Abstract
Purpose
Sialendoscopy is a new, minimally invasive method that is becoming increasingly more popular than traditional methods for the treatment of sialolithiasis. In this systematic review and meta-analysis, the effectiveness and safety of this method in children with sialolithiasis are investigated.
Methods
Inclusion criteria were children with sialolithiasis. The information sources were databases MEDLINE and PubMed Central (through PubMed), ScienceDirect, Cochrane Central Register of Controlled Trials (CENTRAL), citation indexes Scopus and Google Scholar, trial registries, and “gray literature”. The last search was performed on September 18, 2022. The risk of bias in included studies was assessed using ROBINS-I tool (Risk Of Bias In Non-randomized Studies of Interventions). The pooled proportion of weighted means was calculated for the quantitative synthesis of available data.
Results
The effectiveness of the method was estimated at 95.5% (95% CI 89.8–99.3%), from 13 studies including 133 cases. The safety was estimated at 97.2% (95% CI 91.8–100%), from 10 studies including 113 cases.
Conclusion
The limitations of this study, briefly summarized, are the small number of included studies, the fact that they are mostly retrospective, the difficult application of the guidelines suggested by the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and Cochrane handbook due to the nature of this specific condition and intervention, and the difficulty in assessing reporting bias. The results of the current study indicate that sialendoscopy is an effective and safe method for the treatment of sialolithiasis in children and should be implemented in daily clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rationale
Sialolithiasis is a relatively common disease in daily clinical practice. Although it is less common in children, the symptoms cause a considerable burden to them and their caregivers. Its treatment varies. The application of sialendoscopy began in 1990 [1,2,3,4,5,6]. Its use is constantly expanding as a new, minimally invasive method of treating sialolithiasis. During the early years, many surgeons experimented by using finer instruments and described their initial experiences [7,8,9,10,11,12,13,14]. Many more enriched the current knowledge by exploring several aspects of sialendoscopic management of sialolithiasis and standardized the procedure [15,16,17,18,19,20,21,22,23]. The first paper including pediatric patients with sialolithiasis was published in 1997 [11] while the first paper involving exclusively children was published in 2000 [24]. Since then, several more papers have been published regarding sialendoscopy in sialolithiasis in children [25,26,27,28,29].
A systematic review was published in 2018 regarding the use of sialendoscopy in salivary gland diseases in children [30]. However, cases of sialolithiasis were not examined separately. The findings were grouped in a table, without drawing clear conclusions regarding the effectiveness and safety of the method in children with sialolithiasis. Another, more recent review, addressed pediatric salivary gland stones over the last half-century, without posing a specific research question, but rather reported several data without specific quantitative synthesis [31].
Objectives
The purpose of this systematic review is to assess the effectiveness and safety of sialendoscopy as an intervention in children with sialolithiasis, based on the existing relevant literature, according to the most recent guidelines of the PRISMA-statement (Preferred Reporting Items for Systematic reviews and Meta-Analyses) [32], as well as based on the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions version 6.3 [33].
Methods
Eligibility criteria
Population
We included studies involving children suffering from sialolithiasis. Children were defined as patients up to 18 years of age, with the majority required to be under 16 years of age (for studies that did not provide individual patient characteristics, we derived indicative information from the mean age). Cases of sialolithiasis were defined as those in which a stone was found either preoperatively or postoperatively.
Intervention
The intervention to be studied is interventional sialendoscopy-based techniques, such as basket removal, as well as combined.
Outcomes
Successful stone removal is the primary outcome studied in the present study, thus studies that clearly described the effectiveness of the intervention were included. The secondary outcome of the study is the safety of the methods, as an expression of the complications presented, however, studies that did not contain the relevant data were not excluded.
All eligible studies were included regardless of design (retrospective and prospective), date, and language of publication. Cases in which the pathology was related to malignant salivary gland diseases were excluded.
