Abstract
Purpose
To determine the efficacy and safety of the intratympanic infiltration of infliximab at the hearing threshold of patients in follow-up for refractory immune-mediated hearing loss.
Methods
17 patients were collected with relapses, despite maintenance treatment with oral azathioprine associated or not with oral prednisone at low doses (between 5 and 7.5 ml/day) or refractory relapses to previous intratympanic corticoid treatment being 19 affected ears infiltrated. We measured the hearing threshold by Pure-Tone Average (PTA) 500–3000 Hz, 125–8000 Hz and 250–8000 Hz in pre-infiltration (baseline) and follow-up 3 weeks post-infiltration with auditory threshold at frequencies 125–8000 Hz.
Results
The average age was 50.68 years (±15.23 years). After the administration of intratympanic infliximab, an improvement of the hearing threshold was showed in the Pure-Tone Average (PTA) calculated at 500–3000 Hz (p = 0.004), 125–8000 Hz (p = 0.001) and 250–8000 Hz (p = 0.006). An immediate improvement in low frequencies also was observed: 125, 250 and 500 Hz (p = 0.009, p = 0.002 and p < 0.001 respectively) also at 1000 Hz (p = 0.004) and a persistence of the effect at 3 months in the low frequencies: 125 Hz (p = 0.020), 250 Hz (p = 0.006) and 500 Hz (p = 0.002).
Conclusions
Infliximab intratympanic infiltration improves the hearing threshold in patients with immune-mediated hearing loss. The effect of improving the hearing threshold is higher in low frequencies and persists within 3 months of the infiltration. The administration of intratympanic infliximab is an effective and safe technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rapidly progressive or fluctuating hearing loss accounts for less than 1% of hearing loss [1]. It is estimated that the immune-mediated hearing loss affects 5 of every 100,000 patients/year; therefore, it is considering a rare disease [2].
The interest of this type of sensorineural hearing loss lies in its response to medical treatment. Two clinical characteristics are those that mark the type of treatment to follow in the immune-mediated hearing loss: relapses and chronicity. Relapses require acute treatment to recover the auditory threshold [3] and chronicity requires a maintenance treatment that delays the hearing impairment and decreases the relapse frequencies [4, 5].
Tumour Necrosis Factor Alpha (TNF-α) is an early mediator [6] and key in the cochlear damage present in the immune-mediated hearing loss [7]. Cochlear damage induces an early expression of proinflammatory cytokines in cochlear macrophages [8], fibrocytes of the spiral ligament [9], stria vascularis cells and spiral ganglion neurons, including interleukins (IL) such as IL-1 β, IL-6 and TNF-α [10]. Anti-TNF drugs [11] are used to modulate the local inflammatory response by reducing the release of proinflammatory cytokines and secondary cochlear damage [12,13,14].
Infliximab is a monoclonal antibody chimeric (mouse/human) that, unlike the etanercept can join the receptor and lead to apoptosis of activated lymphocytes [15].
Currently, the intratympanic pathway is used for the administration of corticoid as a rescue treatment for sudden deafness [16] and gentamicin for crisis control in Meniere's disease [17]. The incorporation into the clinical practice of intratympanic biological therapy administered daily is a recent fact.
Despite the valuable information offered by experimental studies, animal models are not extrapolated to humans, hence the relevance of the results obtained in clinical studies, showing that the transtympanic administration of infliximab allows the withdrawal of prednisone and reduces the number of relapses in patients with immune-mediated hearing loss [18].
The aim of the study was to determine the efficacy and safety of the intratympanic infiltration of infliximab (ITII) in the hearing threshold of patients in follow-up for immune-mediated hearing loss.
Methods
Study design
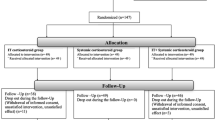
Prospective longitudinal case series.
Participants
Seventeen patients diagnosed with immune-mediated hearing loss were selected and monitored in consultation from April 2012 to October 2018 and showed refractory relapses of the auditory threshold. 19 ears were treated, due 2 patients presented 2 relapses treated with ITII.
