Abstract
Impaired perceptual inference has been suggested to be at the core of positive symptoms in schizophrenia. Apparent motion (AM) is a visual illusion in which perceptual inference gives rise to the experience of a single object moving back and forth when two spatially separated objects are flashed in alternation. Here, we investigated the strength of AM perception in patients with paranoid schizophrenia. Patients were less susceptible to the illusion as indicated by a lower probability of motion perception at the individual’s optimal presentation frequency for AM. In addition, the probability of AM perception was inversely related to delusional conviction in the patient group. These results suggest that schizophrenia may be associated with a reduced susceptibility to visual phenomena that commonly rely on perceptual inference.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is substantial agreement that our perception is shaped by contextual information and stored patterns of previous sensory experiences [1–6]. A failure in such a perceptual inference mechanism has been suggested to be at the core of positive symptoms in schizophrenia [7–9]. According to these theories, patients rely more on bottom-up, stimulus-driven information rather than on top-down, conceptually driven strategies [10, 11]. As a result, sensory inputs that would otherwise be effortlessly interpreted by the brain are pieced together without reference to an expected model [12, 13]. While this altered mechanism may promote creative interpretations that are driven by data rather than theory, the attempt to cope with unusual perceptual experiences resulting from such impaired perceptual inference is thought to give rise to delusional explanations.
A striking example of how top-down expectations influence our perception is that of apparent motion (AM) [14]. In AM, the problem posed by the rapid alternating appearance and disappearance of two stationary stimuli separated by some distance is normally interpreted by the brain as one single moving object [15]. The subjective perception of AM depends on the presentation frequency of the stationary stimuli, with the percept changing from sequential alternation to smooth movement (AM) and finally to two simultaneous flickering dots as the alternation rate of the stimuli increases [16]. In the optimal frequency range, the illusion of motion is thought to occur through a top-down inferential process, which makes the sequential appearance of the two blinking dots appear as smooth displacement.
It is the disparity between stimulus configuration and perception that makes the AM phenomenon suitable to investigations of perceptual inference accounts of delusions. Here, we adopted the method of constant stimuli [17], a method in which different levels of a certain property of the stimulus are presented randomly, to assess the individual’s optimal presentation frequency for AM perception, and compared the strength of the illusion (i.e., the probability of reporting a motion percept at the optimal presentation frequency) between groups. Our hypothesis was that impaired perceptual inference in patients with schizophrenia would be reflected by a reduced strength of AM perception and that this impairment would be related to the degree of delusional psychopathology. Because altered perceptual inference has been proposed as a key mechanism specifically for the formation of delusions [7], we focused on the paranoid subtype of schizophrenia in the present study.
Method
Participants
Thirty-four patients who fulfilled the International Classification of Disease (ICD-10, World Health Organization) criteria for paranoid schizophrenia were recruited at the Charité University Hospital, Campus Charité Mitte. Except for three unmedicated patients, all were on stable doses of atypical antipsychotic medication. The chlorpromazine-equivalent doses of medications and clinical characteristics of these patients are summarized in Table 1. Thirty-four healthy subjects matched for age and gender served as controls. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) was used to rule out current or past psychiatric disorders in the control group. We used the Positive and Negative Syndrome Scale (PANSS) [18] for quantitative assessment of symptom severity in schizophrenia patients. Furthermore, we obtained a measure of delusional ideation in both groups using the Peters Delusion Inventory (PDI) [19], a 21-item self-report questionnaire specifically designed to quantify delusional ideation. Each item is answered with yes or no, and, if endorsed, three subscales are rated: distress, preoccupation, and conviction (subscale scores range from 1 to 5). A total score is computed by summing all items. Higher scores reflect greater delusion-proneness. The PDI provides a more specific assessment of delusional experiences than the PANSS (an instrument in which delusions are quantified in only one of the 7 items of the positive scale). Participants also underwent the d2 test of attention [20] and the Edinburgh handedness inventory to assess hand preference [21]. Except for six patients and three healthy control subjects, all participants completed the German vocabulary test to measure verbal IQ [22] (see Table 1). All subjects had normal or corrected-to-normal vision. Exclusion criteria for both groups were benzodiazepine intake within 15 h before the experiment, illicit substance use in the 3 days prior to the test, and neurological comorbid diagnoses. All participants gave written informed consent before participation in the study, which was approved by an accredited Medical Ethics Review Committee (METC). Subjects received credit points or financial compensation for their participation. Thirty-one patients and thirty-one healthy subjects that took part in this experiment also participated in a related study that we reported in a separate paper [23].