Information sources
We searched databases MEDLINE and PubMed Central (through PubMed), ScienceDirect, Cochrane Central Register of Controlled Trials (CENTRAL) and citation indexes Scopus και Google Scholar. To identify ongoing and unpublished studies, we searched trial registers ClinicalTrials.gov, WHO International Clinical Trials Registry Platform (ICTRP), and EU Clinical Trials Register. Gray Matters and OpenGrey (archived) databases were used for gray literature searches, Open Access Theses and Dissertations (OATD), Center for Research Libraries (CRL) and DART-Europe for theses and dissertations, CENTRAL and Zetoc for conference proceedings, and PROSPERO and Epistemonikos for systematic reviews. The last search was conducted on September 18, 2022.
Search strategy
Initially, we performed a draft search in PubMed with the terms “pediatric sialolithiasis sialendoscopy”. We extracted the final search terms from the titles and abstracts of the resulting studies, and with the help of the PubMed PubReMiner tool. The full search strategy for the databases and citation indexes can be found in Supplementary Table 1.
Finally, forwards and backwards citation searching was performed on the references of the studies that met the inclusion criteria, to identify additional studies. These references were checked against those already identified, for the existence of any additional studies that were not identified by the initial search strategy.
In addition, a peer review of the search strategy was conducted, according to the guidelines of the PRESS checklist (Peer Review of Electronic Search Strategy) [34].
Selection process
Initially, all entries identified during the search were entered into the citation management software Endnote. With the help of the software duplicate references were removed. The titles and abstracts of the remaining studies were reviewed by two researchers (AS and IK) in order to screen those that were suitable for inclusion in the data synthesis. For these studies, the full text was retrieved where possible and reviewed in detail. After excluding studies that did not meet the inclusion criteria, studies that were suitable for inclusion were identified. Disagreements on exclusion or inclusion were discussed and solved by consensus.
Data collection process
We designed a data extraction form taking into consideration the TIDieR checklist (Template for Intervention Description and Replication) [35]. Two researchers (AS and IK) extracted eligible data. Extracted data were compared and differences were addressed and resolved.
Data items
Data were sought primarily for the effectiveness and safety of sialendoscopy in children, which were the main outcomes of our study. Therefore, we recorded the cases of success, as an indicator of the effectiveness of the method. For method safety, data on complications in each study were pooled.
Additionally, we collected data regarding:
-
the study: year of publication, authors, source of publication, design, sample size, country
-
the patients: age, gender
-
the condition: affected gland, symptoms, imaging, stone size, coexistence of stenoses
-
the intervention: type of anesthesia, surgical time, instruments used, irrigation technique, stone removal technique, postoperative treatment
-
the follow-up: duration, recurrences
Study risk of bias assessment
The study risk of bias in the studies was assessed using the Cochrane tool for non-randomized studies ROBINS-I (Risk Of Bias In Non-randomized Studies of Interventions) [36]. This tool assesses seven bias domains: confounding, selection of participants, classification of interventions, deviation from intended intervention, missing data, measurement of outcomes, and selection of the reported result. The response options for each domain are low, moderate, severe, or critical risk of bias. Two reviewers assessed the risk of bias in each study independently. Discrepancies were solved by consensus for each domain, and the overall risk of bias for each study was derived. The Robvis tool was used to create the corresponding graphs [37].
Synthesis methods
For the quantitative synthesis of the data, we decided to include all the studies that were identified, except for the case report [38], because case reports are likely to report only successful treatment cases and thus carry a high risk of publication bias, as well as their inclusion in a systematic review is problematic in many areas.
For the effectiveness of the method, a meta-analysis was performed by calculating the pooled proportion of the weighted means of the success rates, using the Miller method in a fixed effects model [39]. Additionally, we investigated heterogeneity and performed sensitivity analyses.
A meta-analysis was also performed on the safety of sialendoscopy, using the same method. The safety rate was calculated based on the cases in which there was no intraoperative or immediate postoperative complication among the total of sialendoscopy procedures performed. StatsDirect software was used for the statistical analysis and visual presentation of the data.
Reporting bias assessment
To estimate and minimize reporting bias, we also searched information sources other than published studies. The risk for unreported results in published studies (known unknowns) was assessed. We also addressed the possibility of missing studies from the synthesis (unknown unknowns) using funnel plots and the Egger test [40].
