Abstract
Purpose
To report on failures related to active middle ear implants (AMEI) surgery, within a series of subjects treated at a single Implanting Center.
Methods
A retrospective review of 79 cases of implanted AMEI has been performed to report the failure ratio, the causes for the failure and the selected rehabilitative solution. The AMEI included 25 Vibrant Soundbridge® (Medel, Innsbruck, Austria), 20 as round window vibroplasty (RW-VSB) for mixed hearing loss, 5 as incus-vibroplasty for sensorineural hearing loss; 7 MET/Carina® (Cochlear, Melbourne, Australia), 2 MET for mixed and sensorineural hearing loss, 5 Carina for sensorineural hearing loss; 43 Esteem® (EnvoyMedical, St Paul, USA) for sensorineural hearing loss; 3 Maxum® (Ototronics, Texas, USA) for sensorineural hearing loss; 1 Codacs® (Cochlear, Melbourne, Australia) for severe mixed hearing loss.
Results
The overall complication rate affected 20% of the implanted devices, individually ranging from 6.9 to 100%. Hardware system failures were recorded in all the AMEI, ranging from 10 to 50%. The alternative auditory rehabilitation included replacement of the same system in 2 cases, use of a conventional hearing aid in 3 cases, Cochlear implantation in 4 cases and implantation in the contralateral ear in 2 cases.
Conclusion
The present clinical experience showed that, in spite of the successful functional rate displayed by the majority of the AMEI implantees, complications may occur to a certain percentage of cases and should prompt the professionals to select alternative solutions, starting from the (re)adoption of a conventional hearing aid and ending up to Cochlear implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The active middle ear implants (AMEI) are presently considered an alternative tool for rehabilitating—in selected cases—different type and severity of hearing loss, when the use of a conventional hearing aid (cHA) is inappropriate or inadequate [1]. Contrary to a cochlear implant (CI) which is indicated for helping a total or near-total decrease of speech discrimination that generally accompanies severe or profound sensorineural hearing loss, the audiological indications for an AMEI include conductive, mixed or moderate to severe sensorineural hearing loss [2, 3]. Conductive and mixed hearing loss usually derive from middle ear pathology or surgery: hence, one should always consider the potential risk of a further functional deterioration due the original disease over the years, requiring at a later stage a different solution in respect to the first choice. Sensorineural hearing loss also entails the possibility of threshold deterioration over time, although AMEI are advisably indicated only for hearing impairments that have remained stable for a considerable amount of time.
The AMEI are composed by sophisticated technological systems that accomplish their duty by delivering a vibratory movement to the anatomical element of the ossicular chain/inner ear chosen for the coupling, using either an electromagnetic or piezoelectric modality [4]. Being artificial, non-biological systems, the possibility for a foreign body reaction or rather their breakdown with consequent functional interruption, have to be taken into account in view of adopting alternative rehabilitative solutions.
At our Implanting Center, there has been the opportunity to apply, albeit with different numbers, all types of semi- and fully implantable AMEI available today, mostly for rehabilitation of mixed and sensorineural hearing loss. Besides an overall general satisfaction of the implanted subjects, in a few of them there has been the need for device removal and subsequent substitution with the same system or by alternative rehabilitative solutions, including cHA and CI.
The aim of the present work is to report the experience of a single Implanting Center on AMEI revision surgery, including their explantation, with particular emphasis on the underlying causes, the surgical procedures and the rationale for choosing alternative auditory solutions.
Materials and methods
From 2005 to 2018, 79 AMEI have been implanted at a Tertiary University Hospital, including: 25 Vibrant Soundbridge® (Medel, Innsbruck, Austria), 20 as round window vibroplasty (RW-VSB) for mixed hearing loss, 5 as incus-vibroplasty for sensorineural hearing loss; 7 MET/Carina® (Cochlear, Melbourne, Australia), 2 MET for mixed and sensorineural hearing loss, 5 Carina for sensorineural hearing loss; 43 Esteem® (Envoymedical, St Paul, USA) for sensorineural hearing loss; 3 Maxum® (Ototronics, Texas, USA) for sensorineural hearing loss; 1 Codacs® (Cochlear, Melbourne, Australia) for severe-to profound mixed hearing loss (Table 1).
Beyond the audiological indications, each AMEI has been used also on the ground of different factors that included its availability in the Hospital at the time planned for implantation; the lack of alternative solutions; and a specific patient’s request (in particular when considering a fully implantable type).
At a certain distance from their surgical application, some of these devices needed to be explanted for different reasons that are listed in Table 2, in which also the adopted alternative solution is shown.
