S (2021) Violence and mental disorders: a structured review of associations by individual diagnoses, risk factors, and risk assessment. Lancet Psychiatry 8:150–161. https://doi.org/10.1016/S2215-0366(20)30262-5
Brekke JS, Prindle C, Bae SW, Long JD (2001) Risks for individuals with schizophrenia who are living in the community. Psychiatr Serv Wash DC 52:1358–1366. https://doi.org/10.1176/appi.ps.52.10.1358
Fazel S, Sariaslan A (2021) Victimization in people with severe mental health problems: the need to improve research quality, risk stratification and preventive measures. World Psychiatry 20:437–438. https://doi.org/10.1002/wps.20908
Barlati S, Morena D, Nibbio G et al (2021) Internalized stigma among people with schizophrenia: Relationship with socio-demographic, clinical and medication-related features. Schizophr Res. https://doi.org/10.1016/j.schres.2021.06.007
Latalova K, Kamaradova D, Prasko J (2014) Violent victimization of adult patients with severe mental illness: a systematic review. Neuropsychiatr Dis Treat 10:1925–1939. https://doi.org/10.2147/NDT.S68321
Maniglio R (2009) Severe mental illness and criminal victimization: a systematic review. Acta Psychiatr Scand 119:180–191. https://doi.org/10.1111/j.1600-0447.2008.01300.x
Rossa-Roccor V, Schmid P, Steinert T (2020) Victimization of people with severe mental illness outside and within the mental health care system: results on prevalence and risk factors from a multicenter study. Front Psychiatry 11:932. https://doi.org/10.3389/fpsyt.2020.563860
Barlati S, Stefana A, Bartoli F et al (2019) Violence risk and mental disorders (VIORMED-2): a prospective multicenter study in Italy. PLoS ONE 14:e0214924. https://doi.org/10.1371/journal.pone.0214924
Iozzino L, Ferrari C, Large M et al (2015) Prevalence and risk factors of violence by psychiatric acute inpatients: a systematic review and meta-analysis. PLoS ONE 10:e0128536. https://doi.org/10.1371/journal.pone.0128536
Sariaslan A, Arseneault L, Larsson H et al (2020) Risk of subjection to violence and perpetration of violence in persons with psychiatric disorders in Sweden. JAMA Psychiat 77:359–367. https://doi.org/10.1001/jamapsychiatry.2019.4275
Fazel S, Gulati G, Linsell L et al (2009) Schizophrenia and violence: systematic review and meta-analysis. PLoS Med 6:e1000120. https://doi.org/10.1371/journal.pmed.1000120
Stevens H, Laursen TM, Mortensen PB et al (2015) Post-illness-onset risk of offending across the full spectrum of psychiatric disorders. Psychol Med 45:2447–2457. https://doi.org/10.1017/S0033291715000458
Duke AA, Smith KMZ, Oberleitner LMS et al (2018) Alcohol, drugs, and violence: a meta-meta-analysis. Psychol Violence 8:238–249. https://doi.org/10.1037/vio0000106
Van Dorn R, Volavka J, Johnson N (2012) Mental disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol 47:487–503. https://doi.org/10.1007/s00127-011-0356-x
Fazel S, Smith EN, Chang Z, Geddes JR (2018) Risk factors for interpersonal violence: an umbrella review of meta-analyses. Br J Psychiatry J Ment Sci 213:609–614. https://doi.org/10.1192/bjp.2018.145
Lamsma J, Cahn W, Fazel S, GROUP and NEDEN investigators (2020) Use of illicit substances and violent behaviour in psychotic disorders: two nationwide case-control studies and meta-analyses. Psychol Med 50:2028–2033. https://doi.org/10.1017/S0033291719002125
Bo S, Abu-Akel A, Kongerslev M et al (2011) Risk factors for violence among patients with schizophrenia. Clin Psychol Rev 31:711–726. https://doi.org/10.1016/j.cpr.2011.03.002
Fazel S, Wolf A, Larsson H et al (2017) Identification of low risk of violent crime in severe mental illness with a clinical prediction tool (Oxford Mental Illness and Violence tool [OxMIV]): a derivation and validation study. Lancet Psychiatry 4:461–468. https://doi.org/10.1016/S2215-0366(17)30109-8
Fleischman A, Werbeloff N, Yoffe R et al (2014) Schizophrenia and violent crime: a population-based study. Psychol Med 44:3051–3057. https://doi.org/10.1017/S0033291714000695
Jeyagurunathan A, Lau JH, Abdin E et al (2022) Aggression amongst outpatients with schizophrenia and related psychoses in a tertiary mental health institution. Front Psychiatry. https://doi.org/10.3389/fpsyt.2021.777388
Witt K, van Dorn R, Fazel S (2013) Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies. PLoS ONE 8:e55942. https://doi.org/10.1371/journal.pone.0055942