Stimuli
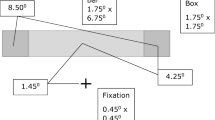
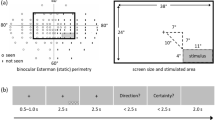
The stimuli were generated using MATLAB software (version 2009a, http://www.mathworks.com/) and Cogent2000 toolbox (http://www.vislab.ucl.ac.uk/cogent.php) and presented on a CRT computer monitor (1,024 × 768 resolution, 75-Hz refresh rate, gray background). A white fixation cross (1.2 × 1.2 degrees of visual angle) was always displayed at the center. The stimuli consisted of white squares (2.35° × 2.35°) flashed 7.72° to the right of the fixation cross at two fixed positions with a vertical separation of 16.45°. The squares alternated between the two positions at ten different presentation frequencies. Each stimulus was presented for 333.3, 240.0, 186.7, 146.7, 106.7, 80.0, 66.7, 53.3, 40.0, or 26.7 ms, with an inter-stimulus interval (ISI) of the same duration, resulting in a presentation frequency of 0.75, 1.04, 1.34, 1.7, 2.34, 3.12, 3.75, 4.69, 6.25, or 9.37 Hz, respectively. Depending on the presentation frequency, these stimuli yielded the perception of either sequential alternation between the two stimulus locations, of a square moving up and down (AM), or of two simultaneously flickering squares.
Procedure
Participants were seated in front of the screen in a darkened room (48 cm viewing distance) and were asked to fixate the fixation cross throughout the entire duration of the experiment. Eye movements were recorded using a remote video eye-tracking system to control for fixation (Cambridge research System, 250-Hz sampling rate). At the beginning of each trial, the fixation cross was displayed alone for 0.2 s, and then AM stimuli were presented for 2.5 s. Subjects were asked to report whether they perceived the square as moving smoothly back and forth (“motion”) or not (“sequential alternation” or “flicker”) by pressing specified keys on the keyboard. Each presentation frequency was presented 20 times in a randomized order. The probability of reporting a motion percept, that is, the proportion of “motion” responses, was determined for each presentation frequency. The optimal presentation frequency was defined as the presentation frequency that yielded the highest proportion of “motion” responses or, in case of two or more frequencies yielding the maximum probability of AM perception, as the average between these frequencies. The strength of AM percept was defined as the probability of reporting a motion percept at the individual optimal presentation frequency. We calculated eye gaze fixation rates as the percentage of time in which the participant fixated his/her gaze within the region corresponding to a circle of 2° radius on the center of the screen.
Statistics
Sample characteristics and gaze fixation rates were compared by means of independent samples t-tests (for continuous variables) and χ2 test (for the categorical variable gender). We used repeated-measures analyses of variance (ANOVA) and independent samples t test to assess group differences in AM perception. In the presence of group differences, we performed additional correlation analyses on the variables that differed significantly between groups (see “Results”). As these additional analyses were exploratory in nature, no correction for multiple testing was applied. Where appropriate, degrees of freedom were corrected using Greenhouse-Geisser estimates of sphericity. All analyses were conducted using the software SPSS 17.0 (Statistical Package for Social Sciences, http://www-01.ibm.com/software/analytics/spss/).