Certainty assessment
Two researchers (AS and IK) independently assessed the certainty of the evidence, using the GRADE considerations (Grades of Recommendation, Assessment, Development and Evaluation) [41,42,43]. The five areas assessed are risk of bias, heterogeneity or inconsistency, indirectness, imprecision, and publication bias. The certainty of evidence is ranked as high/moderate/low/very low. Any disagreements were solved by consensus and the results are listed in a “Summary of findings” table.
Results
Study selection
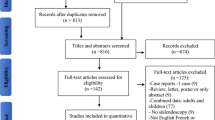
The search yielded 1620 entries. After removing duplicates as well as problematic entries, 955 entries came up, which were screened (title and abstract). After screening, 56 studies were retrieved for full-text review. Finally, 14 studies were included. We performed forwards and backwards citation searching to identify additional studies. We identified 240 and 176 references respectively, however, no additional studies meeting the inclusion criteria were found.
The full text could not be retrieved in two studies. After a full-text review, 42 studies were excluded. Six studies were excluded because they did not report the ages of the participating patients. Five studies were excluded because full-text review revealed that they did not include children. 27 studies were excluded because, while they included children, they did not examine outcomes separately between children and adults. Two studies were excluded because while the title referred to pediatric patients, they included patients older than 18 years. One study did not include pediatric patients with sialolithiasis, while another did not separately report the results of sialendoscopy in cases of sialolithiasis. One study was excluded from the quantitative data synthesis because it was a case report. 13 studies were included in the quantitative data synthesis. The excluded and included studies are cited in Supplementary Tables 2 and 3, respectively.
The flow diagram is shown in Supplementary Fig. 1.
Study characteristics
The study characteristics studies in terms of the main author, the year of publication, the country of conduct, the period of the study, its design, the total number of affected glands (instead of the total number of patients because in some patients more than one gland was affected), the age, and gender are listed in Table 1. In addition, success, complications, follow-up time, and any recurrences are presented in Table 2. Stone removal techniques, for studies specifying them, are presented in Fig. 1. The most frequently used was wire basket removal, followed by LASER fragmentation and combined technique, and a few cases of papillotomy (direct cut-down and removal after sialendoscopy). The other study data collected include indications, imaging, instruments used, irrigation fluid, stone removal technique, sialendoscopy findings (specific gland, stone size, stenoses), surgery duration, type of anesthesia, and postoperative management can be found in Supplementary Tables 4–7.
Risk of bias in studies
To assess the risk of bias in the studies, we used the Cochrane tool for non-randomized studies ROBINS-I (Risk Of Bias In Non-randomized Studies of Interventions). One study was judged to be at high risk of bias, one at moderate risk, and the rest at low risk.
The “traffic light” plots showing the risk of bias assessment for the individual studies, as well as the overall risk of bias, are provided in Supplementary Figs. 2 and 3 respectively.
Results of individual studies
The results of the studies regarding the safety and effectiveness of endoscopy are listed below as forest plots (Figs. 2 and 3).
Results of syntheses
Effectiveness
In the synthesis of the results, 13 studies were included that described the effectiveness of sialendoscopy in sialolithiasis in children. A total of 133 cases were included.
The effectiveness of endoscopy was 95.5% (95% CI 89.8–99.3%). The heterogeneity of the meta-analysis studies was approached by the method of I2 which was found equal to 50.1%, indicating a moderate degree of heterogeneity.
The heterogeneity of the studies was then investigated. First, the pooled percentage of the weighted mean success rates was recalculated with the random effects model (DerSimonian–Laird). This was 94.4% (95% CI 84.8–99.8%). The two percentages are close, a reassuring fact about the effect of the heterogeneity of the studies on the final result.
In addition, a sensitivity analysis was performed. An approach to the heterogeneity of studies was initially attempted by excluding the Kanerva et al. study [44]. This particular study had a higher failure rate than the others as a rule but reported that the failures mostly occurred in the first half of the study period, likely reflecting the surgeons' learning curve. Indeed by excluding this particular study, the heterogeneity was significantly reduced (I2 = 28%, i.e. probably not significant). Furthermore, the effectiveness of the method was calculated at 98.2% (95% CI 93–100%).