Patients with relapse were included despite treatment of maintenance with oral azathioprine (AZA) associated or not with oral prednisone at low doses (between 5 and 7.5 mg/day) and patients with relapses refractory to previous intratympanic corticoid infiltration without treatment at the time of relapse.
A decrease in the hearing threshold of 10 dB in two consecutive frequencies or 15 dB in a single frequency was considered relapse.
The type of refractory hearing loss to diagnosis was specified:
• High Rapidly Progressive (HRP), if hearing threshold deterioration occurred in less than 3 months.
• Fluctuating Hypoacusis (FH), if the fluctuation was found in 3 hearing tests in less than 12 months.
• Sudden Repeat Deafness (SRD), if the patient presented more than 3 episodes.
Informed consent was obtained from all individual participants included in the study. The authors declare that they have complied with the requirements established by the Declaration of Helsinki for Human Research of 1974 (last modified in 2000).
Variables
Demographic variables were taken from the study patients; age, sex, infiltrated ear, diagnosis, base treatment with AZA and systemic disease. Hearing threshold by Pure-Tone Average (PTA) 500–3000 Hz, 125–8000 Hz and 250–8000 Hz in pre-infiltration (baseline) and follow-up 3 weeks post-infiltration. Auditory threshold at frequencies 125 Hz, 250 Hz, 500 Hz, 1000 Hz, 2000 Hz, 4000 Hz and 8000 Hz before infiltration (baseline), 3 weeks after infiltration and follow-up 3 months post-treatment.
Procedure
The preparation of intratympanic infliximab was performed in the pharmacy service, reconstituting a 100 mg of infliximab vial with 10 mL of API (Application Programming Interface) in a 1 mL syringe, bagged and labelled with the consideration of cytostatic sanitary residue effects.
Intratympanic infiltration was performed on an outpatient basis. The patient was placed in supine decubitus with head rotated to the contralateral side. With microscopic control and the help of a speculum, the tympanic membrane was inspected. As a topical anaesthetic, a drop of phenol was used at 88% placed in posteroinferior quadrant using a small-calibre ear aspiration terminal. A long lumbar puncture needle (22G/90 mm) is docked to the 1 ml syringe, with angle to allow local infiltration. 0.3 mL (3 mg) were administered in each infiltration, programming four consecutive doses (one weekly). Patients remained in supine decubitus for 10 min, avoiding phonation and swallowing during this time.
A tonal audiometry was performed with Interacoustic AD33 equipment (Fisher Sacchi, S.A. Medical France) before starting treatment, 3 weeks after the last infiltration and 3 months follow-up. The audiometry was performed in the Otolaryngology consultation by nurses under the supervision of the principal investigator. The hearing threshold was recorded in dB at different frequencies: 125, 250, 500, 1000, 2000, 4000 and 8000 Hz. The PTA was calculated on each audiometric control for different frequencies: 500–3000 Hz, 125–8000 Hz and 250–8000 Hz.
Statistical analysis
The SPSS 21.0® for Windows package was used (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp).
Qualitative variables were expressed in frequencies and as many percent and quantitative variables in mean and standard deviation.
Paired t test was performed to compare PTA and improvement of hearing thresholds before and after Infliximab infiltration for the patients treated in baseline measurements, 3 weeks and 3 months follow-up.
Significance was determined to be at the confidence level of p < 0.05.
Results
64.7% of the patients were males. The average age was 50.68 years (± 15.23). 88.2% presented specific organ disease. 5.8% presented fluctuating hearing loss (one patient), 47.1% progressive (eight patients) and 47.1% more than three episodes of sudden deafness (eight patients). Two patients had systemic disease (Panarteritis Nodosa (PAN) and Graves’ disease).
The clinical characteristics of the 17 patients included in the study: age, sex, demographic variables (Table 1) together with the diagnostic details and hearing threshold of the 19 study cases (Table 2).
A pre-and post-treatment analytical study was conducted: prior to infiltration (baseline) and 3 weeks (post-treatment) with PTA data (Table 3).