Results
Sample characteristics
The groups did not differ significantly in gender, handedness, and age (see Table 1). Patients had a slightly lower mean verbal IQ than healthy control subjects, but did not differ in years of education, indicating equivalent levels of premorbid IQ. As expected, PDI scores were significantly higher in the patient group, reflecting the high level of delusional ideation in schizophrenia patients.
Gaze fixation
Fixation rates, i.e., the percentage of eye positions inside a circle of 2° radius on the center of the screen, did not differ between groups (patients: μ = 84.4 %, SD = 28.3; controls: 84.4 %, SD = 29.2; t = −0.002, n.s.).
AM perception
First, we tested whether AM perception differed between groups across all presentation frequencies (see Fig. 1a). A two-way ANOVA with the factors group and presentation frequency revealed a main effect of frequency (F(9,594) = 19.4, p ≤ 0.001, η² = 0.227), but no main effect of group (F(1,66) = 1.9, p = 0.176, η² = 0.028) nor group x presentation frequency interaction (F(9,594) = 1.6, p = 0.19, η² = 0.024). Since inter-individual variability relating to optimal presentation frequency for AM may hamper the sensitivity of such an analysis, we subsequently analyzed the strength of AM perception at each individual’s optimal presentation frequency. Importantly, the identification of the optimal presentation frequency in each individual is independent of the comparison of group means and does not impose any systematic bias on the analysis. While healthy control participants reported AM perception in the majority of trials at their optimal presentation frequency, the corresponding proportion of trials with reported AM perception was substantially lower in patients with paranoid schizophrenia (t = −2.841 p = 0.006, two-tailed t test, see Fig. 1b). This indicates that the illusion was less compelling in the patient group. Finally, we examined the individual optimal presentation frequency for AM perception. There was no significant difference in the optimal presentation frequency for AM perception between groups (patients: μ = 2.88, SD = 1.75; controls: μ = 3.6, SD = 2.04; t = −1.572, p = 0.121). In other words, we did not find any evidence for between-group differences in the relationship between presentation frequency and susceptibility to the AM illusion.
a Group psychometric curves: % AM perception as a function of presentation frequency, b AM percept strength (%) in each group, c correlation between PDI conviction score and AM percept strength (%) in the patient group. Error bars indicate ±1 Standard error of the mean, the asterisk indicate p < 0.01
Correlational analyses
To explore the relationship between psychopathology and AM perception, we tested for correlations of clinical symptoms with the strength of the AM percept at each individual’s optimal frequency in the patient group. PANSS was used as a measure of general, positive, and negative symptom severity, and PDI more specifically assessed delusional ideation. There was no significant correlation of PANSS subscores or total score, or of the total PDI score with the strength of AM percept. Interestingly, however, AM percept strength was negatively correlated with PDI conviction subscale (r = −0.382, p = 0.028, see Fig. 1c), suggesting that the strength of the illusion decreases as delusional belief conviction increases in the patient group. To rule out unspecific effects of intelligence, attention problems, and medication, we also tested for correlations of the AM percept strength with the WST-IQ score, the d2-test composite index, and chlorpromazine-equivalents, respectively. No significant correlations were found (all p > 0.1).
Discussion
The aim of this study was to investigate perceptual inference in patients with paranoid schizophrenia. We assessed patient’s susceptibility to AM, a visual illusion that is thought to arise from the inferential nature of perception. Our results reveal a reduced probability of AM perception at the individual’s optimal presentation frequency in patients with schizophrenia and reflect a weakened susceptibility to the illusion. In accordance with our hypothesis, the strength of the AM percept was inversely related to the PDI conviction score in the patient group, suggesting that delusional belief conviction increases with poorer perceptual inference.