An additional sensitivity analysis was performed including only the studies that had a low risk of bias. The results were 96.5% (95% CI 90.5–99.9), I2 = 52.8%, very similar to the original analysis, indicating that the risk of bias does not affect our results. The graphs resulting from the heterogeneity investigation and sensitivity analysis are listed in the Supplementary Information (Supplementary Figs. 4 to 6).
Safety
In the synthesis of the results, 10 studies were included that described the complications of sialendoscopy in sialolithiasis in children (a total of 113 cases). The safety of endoscopy in children was 97.2% (95% CI 91.8–100%). The heterogeneity of the studies in the meta-analysis was probably not significant (I2 = 0%).
Additional data
From the collection of data for the present study, several more interesting elements can be derived, in addition to those concerning the main outcomes that were studied. Detailed information can be found in Supplementary Tables 4–7.
The youngest recorded age of a patient who underwent sialendoscopy is two years. Boys are affected at a similar rate as girls. The incidence of sialolithiasis is overwhelmingly greater in the submandibular gland (87.5%) than in the parotid gland (12.5%). The most common indications for sialendoscopy were recurrent episodes of sialadenitis and swelling of the salivary glands during meals, while quite often the waiting time before the decision to operate was quite long. The most common imaging modalities were CT and ultrasound, but without particularly high diagnostic accuracy compared to endoscopy. Three out of the four studies that reported using a CT were conducted in the USA and one in France.
Operative time was reported in a few studies and the mean duration recorded ranged from 32 to 125 min. In the majority of cases, general anesthesia was preferred, however, in the few cases where local anesthesia was applied (only nine reported), no difficulty was reported in performing the operation. The endoscopes used had diameters from 0.8 to 2.3 mm, while the most commonly used was the “all-in-one” with a diameter of 1.3 mm. Isotonic saline was most often used for irrigation into the duct. Some surgeons also added anesthetic (most commonly xylocaine) and/or corticosteroids (most commonly prednisolone).
A variety of techniques was used to remove salivary stones, which were described to a different extent in each study. In general, smaller stones were removed primarily with a basket, microdrill, and grasping instruments. For larger stones, lasers (holmium, thulium, and CO2) were used for initial fragmentation, as well as combined techniques. Stone size ranged from 1 to 18 mm, while LSD classification was used in a few cases to describe ductal and glandular pathology. Strictures were reported in 20 cases.
Painkillers, antibiotics (most commonly amoxicillin—clavulanic acid), and corticosteroids (e.g. dexamethasone, betamethasone) were used postoperatively. The most commonly observed complication was ductal perforation which was reported in three cases. The need for a second operation was rare and occurred due to the recurrence of symptoms either due to stenosis (three cases) or residual stones (one case) that were not detected at the first operation.
Risk of reporting bias in syntheses
The search in sources outside of published studies did not retrieve additional studies.
The risk of unpublished results in published studies (known unknowns) appears to be small. In all studies identified, the authors provided data on the effectiveness of the method. In two studies [45, 46] there were no data on complications, while in one [47] the complications of sialendoscopy were not reported separately for sialolithiasis. However, the careful examination of the studies, as well as the fact that the safety of sialendoscopy was not their main outcome, do not raise suspicions about the possibility of risk of bias.
In addition, we attempted to estimate the risk of reporting bias due to studies that have been undertaken but not reported (unknown unknowns). The corresponding funnel plots are listed in Figs. 4 and 5. Using the Egger test, a statistically significant probability of risk of reporting bias is found in the meta-analysis concerning effectiveness (p = 0.0273 < 0.05), while it is not found in the meta-analysis concerning safety (p = 0.1568 > 0.05).