Each AMEI required a specific surgical approach in relation to the decision to replace it with a similar device or to substitute it with an alternative solution that was also driven by the patient’s auditory and clinical situation.
Esteem® (Envoymedical, St Paul, USA)
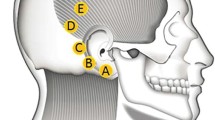
It is a fully implantable device indicated for moderate-to-severe sensorineural hearing loss [5]. When revising subjects with residual hearing and potential return to use a cHA, the procedure aims to reconnect the interrupted ossicular chain that represents an obligatory consequence of the primary surgical technique. In analogy with all the procedures performed in presence of an electronic device, monopolar electrocautery must be banned. Due to the particular assemblage of this device, particular care should be taken to carefully free the ossicular chain from the cemented points, to avoid a possible inner ear damage due to the mechanical transmission to the mobile stapes (Fig. 1).
The first important maneuver, after exposing the cemented mastoidectomy cavity (Fig. 1), is to look through the posterior tympanotomy and peel (or pick) off the cement covering the actuator, to allow its careful displacement from the stapes head. Once accomplished it, the surgeon performs a similar maneuver on the device’s sensor (Fig. 2). Once both transducers have been separated from the ossicles, the hydroxyapatite cement is removed from the mastoidectomy cavity via drilling and/or curetting it away so as to allow the removal of the whole implant (bodies and cables). After this preliminary step, the next one aims to reconnect the interrupted ossicular chain. In our experience this was achieved via either cementing the gap between the stump of the long process of the incus to the stapes head, or using the interposition of a passive, titanium prosthesis (Krause K-Helix Crown®, Grace Medical, Memphis, USA). This reconstructive surgery will theoretically enable the patient to wear a cHA.
In those Esteem® implantees with no residual hearing, it is not necessary to pay particular attention to the integrity of the cemented ossicular chain, since the ultimate goal is to simultaneously replace the device with a CI. This can be achieved via the already wide posterior tympanotomy access and the appropriate preparation of the round window niche.
Carina® (Cochlear, Melbourne, Australia)
Carina® is a fully-implantable system based on the mechanical stimulation of the ossicular chain by an actuator placed on the incus body through a limited epitympanectomy approach. When performing a revision for this device, with the aim to replace it with a new similar system, the main caution should be not to inadvertently manipulate the incus which is connected with the device’s actuator, since preservation of the optimal ossicular continuity/motility is the prerequisite for the new replaced device to properly work. This can be achieved by first pulling back—via a screwdriver on the internal micro manipulator system—the actuator placed on the incus body, keeping the mounting bracket screwed on the skull in place. After removal of the damaged device, the previously positioned mounting bracket serves as a guide for the new device. Contrarily, if the device’s explantation will simultaneously be followed by a CI, surgery will also encompass the removal of the mounting bracket and the performance of a mastoidectomy with posterior tympanotomy that was not initially necessary for this device’s application.
Vibrant Soundbridge® (MedEl, Innsbruck, Austria)
The VSB is a semi-implantable AMEI indicated for any type of hearing loss, by coupling the actuator (Floating Mass Transducer) to the incus, round window or oval window. The surgical revision/substitution at our Center occurred only in RW-VSB cases that, in our practice, represents the gold standard for the functional rehabilitation of open cavities with severe, mixed hearing loss for which a cHA or bone conductive implants are inadequate [5]. The most critical step in this revision surgery is represented by the possible harm to the inner ear when detaching the floating mass transducer from the round window niche usually occupied by thick and tenacious scar tissue. For this purpose, cutting rather than by pulling maneuvers are advised. If the revision was motivated by an imperfect coupling, the same device can be temporarily moved while enlarging the coupled area of the round window membrane, followed by its repositioning. A similar technique could be used in case of hardware failure with replacement with a new similar system. When facing, instead, cases with profound hearing deterioration, a simultaneous ipsilateral CI or alternative solution in the contralateral ear can be chosen.
Codacs® (Cochlear, Melbourne, Australia)
This device has been introduced for treating severe mixed hearing loss, such as in far-advanced otosclerosis. Surgery consists in coupling a piston prosthesis anchored to an artificial incus to a platinotomy via a posterior tympanotomy approach. At the present time, this device has been withdrawn from the market, and our experience is limited to only one subject. Considering the already poor pre-operative hearing threshold, a further deterioration could be likely to occur with consequent functional interruption, so that a CI can be simultaneously positioned after its explantation, via the performed posterior tympanotomy.