Patients were less prone to integrate the rapid alternating appearance and disappearance of two AM stimuli into the percept of one single moving object. This is in line with previous reports of misinterpretation of percepts in risk of schizophrenia-spectrum disorders [24] and impaired perceptual organization in schizophrenia [25–28]. Patients have been shown to be less susceptible to forms of visual contextual modulation, whereby the perception of a center stimulus is influenced by the presence of a surround [27, 29, 30], as well as to the hollow-mask illusion, a phenomenon in which the percept of an implausible inverted face is replaced by that of a coherent visual object [10, 31]. While these previous findings are in line with our current data in that they show a reduced susceptibility of schizophrenia patients to perceptual illusions, investigations of the Müller-Lyer illusion, another example of context-induced misperception, have yielded mixed results. Some studies showed decreased susceptibility to this illusion [32–34], whereas others found either no alteration or even increased susceptibility [32, 35], possibly due to the heterogeneity of patient samples included in these studies [36]. Overall, our findings extend previous evidence for altered contextual modulation and object processing in schizophrenia. Together, the evidence suggests a reduced ability to apply top-down processing in order to interpret sensory stimuli and may imply a general alteration of perceptual inference in schizophrenia.
Consistent with an early investigation of AM perception in patients with paranoid schizophrenia [37], we did not find a difference in the optimal frequency range for AM perception between groups. The lack of group difference in the optimal stimulation parameters for the illusion places our finding of weaker AM perception in paranoid schizophrenia at the level of perceptual judgment. That patients were less likely to perceive AM stimuli as moving supports the argument that delusions are related to an increased confidence in actual perceptual inputs and a weakening of top-down inference (for a review of Bayesian concepts of psychosis, see Corlett et al. [38]). The correlation between the strength of the illusion and the conviction score of the PDI scale that we found in the patient group corroborates this interpretation. Using an objective target detection task, we have recently demonstrated that patients with paranoid schizophrenia are able to predict the spatiotemporal position of visual events along the illusory AM trace [23]. In light of this previous finding, patients’ reduced subjective AM perception indicates a failure to integrate top-down predictions into a compelling motion percept.
Nevertheless, early investigations of AM perception in schizophrenia reported a lower threshold for the breakdown of AM (i.e., the presentation frequency at which subjects stop perceiving motion) in patients with acute, chronic, and undifferentiated schizophrenia [37, 39, 40]. These reports point to a different stimulation frequency range for AM perception in other schizophrenia subtypes. Taking into account the changes in the diagnostic criteria that have taken place since the aforementioned studies, it would be interesting to investigate the frequency range as well as the strength of this illusion in other schizophrenia subtypes.
One shortcoming of this study is that the majority of patients were medicated at the time of testing. Saucer et al. [41] have shown that antipsychotic treatment raises the threshold for AM breakdown. Hence, medication may have masked group differences in the optimal presentation frequency for AM perception in our study. Although we cannot rule out the possibility that drug treatment contributed to the observed decrease in patients’ susceptibility to AM, the results of the study by Saucer et al. (1959) suggest that an effect of medication would have improved AM perception in the patient group. Thus, if anything, we would expect group differences between unmedicated patients and controls to be larger than those observed in this study. Furthermore, since we found no correlation between maximum AM percept and chlorpromazine-equivalent doses in our sample, it is unlikely that medication could underlie our results. People with schizophrenia have been shown to be more resistant to a visual illusion triggered by an attentional cue [42]. While we do not directly address whether deficient motion perception in the patient group reflects a more general stimulus classification/target detection deficit [43], our attention measure (d2 test scores) infers that the reduced strength of AM perception in patients cannot be easily attributed to general attention deficits. No correlation was observed between attention scores and a patients’ probability of reporting a motion percept at their individual optimal presentation frequency.
