Abstract
The objective of this study is to compare the outcomes of transaxillary gasless endoscopic thyroidectomy (TGET) and conventional open thyroidectomy (COT). Thirty-three patients with thyroid nodule were enrolled. All patients were randomized into two different groups. Sixteen patients underwent TGET and 17 patients underwent COT. We analyzed the patients’ characteristics, wound satisfaction, the intraoperative phase, hospitalization, pain, and costs. The operative time for the TGET group was significantly longer than in the COT group. The estimated blood loss, the hospitalized days, and pain between the two groups were not significantly different. The drainage content was significantly more in the TGET group. The patients’ wound satisfaction and mean total cost per case were significantly greater in the TGET group. The TGET provided better cosmetic outcomes and was comparable regarding the estimated blood loss, pain, complication, and hospitalization. However, the TGET required a longer operative time which determines the higher costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traditionally, surgeons are familiar with open thyroid surgery. Conventional open thyroidectomy (COT) is performed through a transverse cervical incision, leaving a scar on the anterior neck in a cosmetically unfavorable site. The easily visible scar can cause a negative impact to the patient’s confidence. Unfortunately most thyroid disease occurs in women who are rather concerned with a good looking image. Therefore, surgeons have developed the surgical techniques of thyroidectomy to achieve better cosmetic results.
Endoscopic thyroid surgery currently becomes an attractive choice of the patients who need thyroid surgery. An excellent cosmetic result is the main advantage of this procedure.
Advancement in endoscopic technology has emphasized emerging various surgical techniques. Gasless endoscopic thyroidectomy using a transaxillary approach, developed and adopted by the surgeons from Department of Surgery, Yonsei University College of Medicine, Seoul, Korea, is one of the most popular methods of endoscopic thyroid surgery [1, 2]. Transaxillary gasless endoscopic thyroidectomy (TGET) is reproducible and provides satisfied cosmetic results [3–5].
So far, many comparative studies between open and endoscopic thyroid surgery has been carried out. However, these studies are lacking of randomization and in economic outlook. The objective of the study is to compare TGET and COT in the comprehensive perspective including intraoperative phase, hospitalization, pain, wound satisfaction, and costs analysis.
Patients and methods
The Ethic Committee at Faculty of Medicine, Prince of Songkla University approved the study protocol. The reference number of the study approval was EC54-193-13-1-3.
Patients
During April 2011 to January 2013, 33 patients with thyroid nodule were enrolled. All patients were randomized into two different groups by a computer generated table. Sixteen patients underwent TGET and 17 patients underwent COT at the Songklanagarind hospital, a university hospital of Prince of Songkla University. All patients were between 18 and 70 years old. The thyroid nodule did not exceed 4 cm in size, as measured by ultrasonography and had fine needle aspiration biopsy (FNAB) results proved it as benign, follicular lesion, or undiagnostic smear. The exclusion criteria included: BMI over 30 kg/m2, thickness of skin and subcutaneous tissue of the neck and chest over 2 cm, FNAB results suspected malignancy, evidence of extracapsular invasion or distant metastasis, previously irradiated at neck or axilla, and contraindicating thyroid surgery or general anesthesia. Informed consent was obtained from each patient.
The TGET group patients were operated on by one surgeon (KJ). The COT group patients were operated or under supervised by KJ or faculties. Postoperative management was administrated along with the standard of care. The same regimen of postoperative pain control was prescribed for both groups. The pain controlling regimen was as follows; during the first day post operative, the patients got Morphine 3 mg intravenous and Acetaminophen 500 mg oral every 4 h, if the patient’s Visual Analog Scale (VAS) was more than 6, Morphine 1 mg intravenous was additionally given every 2 h; after the first day post operative, Acetaminophen 500 mg oral was given every 4 h, if the patient’s VAS was more than 6, Morphine 3 mg intravenous was given every 4 h.
Patients’ demographic data and characteristics of the thyroid nodule were recorded. Intraoperative profiles were analyzed in terms of operative time, intraoperative complication, and blood loss. Postoperative period data was also analyzed with regards to hospital stay days, amount of drainage content, postoperative complication, pain score, dose of pain controller, and wound satisfaction at 6 months’ follow-up. Costs of treatment were analyzed with regards to operative room cost, hospitalized cost, and medication cost.
Operative method
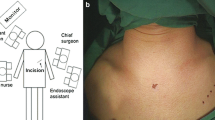
TGET
The patient was set in a supine position after general anesthesia. A thin sponge roll was placed under the shoulder in order to slightly extend the neck. The lesion-side arm was 120° flexed and 90 degree internal rotated to expose the axilla and then retained to a transverse bar attached with an operative table. A 3 cm length incision was made just behind to the anterior axillary fold. This incision was for the Tebbetts retractor to maintain the working space during the operation. A flexible tip endoscope also accessed into the route. Dissection between the pectoralis major muscle and anterior chest subcutaneous soft tissue in a direction toward the anterior neck was performed with an electrocautery. Once there was access to the neck, the sternocleidomastoid muscle (SCM) and the strap muscles were identified. The medial border of SCM and lateral border of the strap muscles were separated. The strap muscles were elevated, and then the Tebbetts retractor was inserted through the incision and placed beneath to the straps muscle. The retractor was lifted up and suspended to expose thyroid gland and to maintain a working space. Two 0.5-cm-sized incisions were made posterior to both ends of the first incision for endoscopic instrument port insertion. Under endoscopic visualization, the surface of thyroid gland was dissected from the surrounding soft tissue using the fine dissector and the grasping forceps. The superior thyroid vessels were identified and carefully controlled close to the thyroid capsule with the Harmonic Scalpel (Johnson & Johnson Medical, Cincinnati, OH, USA). The superior parathyroid gland located near the superior pole was identified and preserved. The middle thyroid vein was identified and divided with the Harmonic Scalpel. The recurrent laryngeal nerve (RLN) was carefully dissected and separated from the inferior thyroid vessels. The Harmonic Scalpel was used for controlling the inferior thyroid arteries and veins as close to the thyroid capsule as possible. The RLN was carefully dissected along its path until reaching to the cricothyroid junction. The inferior parathyroid gland located nearby the inferior pole was identified and preserved as well. The thyroid gland was mobilized and dissected from the trachea. Isthmusectomy was performed with the Harmonic Scalpel. The resected thyroid gland was removed out through the same route. A Radivac drain was inserted through the lower instrument port incision. All surgical wounds were closed layer by layer.