However, caution is needed in the interpretation of these findings. In terms of estimating funnel plots, effectiveness is measured as a percentage, de facto limiting the right-hand side of the graph to one and necessarily creating asymmetry. However, the asymmetry is more pronounced in the effectiveness graph. This, combined with the results of the Egger test, raises suspicions of a risk of reporting bias in the effectiveness meta-analysis. One possible option is indeed that studies with small success rates are not published, perhaps from clinics with limited experience. This is reinforced by the fact that the Kanerva et al. study, which had a small success rate, increased the heterogeneity of the meta-analysis (as shown by the sensitivity analysis), as well as the large learning curve of the technique. Of course, this also applies to the safety results, in which there is no statistically significant probability of a reporting bias. This, combined with the inherent limitations of the statistical approach, impose caution in risk assessment, while it remains quite possible that the results are due to chance.
Certainty of evidence
The certainty of evidence was assessed using the guidelines of the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) framework. Considering the five assessment domains, it was judged to be moderate for both outcomes. The results are also listed in the Summary of Findings table (Table 3).
Discussion
Sialendoscopy is a new, minimally invasive method for treating salivary gland diseases, which is constantly gaining ground. The growing interest in the method and its applications is reflected in the ever-increasing number of related studies published in recent years. The present systematic review and meta-analysis is the first to study the effectiveness and safety of sialendoscopy in sialolithiasis in pediatric patients. The included studies come from many centers, mainly in Europe and the USA, offering considerable diversity in approaches and techniques.
Sialendoscopy appears to be a very effective and safe method in the treatment of sialolithiasis in children, as was shown by the meta-analysis carried out. This seems to be supported by surgeons in published studies, however, without clear documentation so far.
The use of minimally invasive techniques has the advantage of preserving the gland and its functionality, while the adjacent anatomical structures remain unaffected as well. Additionally, it has the potential to significantly reduce the need for hospitalization, offering a more tolerable experience for the patient and simultaneously reducing the cost. Implementation of minimally invasive techniques for sialolithiasis reduces the necessity of gland excision to less than 5% [48]. The above benefits are particularly useful in children, and the initial use of sialendoscopy as a gland-preserving technique with diagnostic capabilities has been recommended [49]. Our study shows effectiveness > 92%, which indicates that sialendoscopy should be considered a first-line treatment in children. However, as the number of specialized centers is limited and the procedure in many countries is still not reimbursed, this seems improbable for the time being.
The safety of sialendoscopy in children was also shown to be particularly high in our study. None of the complications reported were major (Table 2). However, there have been some cases of airway obstruction when sialendoscopy was performed bilaterally for reasons not limited to sialolithiasis [47]. Even though no such events have been reported in the studies included in our systematic review, the possibility of airway emergencies cannot be ruled out, especially with bilateral procedures, and the performing surgeon should always remain vigilant.
General anesthesia seems to be the preferred option for pediatric sialendoscopy. This is more likely due to the smaller diameter of the child’s salivary ductal system as well as the potential lack of cooperation. However, this increases the cost of the procedure and possibly limits its use. Local anesthesia can be used for interventional sialendoscopy in children with good results without an increase in complication rates. However, children with sialolithiasis are not the optimal group, and local anesthesia should be utilized as an alternative option for children older than eight years old, with small stones at a proximal location [29].
The use of sialendoscopy in children, despite its potential for improved cost-effectiveness when compared to other methods, still induces a significant cost [45]. In several countries, the cost of sialendoscopy is not reimbursed by healthcare systems and insurance policies, thus limiting its use. The results of our study, while not focusing on the financial aspects, indicate that the incorporation of this effective and safe method as a standard medical care practice by healthcare systems should be considered.
Sialolithiasis is seldom seen in children and represents only 3% of all sialolithiasis cases [25]. Pediatricians are most likely to be the first to examine a child with salivary gland swelling and pain, and sialolithiasis should be included in the differential diagnosis despite being relatively rare [50]. Furthermore, pediatricians need to be aware of the indications, as well as the safety and effectiveness of sialendoscopy in children, as was shown in our study. A multidisciplinary approach to children with sialolithiasis should therefore be encouraged.