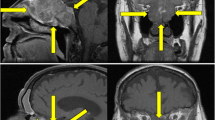
Results found after ITII showed an improvement in hearing threshold, with statistically significant differences in PTA 500–3000 Hz (p = 0.004), 125–8000 Hz (p = 0.001) and 250–8000 Hz (p = 0.006) (Table 4 and Fig. 1).
The differences between the auditory thresholds in each frequency before the infiltration were studied, 3 weeks to 3 months post-infiltration to check infliximab effect. Results showed statistically significant differences with improvement of auditory thresholds after ITII, being the effect of the drug greater than 3 weeks of infiltration than 3 months follow-up. A persistence of the effect was observed at 3 months in the low frequencies (125 Hz (p = 0.020), 250 Hz (p = 0.006) and 500 Hz (p = 0.002) and an immediate improvement in 125, 250 and 500 Hz (p = 0.009, p = 0.002 and p < 0.001 respectively) and also in 1000 Hz (p = 0.004) (Table 5 and Fig. 2).
Data from measurements in 125–250–500 Hz of patients treated with AZA were compared with patients without AZA treatment and no statistically significant differences were found at 125 Hz at 3 weeks (p = 0.884) and 3 months (p = 0.447), 250 Hz at 3 weeks (p = 0.205) and 3 months (p = 0.246) and 500 Hz at 3 weeks (p = 0.488) and 3 months (p = 0.549).
Discussion
In the study development centre, the diagnosis of immune-mediated hearing loss is based on the response of the hearing threshold to corticosteroid treatment at full doses (Prednisone 1 mg/Kg/day) and long guideline (15 days) [19]. In case of relapse, treatment with oral prednisone (1 mg/Kg/day for 7 days) is established if the disease is bilateral or intratympanic corticoids are indicated [20], in case of unilateral affectation (40 mg of Methylprednisolone 3 doses, 1 weekly). As base treatment, AZA was used as a single therapy or associated with low-dose oral corticosteroids (5–7.5 mg/day). Therefore, it is considered relapse an episode of sudden deafness in the context of a chronic disease.
In this study, intratympanic infliximab was used as a rescue therapy in case of refractory relapse without response to oral or intratympanic corticoids. The protocol described by Van Wijk was used [18] with the intention of reducing the number of relapses and/or allowing the dose of oral corticosteroids to be suspended in patients with immune-mediated hearing loss. In this work, infliximab is administered by a local release device placed in the round window (Silverstein MicroWickTM). Van Wijk study treated nine patients with immune-mediated hearing loss and compared two groups: a group of five patients who do not manage to lower the dose of oral corticosteroids and another group of four patients, without oral corticoid treatment that have a relapse. The hearing threshold is assessed by calculating the PTA 250–8000 Hz before and after treatment. In four of five corticoid-dependent patients is corroborated a decrease in the dose of prednisone until its suspension without hearing loss. In the other group, the PTA improves in three of four patients (22.6 ± 15.7 dB) and reduces the total number of recurrences in seven of nine patients. In the present study, with double the sample presented by Van Wijk, but without dividing the patients into two groups, an improvement of the PTA 250–8000 Hz was found that was maintained at 3 months of ITII in 15 of 17 patients (88.2% of cases). These data are like those shown by Van Wijk reporting an improvement of the PTA 250–8000 Hz in seven of the nine cases (77.7%), although the follow-up period is not 3 months in all cases, varying between 10 and 38 weeks.
Van Wijk's study finds a statistically significant decrease in the hearing threshold per month of follow-up (p < 0.001) for the hearing threshold at the end of follow-up (2.4–4.3 months). These data are corroborated by those presented in this work, since it was found that the hearing threshold improved statistically at 3 weeks of the infiltration, with the difference that this improvement was found only in low frequencies (125–500 Hz) and in the conversational frequency of 1000 Hz. In addition, this improvement of the hearing threshold was maintained at 3 months post-infiltrate, results that improve the evidence previously presented by Van Wijk [18].