Although we cannot make any strong conclusions regarding neural mechanisms on the basis of our behavioral findings, it seems likely that patients’ decreased susceptibility to AM results either from a dysfunction in early visual inputs or in the recurrent processing between the human motion complex (hMT/V5) and the primary visual cortex (V1), the two visual areas that have been implicated in AM perception [44–46]. In fact, motion-processing deficits in schizophrenia [47–50] have previously been related to suboptimal neural processing of motion signals [51]. Notwithstanding, it has been demonstrated that conscious perception is associated with an increase in activity not only at the sensory level, but also within the fronto-parietal network [52]. Of interest, Lencer et. al. have recently reported altered transfer of visual motion information to parietal association cortex in untreated patients suffering their first-episode psychosis [53]. Therefore, one could also speculate that reduced subjective AM perception in patients with paranoid schizophrenia might result from inefficient interactions between fronto-parietal regions and lower-order visual areas. This account would be in agreement with previous reports of widespread cortical deficit [54], abnormal integration of functional brain networks [55–64], and decreased influence from the fronto-parietal areas on visual perception in patients with schizophrenia [65–68].
Conclusion
In conclusion, our data indicate that patients with paranoid schizophrenia are less susceptible to AM and that the probability of perceiving the illusion decreases with increasing delusional belief conviction. These results suggest that schizophrenia may be associated with a reduced susceptibility to visual phenomena that commonly rely on perceptual inference.
References
Rao RP, Ballard DH (1999) Predictive coding in the visual cortex: a functional interpretation of some extra-classical receptive-field effects. Nat Neurosci 2(1):79–87. doi:10.1038/4580
Hedges JH, Stocker AA, Simoncelli EP (2011) Optimal inference explains the perceptual coherence of visual motion stimuli. J Vis 11(6). doi:10.1167/11.6.14
Friston K, Kilner J, Harrison L (2006) A free energy principle for the brain. J Physiol Paris 100(1–3):70–87. doi:10.1016/j.jphysparis.2006.10.001
Gregory RL (1997) Knowledge in perception and illusion. Philos T R Soc B 352(1358):1121–1127
Yellott JI (1981) Binocular depth inversion. Sci Am 245(1):148
George D, Hawkins J (2009) Towards a mathematical theory of cortical micro-circuits. PLoS Comput Biol 5(10):e1000532. doi:10.1371/journal.pcbi.1000532
Fletcher PC, Frith CD (2009) Perceiving is believing: a Bayesian approach to explaining the positive symptoms of schizophrenia. Nat Rev Neurosci 10(1):48–58. doi:10.1038/nrn2536
Hemsley DR (1992) Cognitive abnormalities and schizophrenic symptoms. Psychol Med 22(4):839–842
Garety PA, Hemsley DR, Wessely S (1991) Reasoning in deluded schizophrenic and paranoid patients. Biases in performance on a probabilistic inference task. J Nerv Ment Dis 179(4):194–201
Emrich HM, Leweke FM, Schneider U (1997) Towards a cannabinoid hypothesis of schizophrenia: cognitive impairments due to dysregulation of the endogenous cannabinoid system. Pharmacol Biochem Be 56(4):803–807
Gilbert CD, Sigman M (2007) Brain states: top-down influences in sensory processing. Neuron 54(5):677–696. doi:10.1016/j.neuron.2007.05.019
Hemsley DR (1994) A cognitive model for schizophrenia and its possible neural basis. Acta Psychiatry Scand Suppl 384:80–86