Maxum® (Ototronics, Texas, USA)
It is a semi-implantable device, indicated for moderate-to severe sensorineural hearing loss. Surgery uses a transcanal approach with a tympano-meatal flap that allows the exposure of the incudo-stapedial joint, where the magnetic actuator is placed, anchored and cemented. Similarly to primary surgery, revisions can be performed under local anesthesia. Before removing the magnet, the ionomeric cement that makes the device assembled with the ossicular chain needs to be removed, so that its hooks can be set free, enabling the device removal.
All the subjects signed the informed consent specific for each procedure. The study was conducted according to the Helsinki declaration guidelines.
Results
In all the devices’ failures that required an auditory rehabilitation with a CI, revision surgeries could always be successfully completed by applying the standard procedure.
Esteem® (Envoymedical, St Paul, USA)
In two subjects, the device’s explantation was simultaneously performed along with reconnection of the interrupted ossicular chain at the level of the long process of the incus, as described above, so as to allow them to wear again a cHA. In two other subjects, due to the severe deterioration of the hearing threshold, CI was simultaneously performed with explantation. In only one patient, no further decision on hearing rehabilitation was taken, since explantation was motivated by an organ transplantation protocol.
Vibrant Soundbridge® (Medel, Innsbruck, Austria)
In two RW-VSB subjects, an interruption of device function was noticed due to an unspecified hardware issue, and a replacement surgery has been performed. In two other RW-VSB subjects a profound hearing loss was evidenced: in one case after a revision procedure for a limited functional recovery at the first fitting; in the other case without any apparent reason. In both of them, due to a concomitant conductive hearing loss in the contralateral ear, it was decided to implant this latter with a bone conductive device.
MET/Carina® (Cochlear, Melbourne, Australia)
In one case where a semi-implantable model (MET) was applied, the surgical revision inadvertently caused a minor damage to the incudo-malleolar joint so that, when trying to replace it with an Esteem®, this was not possible for the impaired motility of the ossicular chain detected by the intra-operative Laser Doppler Vibrometry, and a cHA was, therefore, chosen. In one subject, the device was successfully replaced. The third explanted subject, instead, needed a CI due to an unexpected total loss of hearing. Especially when considering fully implantable devices, one may assume that this unpredictable complication could be originated by the baseline severe hearing loss as well as by its uninterrupted use, with a continuous inner ear stimulation [6].
Codacs® (Cochlear, Melbourne, Australia)
The implanted subject showed loss of device function due to the total decrease of hearing threshold 1 year after implantation. Since a simultaneous application of a CI was planned, the removal of the device was uneventful and surgery short in duration due the preexisting posterior tympanotomy. Our experience consisted in the removal of the device’s assemblage, as well as of the oval window piston prosthesis, followed by oval window sealing, and insertion of a CI through the RW niche area, via the already-existing posterior tympanotomy.
Maxum® (Ototronics, Texas, USA)
The device explant was needed in only one subject for allowing the execution of an MRI. After the device removal, the patient declined a replacement surgery and decided for a cHA.
Discussion
AMEI application encompasses a demanding task for all the involved professionals, including the surgeons, who are called to familiarize not only with the primary procedures but also with the issues related to their possible revision. In this regard, one may assume that the surgeon’s learning curve that generally grows after several primary applications with each device, plays an important role also in the revision procedures that can be implemented by technical notes not necessary during the primary surgery.
When the AMEI team, which also includes audiologists, engineers and trained technical personnel, reaches the unanimous decision of performing a revision of the implanted device, it is necessary to predict if and what kind of auditory rehabilitation could be eventually planned further, taking mainly into account the reason for the explantation that could be multifold and will be analyzed below.
The AMEI breakdown deserves to be taken into consideration first, since this complication is always possible with any electronic device, whether it is implanted or not, even in systems that have been released after a very careful analysis by the responsible organizations (FDA, for example). However, the majority of them are available, available since more than a decade and reports from the literature citing this aspect are scanty. The experience at our Implanting Center with the most used AMEI showed that this issue was infrequently encountered (2 cases for VSB® and MET/Carina®, none for Esteem®). Should this occur, an appropriate counselling with the patient is necessary to share the decision of a replacement surgery or rather of an alternative solution that may also include reconsidering a cHA, especially if it was worn before.