The improvement of the hearing threshold in the low frequencies coincides with the results found by the author in the treatment of maintenance of the hearing loss immune-mediated with AZA suggesting a greater effect at the level of the basal turns of the cochlea [21]. The influence of AZA was not found as a base treatment in the improvement of hearing at low frequencies compared to patients without base treatment, which reinforces the direct effect of ITII in these frequencies.
The main limitation of the study is the small sample size achieved (17 patients), due to the low incidence of the disease. Similar limitations are found in other studies, like Ghossaini [22] with intratympanic Golimumab with ten patients and less follow-up (42 days/1.3 months), hearing threshold stabilization is reported in 60% of patients and a worsening of 40%. PTA 250–8000 Hz is compared at baseline and 42 days of follow-up. In this study, it is also considered worsening auditory a lowering of the hearing threshold of 15 dB in a single frequency or 10 dB in two consecutive frequencies, which makes the results comparable.
Another bias could be the dose given to patients. To date, no study has allowed the proper dosage of infliximab to be determined to achieve maximum effectiveness. It is known that the bioavailability of drugs after intratympanic injection is low [23]. It has been estimated that only 2.5% of the applied gentamicin reaches the basal cochlea [24]. This study followed the multiple injections protocol to achieve higher levels of local concentration and higher concentrations in the upper area of the cochlea.
The doses reported in Van Wijk's study have been used. Perhaps higher doses or booster doses may influence the long-term hearing threshold, as suggested studies in animals with noise-induced cochlear damage in which dose-dependent therapeutic effects have been described using peptide inhibitors of transforming Growth Factor Beta 1 (TGF-β1) to improve pathological changes in the cochlea [25].
The study also showed that intratympanic administration of anti-TNF is safe, as reported in clinical practice in the works of Van Wijk [18] and Ghossaini [22] and the animal model by other authors, with etanercept [26] and recently with another immunosuppressant, methotrexate [27].
In none of the patients studied, local inflammation or tympanic residual perforation was observed.
Longer term studies would allow to determine whether the ITII has changed the course of the immune-mediated disease, determining the average time of audiometric relapse-free survival of these patients and compared with previous studies of the author showing a mean relapse time of 9.70 months (± 1.03) in patients treated with AZA versus patients exclusively treated with corticoids (5.25 months; ± 0.76) [28].
The work presented is the first to demonstrate that intratympanic infliximab infiltration with standard technique, without placing any release device on the round window, improves the hearing threshold after treatment.
The advantages of the intratympanic technique are: (1) standard technique accepted in the usual practice that can be performed in the consultation, (2) reduction of costs in fungible material (release devices) and (3) reduction of expenses attributable to surgical procedures.
Implications and future direction
The future goes through the development of new methods of instillation, for example, gelatine hydrogel for the administration of Insulin-Like Growth Factor (IGF1) with a demonstrated role in sudden deafness resistant to corticoids [29, 30], the use of nanoparticles of PLGA (Polylactic/glycolic acid) for the release of drugs in the cochlea [31], both by direct injection on the tympanic ramp and by the application on the round and oval window [32] or use of viral vectors to get a vector distribution throughout the cochlea [33].
Better results are expected with the investigation of new therapies in this area that answer questions about the limitations founded in dosage and management techniques. In this way, at study centre, other biological therapies are being monitored systemically (Infliximab, Rituximab, Anakinra) to assess the long-term effect of these treatments on the maintenance of the hearing threshold in patients with immune-mediated hearing loss.
Conclusions
ITII improves the hearing threshold in patients with immune-mediated hearing loss and is an alternative for the treatment of relapse in refractory disease. The effects of improving the hearing threshold is maintained at 3 months of treatment and is higher in low frequencies. ITII is a safe technique. More studies are needed to determine the dose and number of appropriate infiltrations to achieve maximum effects.