There were some limitations to the studies included in this review. The number of included studies was relatively small because the method is relatively recent, the learning curve long and its use limited. The majority of studies were retrospective. In addition, many studies analyzed sialendoscopy as a whole, without focusing on its application in sialolithiasis and without analyzing pediatric patients separately.
Due to the nature of the specific condition and the specific intervention, it is difficult to conduct studies with the elements of randomization, blinding, and control group. This made it difficult to accurately apply the PRISMA and Cochrane handbook guidelines to some aspects of the study. The outcome of the meta-analysis was expressed as a pooled percentage instead of more common effect measures such as ratio ratios. Estimating the risk of reporting bias was difficult because of the above limitations, as well as for the reasons mentioned in the corresponding section.
Conclusion
Implications for practice
The findings of the present study show that sialendoscopy is a method with a high success rate and minimal complications for the treatment of sialolithiasis in children. It has the prospect of greatly reducing gland removal surgeries in cases of sialolithiasis, offering the advantage of treating without creating a surgical wound, preserving the gland, and avoiding possible complications of surgical resection. Otolaryngologists and maxillofacial surgeons should be trained in it and its use should be expanded and incorporated into otolaryngology and maxillofacial surgery clinics, especially those dealing with salivary gland disease in children.
Implications for future research
As more studies on the subject are published, existing knowledge will be enriched. Success and safety rates will be able to be more accurately determined, as well as knowledge of the variations in techniques used and potential complications. In this context, it would be important to publish prospective studies, as well as studies from centers with limited experience, in order to reduce the risk of bias in future meta-analyses. In addition, it is important to publish more studies that analyze the data separately for pediatric patients and for sialolithiasis.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Konigsberger R, Feyh J, Goetz A, Schilling V, Kastenbauer E (1990) Endoscopic controlled laser lithotripsy in the treatment of sialolithiasis. Laryngorhinootologie 69:322–323. https://doi.org/10.1055/s-2007-998200
Konigsberger R, Feyh J, Goetz A, Kastenbauer E (1993) Endoscopically-controlled electrohydraulic intracorporeal shock wave lithotripsy (EISL) of salivary stones. J Otolaryngol 22:12–13
Katz P (1993) New treatment method for salivary lithiasis. Rev Laryngol Otol Rhinol (Bord) 114:379–382
Katz P (1991) Endoscopy of the salivary glands. Ann Radiol (Paris) 34:110–113
Katz P (1990) New method of examination of the salivary glands: the fiberscope. Inf Dent 72:785–786
Gundlach P, Scherer H, Hopf J, Leege N, Müller G, Hirst L et al (1990) Endoscopic-controlled laser lithotripsy of salivary calculi. In vitro studies and initial clinical use. HNO 38:247–250
Zenk J, Koch M, Bozzato A, Iro H (2004) Sialoscopy–initial experiences with a new endoscope. Br J Oral Maxillofac Surg 42:293–298. https://doi.org/10.1016/j.bjoms.2004.03.006
Marchal F, Becker M, Dulguerov P, Lehmann W (2000) Interventional sialendoscopy. Laryngoscope 110:318–320. https://doi.org/10.1097/00005537-200002010-00026
Nahlieli O, Baruchin AM (1999) Endoscopic technique for the diagnosis and treatment of obstructive salivary gland diseases. J Oral Maxillofac Surg 57:1394–1401. https://doi.org/10.1016/s0278-2391(99)90716-4
Marchal F, Dulguerov P, Lehmann W (1999) Interventional sialendoscopy. N Engl J Med 341:1242–1243. https://doi.org/10.1056/NEJM199910143411620