Hemsley DR (2005) The development of a cognitive model of schizophrenia: placing it in context. Neurosci Biobehav Rev 29(6):977–988. doi:10.1016/j.neubiorev.2004.12.008
Tse PU, Cavanagh P (2000) Chinese and Americans see opposite apparent motions in a Chinese character. Cognition 74(3):B27–32
Sigman E, Rock I (1974) Stroboscopic movement based on perceptual intelligence. Perception 3(1):9–28
Wertheimer M (1912) Experimental studies on seeing of movement. Z Psychol Physiol Si 61:161–265
Simpson WA (1988) The method of constant stimuli is efficient. Percept Psychophys 44(5):433–436
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13(2):261–276
Peters E, Joseph S, Day S, Garety P (2004) Measuring delusional ideation: the 21-item Peters et al. delusions inventory (PDI). Schizophr Bull 30(4):1005–1022
Bates ME, Lemay EP Jr (2004) The d2 Test of attention: construct validity and extensions in scoring techniques. J Int Neuropsychol Soc 10(3):392–400. doi:10.1017/S135561770410307X
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9(1):97–113
Stephan P (1995) Description of the Wortschatztest. Diagnostica 41(3):297–301
Sanders LL, Muckli L, de Millas W, Lautenschlager M, Heinz A, Kathmann N, Sterzer P (2012) Detection of visual events along the apparent motion trace in patients with paranoid schizophrenia. Psychiatry Res. doi:10.1016/j.psychres.2012.03.006
Hoffman RE, Woods SW, Hawkins KA, Pittman B, Tohen M, Preda A, Breier A, Glist J, Addington J, Perkins DO, McGlashan TH (2007) Extracting spurious messages from noise and risk of schizophrenia-spectrum disorders in a prodromal population. Br J Psychiatry 191:355–356. doi:10.1192/bjp.bp.106.031195
Uhlhaas PJ, Phillips WA, Mitchell G, Silverstein SM (2006) Perceptual grouping in disorganized schizophrenia. Psychiatry Res 145(2–3):105–117. doi:10.1016/j.psychres.2005.10.016
Silverstein SM, Kovacs I, Corry R, Valone C (2000) Perceptual organization, the disorganization syndrome, and context processing in chronic schizophrenia. Schizophr Res 43(1):11–20
Horton HK, Silverstein SM (2011) Visual context processing deficits in schizophrenia: effects of deafness and disorganization. Schizophr Bull 37(4):716–726. doi:10.1093/schbul/sbr055
Silverstein SM, Keane BP (2011) Perceptual organization impairment in schizophrenia and associated brain mechanisms: review of research from 2005 to 2010. Schizophr Bull 37(4):690–699. doi:10.1093/schbul/sbr052
Dakin S, Carlin P, Hemsley D (2005) Weak suppression of visual context in chronic schizophrenia. Curr Biol 15(20):R822–824. doi:10.1016/j.cub.2005.10.015
Yoon JH, Rokem AS, Silver MA, Minzenberg MJ, Ursu S, Ragland JD, Carter CS (2009) Diminished orientation-specific surround suppression of visual processing in schizophrenia. Schizophr Bull 35(6):1078–1084. doi:10.1093/schbul/sbp064
Schneider U, Borsutzky M, Seifert J, Leweke FM, Huber TJ, Rollnik JD, Emrich HM (2002) Reduced binocular depth inversion in schizophrenic patients. Schizophr Res 53(1–2):101–108
Parnas J, Vianin P, Saebye D, Jansson L, Volmer-Larsen A, Bovet P (2001) Visual binding abilities in the initial and advanced stages of schizophrenia. Acta Psychiatry Scand 103(3):171–180
Letourneau JE (1974) The Oppel-Kundt and the Muller-Lyer illusions among schizophrenics. Percept Mot Skills 39(2):775–778
Weckowicz TE, Witney G (1960) The Muller-Lyer illusion in schizophrenic patients. J Ment Sci 106:1002–1007