References
Chau JK, Cho JJ, Fritz DK (2012) Evidence-based practice: management of adult sensorineural hearing loss. Otolaryngol Clin North Am 45:941–958
Vambutas A, Pathak S (2016) AAO: Autoimmune and Autoinflammatory (Disease) in Otology: What is New in Immune-Mediated Hearing Loss. Laryngoscope Investig Otolaryngol 1:110–115
Garcia-Berrocal JR, Ibanez A, Rodriguez A, Gonzalez-Garcia JA, Verdaguer JM, Trinidad A, Ramirez-Camacho R (2006) Alternatives to systemic steroid therapy for refractory immune-mediated inner ear disease: a physiopathologic approach. Eur Arch Otorhinolaryngol 263:977–982
Rahman MU, Poe DS, Choi HK (2001) Autoimmune vestibulo-cochlear disorders. Curr Opin Rheumatol 13:184–189
Lobo D, Garcia-Berrocal JR, Trinidad A, Verdaguer JM, Ramirez-Camacho R (2013) Review of the biologic agents used for immune-mediated inner ear disease. Acta Otorrinolaringol Esp 64:223–229
Demirhan E, Eskut NP, Zorlu Y, Cukurova I, Tuna G, Kirkali FG (2013) Blood levels of TNF-alpha, IL-10, and IL-12 in idiopathic sudden sensorineural hearing loss. Laryngoscope 123:1778–1781
Satoh H, Firestein GS, Billings PB, Harris JP, Keithley EM (2003) Proinflammatory cytokine expression in the endolymphatic sac during inner ear inflammation. J Assoc Res Otolaryngol 4:139–147
Fujioka M, Okano H, Ogawa K (2014) Inflammatory and immune responses in the cochlea: potential therapeutic targets for sensorineural hearing loss. Front Pharmacol 5:287
Yoshida K, Ichimiya I, Suzuki M, Mogi G (1999) Effect of proinflammatory cytokines on cultured spiral ligament fibrocytes. Hear Res 137:155–159
Okano T (2014) Immune system of the inner ear as a novel therapeutic target for sensorineural hearing loss. Front Pharmacol 5:205
Monaco C, Nanchahal J, Taylor P, Feldmann M (2015) Anti-TNF therapy: past, present and future. Int Immunol 27:55–62
Hess A, Bloch W, Huverstuhl J, Su J, Stennert E, Addicks K, Michel O (1999) Expression of inducible nitric oxide synthase (iNOS/NOS II) in the cochlea of guinea pigs after intratympanical endotoxin-treatment. Brain Res 830:113–122
Warchol ME (1999) Immune cytokines and dexamethasone influence sensory regeneration in the avian vestibular periphery. J Neurocytol 28:889–900
Warchol ME, Kaplan BA (1999) Macrophage secretory products influence the survival of statoacoustic neurons. NeuroReport 10:665–668
Van den Brande JM, Braat H, van den Brink GR, Versteeg HH, Bauer CA, Hoedemaeker I, van Montfrans C, Hommes DW, Peppelenbosch MP, van Deventer SJ (2003) Infliximab but not etanercept induces apoptosis in lamina propria T-lymphocytes from patients with Crohn's disease. Gastroenterology 124:1774–1785
Lavigne P, Lavigne F, Saliba I (2016) Intratympanic corticosteroids injections: a systematic review of literature. Eur Arch Otorhinolaryngol 273:2271–2278
Huon LK, Fang TY, Wang PC (2012) Outcomes of intratympanic gentamicin injection to treat Meniere's disease. Otol Neurotol 33:706–714
Van Wijk F, Staecker H, Keithley E, Lefebvre PP (2006) Local perfusion of the tumor necrosis factor alpha blocker infliximab to the inner ear improves autoimmune neurosensory hearing loss. Audiol Neurootol 11:357–365
Harris JP, Weisman MH, Derebery JM, Espeland MA, Gantz BJ, Gulya AJ, Hammerschlag PE, Hannley M, Hughes GB, Moscicki R, Nelson RA, Niparko JK, Rauch SD, Telian SA, Brookhouser PE (2003) Treatment of corticosteroid-responsive autoimmune inner ear disease with methotrexate: a randomized controlled trial. JAMA 290:1875–1883
Hamid M, Trune D (2008) Issues, indications, and controversies regarding intratympanic steroid perfusion. Curr Opin Otolaryngol Head Neck Surg 16:434–440