Nahlieli O, Baruchin AM (1997) Sialoendoscopy: three years’ experience as a diagnostic and treatment modality. J Oral Maxillofac Surg 55:912–918. https://doi.org/10.1016/s0278-2391(97)90056-2
Iro H, Zenk J, Benzel W (1995) Laser lithotripsy of salivary duct stones. Adv Otorhinolaryngol 49:148–152. https://doi.org/10.1159/000424360
Nahlieli O, Neder A, Baruchin AM (1994) Salivary gland endoscopy: a new technique for diagnosis and treatment of sialolithiasis. J Oral Maxillofac Surg 52:1240–1242. https://doi.org/10.1016/0278-2391(94)90043-4
Arzoz E, Santiago A, Garatea J, Gorriaran M (1994) Removal of a stone in Stensen’s duct with endoscopic laser lithotripsy: report of case. J Oral Maxillofac Surg 52:1329–1330. https://doi.org/10.1016/0278-2391(94)90059-0
Marchal F, Chossegros C, Faure F, Delas B, Bizeau A, Mortensen B et al (2008) Salivary stones and stenosis. A comprehensive classification. Rev Stomatol Chir Maxillofac 109:233–236. https://doi.org/10.1016/j.stomax.2008.07.004
Iro H, Zenk J, Koch M, Bozzato A (2008) Storz. The Erlangen salivary gland project, Part I, Sialendoscopy in obstructive diseases of the major salivary glands. Tuttlingen Endo-Press, Tuttlingen
Nahlieli O, Shacham R, Zagury A, Bar T, Yoffe B (2007) The ductal stretching technique: an endoscopic-assisted technique for removal of submandibular stones. Laryngoscope 117:1031–1035. https://doi.org/10.1097/MLG.0b013e31804f8163
Nahlieli O, Nakar LH, Nazarian Y, Turner MD (2006) Sialoendoscopy: a new approach to salivary gland obstructive pathology. J Am Dent Assoc 137:1394–1400. https://doi.org/10.14219/jada.archive.2006.0051
Katz P (2004) New techniques for the treatment of salivary lithiasis: sialoendoscopy and extracorporal lithotripsy: 1773 cases. Ann Otolaryngol Chir Cervicofac 121:123–132. https://doi.org/10.1016/s0003-438x(04)95499-0
Marchal F, Dulguerov P (2003) Sialolithiasis management: the state of the art. Arch Otolaryngol Head Neck Surg 129:951–956. https://doi.org/10.1001/archotol.129.9.951
Nahlieli O, London D, Zagury A, Eliav E (2002) Combined approach to impacted parotid stones. J Oral Maxillofac Surg 60:1418–1423. https://doi.org/10.1053/joms.2002.36097
Zenk J, Zikarsky B, Hosemann WG, Iro H (1998) The diameter of the Stenon and Wharton ducts. Significance for diagnosis and therapy. HNO 46:980–985. https://doi.org/10.1007/s001060050345
Katz P (1998) A new therapeutic approach to salivary calculi: extracorporeal lithotripsy. Rev Stomatol Chir Maxillofac 99(Suppl 1):109–111
Nahlieli O, Eliav E, Hasson O, Zagury A, Baruchin AM (2000) Pediatric sialolithiasis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90:709–712. https://doi.org/10.1067/moe.2000.109075a
Iro H, Zenk J (2014) Salivary gland diseases in children. GMS Curr Top Otorhinolaryngol Head Neck Surg 13:Doc06. https://doi.org/10.3205/cto000109
Francis CL, Larsen CG (2014) Pediatric sialadenitis. Otolaryngol Clin N Am 47:763–778. https://doi.org/10.1016/j.otc.2014.06.009
Bruch JM, Setlur J (2012) Pediatric sialendoscopy. Adv Otorhinolaryngol 73:149–152. https://doi.org/10.1159/000334474
Faure F, Froehlich P, Marchal F (2008) Paediatric sialendoscopy. Curr Opin Otolaryngol Head Neck Surg 16:60–63. https://doi.org/10.1097/MOO.0b013e3282f45fe1
Konstantinidis I, Chatziavramidis A, Tsakiropoulou E, Malliari H, Constantinidis J (2011) Pediatric sialendoscopy under local anesthesia: limitations and potentials. Int J Pediatr Otorhinolaryngol 75:245–249. https://doi.org/10.1016/j.ijporl.2010.11.009
Schwarz Y, Bezdjian A, Daniel SJ (2018) Sialendoscopy in treating pediatric salivary gland disorders: a systematic review. Eur Arch Otorhinolaryngol 275:347–356. https://doi.org/10.1007/s00405-017-4830-2
Chen T, Szwimer R, Daniel SJ (2022) The changing landscape of pediatric salivary gland stones: a half-century systematic review. Int J Pediatr Otorhinolaryngol 159:111216. https://doi.org/10.1016/j.ijporl.2022.111216