A second important reason for requiring AMEI revision/explantation was the lack of the expected benefit, i.e., an immediate or delayed loss of the vibratory efficacy of the AMEI’s actuator on the selected coupling structure, as shown by the post-operative audiological evaluation, at the first fitting session or at the late controls. In the first case, an early intervention can be planned, as it was experienced in two RW-VSB cases that needed to adjust the coupling of the floating mass transducer to the round window membrane; and in three Esteem® subjects who showed limited amplification due to fibrous tissue growth inside the middle ear cavity. When the benefit declines after months or years from the AMEI application, the first parameter to check is the hearing threshold level, in terms of bone conduction (BC), that could have deteriorated to the point to make the device unable to function. If this is the case, one may hypothesize that the most likely reason could be the natural progression of the hearing loss over time. It is noteworthy to remark that, in our series, a BC deterioration has been observed, over the time, with nearly all the devices, and especially in those subjects that were selected with an advanced hearing loss, nearly being off-label according to the Companies’ recommendations [7]. This finding has been in particular noticed in the Esteem®’s implantees who were all selected for a bilateral, nearly symmetric sensorineural hearing loss. Since the hearing deterioration was only observed in the operated ear and not in the contralateral, non-implanted one, the possibility that it could originate from the primary cause for the hearing loss can be reasonably ruled out. One might, therefore, speculate that the continuous AMEI mechanical vibratory activity, especially in the fully implantable systems that can be left active during the whole day, would play a detrimental role in this regard. The total loss of hearing was also one of the causes for requiring explantation of the AMEI applied for sensorineural hearing loss, in Carina®, Esteem® and Codacs®, all successfully rehabilitated with a CI.
An additional reason that could raise the requirement for an AMEI explantation is the need of performing an MRI. This was occurring only in one subject of our study group, i.e., one Maxum® case, but it certainly represents an important issue to negotiate when counselling with any AMEI candidate. The AMEI manufacturers, mostly also CI companies, are paying more and more attention to this issue when developing new device generations for limiting or abolishing the risk of loss of the device function, due to device shift or demagnetization, as well as to get rid of the shadowing cone effects on the surrounding areas that would limit the MRI diagnostic power. In addition, the eventual noxious effect from an outside magnetic field can disassemble the contact between the AMEI actuator and the coupling structure, leading to a sudden loss of its function.
One limitation of the present study is represented by the different figures of the implanted devices that may offer the wrong impression of a greater likelihood of revisions in the less utilized devices. Since the reasons for explantation were in common among all the devices, it has been considered worth mention them regardless of the numerosity of subject for each device.
It is possible to conclude that, in spite of the high successful rate displayed by the majority of the AMEI implantees, complications that require a surgical revision may occur, although in a limited percentage of cases, with solutions including replacement or further rehabilitative procedures. The AMEI team should, therefore, be prepared for facing this eventuality by selecting alternative solutions to be shared and negotiated with the patients, and that may range from the simple (re)adoption of a cHA to the more complex CI surgery.
References
Lee JM, Jeon JH, Moon IS, Choi JY (2017) Benefits of active middle ear implants over hearing aids in patients with sloping high-tone hearing loss: comparison with hearing aids. Acta Otorhinolaryngol Ital 37(3):218–223
de Abajo J, Sanhueza I, Giron L, Manrique M (2013) Experience with the active middle ear implant in patients with moderate-to-severe mixed hearing loss: indications and results. OtolNeurotol 34(8):1373–1379
Boeheim K, Pok S-M, Schloegel M, Filzmoser P (2010) Active middle ear implant compared with open-fit hearing aid in sloping high-frequency sensorineural hearing loss. OtolNeurotol 31(3):424–429
Park IY, Shimizu Y, O’Connor KN, Puria S, Cho JH (2010) Comparisons of electromagnetic and piezoelectric floating-mass transducers in human cadaveric temporal bones. Hear Res 272(1–2):187–192
Marzo SJ, Sappington JM, Shohet JA (2014) The Envoy Esteem implantable hearing system. OtolaryngolClin North 47(6):941–952
Barbara M, Volpini L, Covelli E, Romeo M, Filippi C, Monini S (2019) Complications after round window vibroplasty. Eur Arch Otorhinolaryngol 276(6):1601–1605
Barbara M, Filippi C, Covelli E, Volpini L, Monini S (2018) Ten years of active middle ear implantation for sensorineural hearing loss. Acta Otolaryngol 138(9):807–814
Funding
No funding or financial interests to the Authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barbara, M., Covelli, E., Filippi, C. et al. Revision of active middle ear implants (AMEI): causes, surgical issues and rehabilitative transition at a single implanting center. Eur Arch Otorhinolaryngol 278, 4289–4294 (2021). https://doi.org/10.1007/s00405-020-06565-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06565-9