Mata-Castro N, Gavilanes-Plasencia J, Ramirez-Camacho R, Garcia-Fernandez A, Garcia-Berrocal JR (2018) Azathioprine reduces the risk of audiometric relapse in immune-mediated hearing loss. Acta Otorrinolaringol Esp 69:260–267
Ghossaini SN, Liu JP, Phillips B (2013) Round window membrane permeability to golimumab in guinea pigs: a pilot study. Laryngoscope 123:2840–2844
Salt AN, Plontke SK (2018) Pharmacokinetic principles in the inner ear: Influence of drug properties on intratympanic applications. Hear Res 368:28–40
Plontke SK, Biegner T, Kammerer B, Delabar U, Salt AN (2008) Dexamethasone concentration gradients along scala tympani after application to the round window membrane. Otol Neurotol 29:401–406
Sanz L, Murillo-Cuesta S, Cobo P, Cediel-Algovia R, Contreras J, Rivera T, Varela-Nieto I, Avendano C (2015) Swept-sine noise-induced damage as a hearing loss model for preclinical assays. Front Aging Neurosci 7:7
Wang X, Truong T, Billings PB, Harris JP, Keithley EM (2003) Blockage of immune-mediated inner ear damage by etanercept. Otol Neurotol 24:52–57
Eren SB, Dogan R, Yenigun A, Veyseller B, Tugrul S, Ozturan O, Aydin MS (2017) Evaluation of ototoxicity of intratympanic administration of Methotrexate in rats. Int J Pediatr Otorhinolaryngol 100:132–136
Mata-Castro N, Garcia-Chilleron R, Gavilanes-Plasencia J, Ramirez-Camacho R, Garcia-Fernandez A, Garcia-Berrocal JR (2018) Analysis of audiometric relapse-free survival in patients with immune-mediated hearing loss exclusively treated with corticosteroids. Acta Otorrinolaringol Esp 69:214–218
Lee KY, Nakagawa T, Okano T, Hori R, Ono K, Tabata Y, Lee SH, Ito J (2007) Novel therapy for hearing loss: delivery of insulin-like growth factor 1 to the cochlea using gelatin hydrogel. Otol Neurotol 28:976–981
Yamamoto N, Nakagawa T, Ito J (2014) Application of insulin-like growth factor-1 in the treatment of inner ear disorders. Front Pharmacol 5:208
Martin-Saldana S, Palao-Suay R, Aguilar MR, Ramirez-Camacho R, San Roman J (2017) Polymeric nanoparticles loaded with dexamethasone or alpha-tocopheryl succinate to prevent cisplatin-induced ototoxicity. Acta Biomater 53:199–210
Murillo-Cuesta S, Garcia-Alcantara F, Vacas E, Sistiaga JA, Camarero G, Varela-Nieto I, Rivera T (2009) Direct drug application to the round window: a comparative study of ototoxicity in rats. Otolaryngol Head Neck Surg 141:584–590
Staecker H, Brough DE, Praetorius M, Baker K (2004) Drug delivery to the inner ear using gene therapy. Otolaryngol Clin North Am 37:1091–1108
Acknowledgements
The authors acknowledge support of physicians and nurses of the Otolaryngology and Rheumatology services of Torrejón Hospital that have collaborated in the attention of the patients of the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NMC designed and carried out the study, analysed data and wrote the paper; NMC and LSV designed and performed experiments at the centre in Spain; NMC and LSV collected and analysed data from the centre; NMC, DVD and AGF provided statistical analysis and critical revision. All authors contributed equally to this work. NMC, DVD and AGF reviewed data from all sites and provided interpretive analysis; NMC, LSV and AGF wrote the main paper. All authors discussed the results and implications and commented on the manuscript at all stages.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Hospital research committee (Torrejón Hospital research committee INF-HUT-2019) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mata-Castro, N., Sanz-López, L., Varillas-Delgado, D. et al. Intratympanic infliximab is a safe and effective rescue therapy for refractory immune-mediated hearing loss. Eur Arch Otorhinolaryngol 277, 393–400 (2020). https://doi.org/10.1007/s00405-019-05716-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05716-x