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160. https://doi.org/10.1136/bmj.n160
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). London: Cochrane Collaboration; 2021. www.training.cochrane.org/handbook.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C (2016) PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 75:40–46. https://doi.org/10.1016/j.jclinepi.2016.01.021
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D et al (2014) Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ Br Med J 348:g1687. https://doi.org/10.1136/bmj.g1687
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
McGuinness LA, Higgins JPT (2020) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synthesis Methods. https://doi.org/10.1002/jrsm.1411
Lin YK, Geddes A, Lloyd TE, Jones SD (2021) Paediatric sialendoscopy under local anaesthesia: a case report. Adv Oral Maxillofacial Surg 3:100139. https://doi.org/10.1016/j.adoms.2021.100139
Miller JJ (1978) The inverse of the Freeman-Tukey double arcsine transformation. Am Stat 32:138. https://doi.org/10.2307/2682942
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926. https://doi.org/10.1136/bmj.39489.470347.AD
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ (2008) What is “quality of evidence” and why is it important to clinicians? BMJ 336:995–998. https://doi.org/10.1136/bmj.39490.551019.BE
Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A et al (2008) Going from evidence to recommendations. BMJ 336:1049–1051. https://doi.org/10.1136/bmj.39493.646875.AE
Kanerva M, Tapiovaara L, Aro K, Saarinen R (2020) Pediatric sialendoscopy: an 11-year study from a single tertiary care center. Int J Pediatr Otorhinolaryngol 131:109869. https://doi.org/10.1016/j.ijporl.2020.109869
Velasquez N, Gardiner L, Ramprasad V, Shaffer A, Jabbour N, Stapleton A (2022) Cost analysis of sialendoscopy for the treatment of salivary gland disorders in children. Int J Pediatr Otorhinolaryngol 153:111020. https://doi.org/10.1016/j.ijporl.2021.111020
Ziegler CM, Steveling H, Seubert M, Mühling J (2004) Endoscopy: a minimally invasive procedure for diagnosis and treatment of diseases of the salivary glands. Six years of practical experience. Br J Oral Maxillofac Surg 42:1–7. https://doi.org/10.1016/s0266-4356(03)00188-8
Martins-Carvalho C, Plouin-Gaudon I, Quenin S, Lesniak J, Froehlich P, Marchal F et al (2010) Pediatric sialendoscopy: a 5-year experience at a single institution. Arch Otolaryngol Head Neck Surg 136:33–36. https://doi.org/10.1001/archoto.2009.184
Iro H, Zenk J, Escudier MP, Nahlieli O, Capaccio P, Katz P et al (2009) Outcome of minimally invasive management of salivary calculi in 4,691 patients. Laryngoscope 119:263–268. https://doi.org/10.1002/lary.20008
Zenk J, Koch M, Klintworth N, Konig B, Konz K, Gillespie MB et al (2012) Sialendoscopy in the diagnosis and treatment of sialolithiasis: a study on more than 1000 patients. Otolaryngol Head Neck Surg 147:858–863. https://doi.org/10.1177/0194599812452837
Chung MK, Jeong HS, Ko MH, Cho HJ, Ryu NG, Cho DY et al (2007) Pediatric sialolithiasis: what is different from adult sialolithiasis? Int J Pediatr Otorhinolaryngol 71:787–791. https://doi.org/10.1016/j.ijporl.2007.01.019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Research involving human participants and/or animals
This is a systematic review using publicly available data from published studies and performed in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments. The Scientific Council of the Papageorgiou Hospital of Thessaloniki has confirmed that no ethical approval is required.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Skalias, A., Garefis, K., Markou, K. et al. The effectiveness and safety of sialendoscopy for sialolithiasis in children: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 280, 3053–3063 (2023). https://doi.org/10.1007/s00405-023-07877-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07877-2