Tam WC, Sewell KW, Deng HC (1998) Information processing in schizophrenia and bipolar disorder: a discriminant analysis. J Nerv Ment Dis 186(10):597–603
Pessoa VF, Monge-Fuentes V, Simon CY, Suganuma E, Tavares MC (2008) The Muller-Lyer illusion as a tool for schizophrenia screening. Rev Neurosci 19(2–3):91–100
Saucer RT (1958) A further study of the perception of apparent motion by schizophrenics. J Consult Psychol 22(4):256–258
Corlett PR, Taylor JR, Wang XJ, Fletcher PC, Krystal JH (2010) Toward a neurobiology of delusions. Prog Neurobiol 92(3):345–369
Deabler HL, Saucer RT (1956) Perception of apparent motion in organics and schizophrenics. J Consult Psychol 20(5):385–389
Chambers JL, Wilson WT (1968) Perception of apparent motion and degree of mental pathology. Percept Mot Skills 26(3):855–861
Saucer RT (1959) Chlorpromazine and apparent motion perception by schizophrenics. J Consult Psychol 23(2):134–136
Crawford TJ, Hamm JP, Kean M, Schmechtig A, Kumari V, Anilkumar AP, Ettinger U (2010) The perception of real and illusory motion in schizophrenia. Neuropsychologia 48(10):3121–3127. doi:10.1016/j.neuropsychologia.2010.06.027
Wang J, Brown R, Dobkins KR, McDowell JE, Clementz BA (2010) Diminished parietal cortex activity associated with poor motion direction discrimination performance in schizophrenia. Cereb Cortex 20(7):1749–1755. doi:10.1093/cercor/bhp243
Ahmed B, Hanazawa A, Undeman C, Eriksson D, Valentiniene S, Roland PE (2008) Cortical dynamics subserving visual apparent motion. Cereb Cortex 18(12):2796–2810. doi:10.1093/cercor/bhn038
Sterzer P, Haynes JD, Rees G (2006) Primary visual cortex activation on the path of apparent motion is mediated by feedback from hMT+/V5. Neuroimage 32(3):1308–1316. doi:10.1016/j.neuroimage.2006.05.029
Wibral M, Bledowski C, Kohler A, Singer W, Muckli L (2009) The timing of feedback to early visual cortex in the perception of long-range apparent motion. Cereb Cortex 19(7):1567–1582. doi:10.1093/cercor/bhn192
Chen Y, Nakayama K, Levy D, Matthysse S, Holzman P (2003) Processing of global, but not local, motion direction is deficient in schizophrenia. Schizophr Res 61(2–3):215–227
Kim J, Park S, Blake R (2011) Perception of biological motion in schizophrenia and healthy individuals: a behavioral and FMRI study. PLoS One 6(5):e19971. doi:10.1371/journal.pone.0019971
Chen Y, Palafox GP, Nakayama K, Levy DL, Matthysse S, Holzman PS (1999) Motion perception in schizophrenia. Arch Gen Psychiatry 56(2):149–154
Chen Y, Levy DL, Sheremata S, Holzman PS (2004) Compromised late-stage motion processing in schizophrenia. Biol Psychiatry 55(8):834–841. doi:10.1016/j.biopsych.2003.12.024
Chen Y, Grossman ED, Bidwell LC, Yurgelun-Todd D, Gruber SA, Levy DL, Nakayama K, Holzman PS (2008) Differential activation patterns of occipital and prefrontal cortices during motion processing: evidence from normal and schizophrenic brains. Cogn Affect Behav Neurosci 8(3):293–303
Rees G (2007) Neural correlates of the contents of visual awareness in humans. Philos Trans R Soc Lond B Biol Sci 362(1481):877–886. doi:10.1098/rstb.2007.2094
Lencer R, Keedy SK, Reilly JL, McDonough BE, Harris MS, Sprenger A, Sweeney JA (2011) Altered transfer of visual motion information to parietal association cortex in untreated first-episode psychosis: implications for pursuit eye tracking. Psychiatry Res 194(1):30–38. doi:10.1016/j.pscychresns.2011.06.011