Galderisi S, Rossi A, Rocca P et al (2014) The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry 13:275–287. https://doi.org/10.1002/wps.20167
Green MF, Horan WP, Lee J (2019) Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry 18:146–161. https://doi.org/10.1002/wps.20624
Harvey PD, Strassnig M (2012) Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry 11:73–79. https://doi.org/10.1016/j.wpsyc.2012.05.004
Vita A, Gaebel W, Mucci A et al (2022) EPA Guidance on treatment of cognitive impairment in schizophrenia. Eur Psychiatry. https://doi.org/10.1192/j.eurpsy.2022.2315
Reinharth J, Reynolds G, Dill C, Serper M (2014) Cognitive predictors of violence in schizophrenia: a meta-analytic review. Schizophr Res Cogn 1:101–111. https://doi.org/10.1016/j.scog.2014.06.001
Ahmed AO, Richardson J, Buckner A et al (2018) Do cognitive deficits predict negative emotionality and aggression in schizophrenia? Psychiatry Res 259:350–357. https://doi.org/10.1016/j.psychres.2017.11.003
Rund BR (2018) A review of factors associated with severe violence in schizophrenia. Nord J Psychiatry 72:561–571. https://doi.org/10.1080/08039488.2018.1497199
Bulgari V, Iozzino L, Ferrari C et al (2017) Clinical and neuropsychological features of violence in schizophrenia: a prospective cohort study. Schizophr Res 181:124–130. https://doi.org/10.1016/j.schres.2016.10.016
Keefe RSE, Harvey PD (2012) Cognitive impairment in schizophrenia. Handb Exp Pharmacol. https://doi.org/10.1007/978-3-642-25758-2_2
Reitan RM (1958) Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills 8:271–276. https://doi.org/10.2466/pms.1958.8.3.271
Stroop JR (1938) Factors affecting speed in serial verbal reactions. Psychol Monogr 50:38–48. https://doi.org/10.1037/h0093516
Fusar-Poli P, Deste G, Smieskova R et al (2012) Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry 69:562–571. https://doi.org/10.1001/archgenpsychiatry.2011.1592
Vita A, Barlati S, Ceraso A et al (2021) Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiat 78:848–858. https://doi.org/10.1001/jamapsychiatry.2021.0620
Kerr SL, Neale JM (1993) Emotion perception in schizophrenia: specific deficit or further evidence of generalized poor performance? J Abnorm Psychol 102:312–318. https://doi.org/10.1037//0021-843x.102.2.312
Guy W (1976) ECDEU assessment manual for psychopharmacology. U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs
Kay SR, Fiszbein A, Opler LA (1987) The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276. https://doi.org/10.1093/schbul/13.2.261
Montoya A, Valladares A, Lizán L et al (2011) Validation of the Excited Component of the Positive and Negative Syndrome Scale (PANSS-EC) in a naturalistic sample of 278 patients with acute psychosis and agitation in a psychiatric emergency room. Health Qual Life Outcomes 9:18. https://doi.org/10.1186/1477-7525-9-18
Patton JH, Stanford MS, Barratt ES (1995) Factor structure of the Barratt impulsiveness scale. J Clin Psychol 51:768–774. https://doi.org/10.1002/1097-4679(199511)51:6%3c768::aid-jclp2270510607%3e3.0.co;2-1
Bechara A, Damasio AR, Damasio H, Anderson SW (1994) Insensitivity to future consequences following damage to human prefrontal cortex. Cognition 50:7–15. https://doi.org/10.1016/0010-0277(94)90018-3
Kay SR, Wolkenfeld F, Murrill LM (1988) Profiles of aggression among psychiatric patients: I. Nature and prevalence. J Nerv Ment Dis 176:539–546. https://doi.org/10.1097/00005053-198809000-00007
Douglas KS, Webster CD (1999) The HCR-20 violence risk assessment scheme: concurrent validity in a sample of incarcerated offenders. Crim Justice Behav 26:3–19. https://doi.org/10.1177/0093854899026001001
Hare RD (2003) The psychopathy checklist—revised manual. Tor Ont Can MHS
Hare RD (2020) The PCL-R assessment of psychopathy. The Wiley International handbook on psychopathic disorders and the law. John Wiley & Sons Ltd, pp 63–106
Heinze G, Wallisch C, Dunkler D (2018) Variable selection – a review and recommendations for the practicing statistician. Biom J Biom Z 60:431–449. https://doi.org/10.1002/bimj.201700067
Midi H, Sarkar SK, Rana S (2010) Collinearity diagnostics of binary logistic regression model. J Interdiscip Math 13:253–267. https://doi.org/10.1080/09720502.2010.10700699