Molina V, Galindo G, Cortes B, de Herrera AG, Ledo A, Sanz J, Montes C, Hernandez-Tamames JA (2011) Different gray matter patterns in chronic schizophrenia and chronic bipolar disorder patients identified using voxel-based morphometry. Eur Arch Psychiatry Clin Neurosci 261(5):313–322. doi:10.1007/s00406-010-0183-1
Bassett DS, Bullmore E, Verchinski BA, Mattay VS, Weinberger DR, Meyer-Lindenberg A (2008) Hierarchical organization of human cortical networks in health and schizophrenia. J Neurosci 28(37):9239–9248. doi:10.1523/JNEUROSCI.1929-08.2008
Micheloyannis S, Pachou E, Stam CJ, Breakspear M, Bitsios P, Vourkas M, Erimaki S, Zervakis M (2006) Small-world networks and disturbed functional connectivity in schizophrenia. Schizophr Res 87(1–3):60–66. doi:10.1016/j.schres.2006.06.028
Rubinov M, Knock SA, Stam CJ, Micheloyannis S, Harris AW, Williams LM, Breakspear M (2009) Small-world properties of nonlinear brain activity in schizophrenia. Hum Brain Mapp 30(2):403–416. doi:10.1002/hbm.20517
Liu Y, Liang M, Zhou Y, He Y, Hao Y, Song M, Yu C, Liu H, Liu Z, Jiang T (2008) Disrupted small-world networks in schizophrenia. Brain 131(Pt 4):945–961. doi:10.1093/brain/awn018
Friston KJ (1998) The disconnection hypothesis. Schizophr Res 30(2):115–125
Stephan KE, Friston KJ, Frith CD (2009) Dysconnection in schizophrenia: from abnormal synaptic plasticity to failures of self-monitoring. Schizophr Bull 35(3):509–527. doi:10.1093/schbul/sbn176
Stephan KE, Baldeweg T, Friston KJ (2006) Synaptic plasticity and dysconnection in schizophrenia. Biol Psychiatry 59(10):929–939. doi:10.1016/j.biopsych.2005.10.005
Uhlhaas PJ, Singer W (2010) Abnormal neural oscillations and synchrony in schizophrenia. Nat Rev Neurosci 11(2):100–113. doi:10.1038/nrn2774
Deserno L, Sterzer P, Wustenberg T, Heinz A, Schlagenhauf F (2012) Reduced prefrontal-parietal effective connectivity and working memory deficits in schizophrenia. J Neurosci 32(1):12–20. doi:10.1523/JNEUROSCI.3405-11.2012
Volpe U, Federspiel A, Mucci A, Dierks T, Frank A, Wahlund LO, Galderisi S, Maj M (2008) Cerebral connectivity and psychotic personality traits. A diffusion tensor imaging study. Eur Arch Psychiatry Clin Neurosci 258(5):292–299. doi:10.1007/s00406-007-0796-1
Dima D, Dietrich DE, Dillo W, Emrich HM (2010) Impaired top-down processes in schizophrenia: a DCM study of ERPs. Neuroimage 52(3):824–832. doi:10.1016/j.neuroimage.2009.12.086
Dima D, Dillo W, Bonnemann C, Emrich HM, Dietrich DE (2011) Reduced P300 and P600 amplitude in the hollow-mask illusion in patients with schizophrenia. Psychiatry Res. doi:10.1016/j.pscychresns.2010.09.015
Dima D, Roiser JP, Dietrich DE, Bonnemann C, Lanfermann H, Emrich HM, Dillo W (2009) Understanding why patients with schizophrenia do not perceive the hollow-mask illusion using dynamic causal modelling. Neuroimage 46(4):1180–1186. doi:10.1016/j.neuroimage.2009.03.033
Peled A, Pressman A, Geva AB, Modai I (2003) Somatosensory evoked potentials during a rubber-hand illusion in schizophrenia. Schizophr Res 64(2–3):157–163. doi:10.1016/S0920-9964(03)00057-4
Acknowledgments
Funding for this study was provided by the German Research Foundation (DFG) Emmy-Noether-Program STE-1430/2-1 and Excellency Initiative DFG Grant GSC86/1-2009.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanders, L.L.O., de Millas, W., Heinz, A. et al. Apparent motion perception in patients with paranoid schizophrenia. Eur Arch Psychiatry Clin Neurosci 263, 233–239 (2013). https://doi.org/10.1007/s00406-012-0344-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-012-0344-5