Peduzzi P, Concato J, Kemper E et al (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379. https://doi.org/10.1016/s0895-4356(96)00236-3
Vittinghoff E, McCulloch CE (2007) Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 165:710–718. https://doi.org/10.1093/aje/kwk052
Erskine HE, Norman RE, Ferrari AJ et al (2016) Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 55:841–850. https://doi.org/10.1016/j.jaac.2016.06.016
Valsecchi P, Nibbio G, Rosa J et al (2021) Adult ADHD: prevalence and clinical correlates in a sample of Italian psychiatric outpatients. J Atten Disord 25:530–539. https://doi.org/10.1177/1087054718819824
Slotboom J, Hoppenbrouwers SS, Bouman YHA et al (2017) Visual attention in violent offenders: susceptibility to distraction. Psychiatry Res 251:281–286. https://doi.org/10.1016/j.psychres.2017.02.031
Maj M, van Os J, De Hert M et al (2021) The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry 20:4–33. https://doi.org/10.1002/wps.20809
Morin L, Franck N (2017) Rehabilitation interventions to promote recovery from schizophrenia: a systematic review. Front Psychiatry. https://doi.org/10.3389/fpsyt.2017.00100
Nibbio G, Barlati S, Cacciani P et al (2020) Evidence-based integrated intervention in patients with schizophrenia: a pilot study of feasibility and effectiveness in a real-world rehabilitation setting. Int J Environ Res Public Health 17:E3352. https://doi.org/10.3390/ijerph17103352
Vita A, Barlati S, Ceraso A et al (2022) Acceptability of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized controlled trials. Psychol Med. https://doi.org/10.1017/S0033291722000319
Firth J, Stubbs B, Rosenbaum S et al (2017) Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull 43:546–556. https://doi.org/10.1093/schbul/sbw115
Stubbs B, Vancampfort D, Hallgren M et al (2018) EPA guidance on physical activity as a treatment for severe mental illness: a meta-review of the evidence and Position Statement from the European Psychiatric Association (EPA), supported by the International Organization of Physical Therapists in Mental Health (IOPTMH). Eur Psychiatry J Assoc Eur Psychiatr 54:124–144. https://doi.org/10.1016/j.eurpsy.2018.07.004
Vita A, De Peri L, Barlati S et al (2011) Psychopathologic, neuropsychological and functional outcome measures during cognitive rehabilitation in schizophrenia: A prospective controlled study in a real-world setting. Eur Psychiatry 26:276–283. https://doi.org/10.1016/j.eurpsy.2010.03.008
Ahmed AO, Hunter KM, Goodrum NM et al (2015) A randomized study of cognitive remediation for forensic and mental health patients with schizophrenia. J Psychiatr Res 68:8–18. https://doi.org/10.1016/j.jpsychires.2015.05.013
O’Reilly K, Donohoe G, O’Sullivan D et al (2019) A randomized controlled trial of cognitive remediation for a national cohort of forensic patients with schizophrenia or schizoaffective disorder. BMC Psychiatry 19:27. https://doi.org/10.1186/s12888-019-2018-6
Thomas ML, Bismark AW, Joshi YB et al (2018) Targeted cognitive training improves auditory and verbal outcomes among treatment refractory schizophrenia patients mandated to residential care. Schizophr Res 202:378–384. https://doi.org/10.1016/j.schres.2018.07.025
Tengström A, Hodgins S, Kullgren G (2001) Men with schizophrenia who behave violently: the usefulness of an early- versus late-start offender typology. Schizophr Bull 27:205–218. https://doi.org/10.1093/oxfordjournals.schbul.a006867
Galderisi S, Mucci A, Dollfus S et al (2021) EPA guidance on assessment of negative symptoms in schizophrenia. Eur Psychiatry 64:e23. https://doi.org/10.1192/j.eurpsy.2021.11
Acknowledgements
All authors who contributed to this paper are listed as authors. No professional medical writer was involved in any portion of the preparation of the manuscript.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in the design, execution, interpretation, or writing of the study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barlati, S., Nibbio, G., Stanga, V. et al. Cognitive and clinical characteristics of offenders and non-offenders diagnosed with schizophrenia spectrum disorders: results of the Recoviwel observational study. Eur Arch Psychiatry Clin Neurosci 273, 1307–1316 (2023). https://doi.org/10.1007/s00406-022-01510-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-022-01510-9