COT
The patient was set in a supine position with neck extension after general anesthesia done. A transverse collar skin incision was made in the midline of the anterior neck in a natural skin crease around 2 cm above the sternal notch. The incision was made through the skin, subcutaneous fat, and platysma. Subplatysmal flap dissection was performed from the sterna notch to the level of the hyoid bone superiorly. The median raphe was identified and the strap muscles were separated laterally to expose the thyroid gland. The superior thyroid vessels were dissected and ligated. The recurrent laryngeal nerve and parathyroid glands were identified and preserved. The thyroid gland was medially mobilized and then isthmusectomy was done. A Radivac drain was placed. The wound was closed layer by layer.
Results
Patient characteristics
Thirty-three patients were recruited to the study. Sixteen patients underwent TGET and 17 patients underwent COT. The clinicopathologic characteristics of the patients are shown in Table 1. There was no statistically significant difference between TGET and COT groups in terms of demographic data, body mass index (BMI), thyroid lesion, and pathologic results.
Intraoperative period (Table 2)
The operative time for the TGET group was significantly longer than in the COT group (297.5 ± 56.2 vs. 156.2 ± 26.9; P < 0.001). The estimated blood loss between two groups was not significantly different. A case of the TGET group was converted to the conventional open surgery regarding of excessive bleeding.
Postoperative period
The complications occurring in the study, such as vocal cord paresis and seroma, were not significantly different between the two groups. The drainage content was significantly more in the TGET group. The patients in both groups were not significantly different regarding the hospitalized days. The patients’ wound satisfaction was significantly greater in the TGET group at 6 months postoperative, although it was not significantly different in the early postoperative period (Table 3).
Regarding pain between the TGET and COT groups, there was no statistically significant difference of VAS at 6 and 48 h but the VAS of the TGET group was significant higher at 24 h (P = 0.006) (Fig. 1). The amount of breakthrough pain medication was not significantly different between the two groups.
Cost analysis (Table 4)
Mean total cost of the TGET and COT group were 940 and 454$ per case, respectively. Subgroup analysis showed the significantly higher operative room cost in the TGET but the hospitalization and medication costs were not different in both groups.
Discussion
At present, minimally invasive surgery plays a role in many fields of surgery. In thyroid surgery, endoscopic technique is becoming more popular with the advantage of attractive cosmetic results. The new technique of thyroid surgery has been compared with the conventional standard in many literatures; however, they are still lacking of randomization. Our comparative study was prospectively conducted with randomization. Without the selection bias the study results emphasized the advantages and disadvantages of each surgical technique.
In the intraoperative phase, the operative time of TGET was significantly longer than the COT (297.5 ± 56.2 vs. 156.2 ± 26.9) as other studies have reported a longer operative time in the endoscopic group [6–13]. More complicated instrument preparation, increased dissection extent, and surgeons’ learning curve are the substantial time consuming factors for TGET. Basically most surgeons and nurses, who are involved in thyroid surgery, are initially trained for the open technique. Therefore, the COT is carried through in a shorter time as it is a familiar procedure. A study of the learning curve for endoscopic thyroidectomy reported that the first 60 cases constitute the early stage of the learning curve and the proficiency and stability of the operation reach the advanced level after 150 cases [14, 15]. Thus, the author and associates are considered in the early stage of the learning curve. In terms of the estimated blood loss, there was no statistically significant difference in both groups but TGET tended to have more blood loss. This finding would result of the relatively more dissected area from axilla to the thyroid gland compared to direct neck access of COT.
In the postoperative phase, the thyroidectomy related complications were not significantly different between the two groups as other literature published [6, 13, 16]. The drainage content was significantly more in the TGET (82.7 ± 23.3 vs. 26.5 ± 21.6). The amount of drainage content was depended on the extent of dissected tissue which was more in TGET. Regarding pain in the early postoperative phase, there was no statistically significant difference of VAS at 6 and 48 h, although the VAS after 6 h postoperative tended to be more in the TGET group. These findings were the results of a greater area of dissected tissue and the prolonged retaining time of the Tabett retractor for the TGET. However, the hospitalizations of both groups were not different as previous literatures reported [1, 7, 9, 11].
In terms of wound satisfaction, the VAS was significantly greater in the TGET group at 6 months post surgery, whereas it was not significantly different in the early postoperative period. This finding states the cosmetic advantage of TGET over COT as the previous literatures published the superior cosmetic results in the various endoscopic approaches [2, 5, 7, 8, 10, 17–19]. The study period of wound satisfaction lasted for 6 months; however, surgical scars continue to mature for many months. The appropriate timing to evaluate the wound satisfaction should be further investigated, regarding the different satisfactions by time.
Considering the costs of treatment, the previous literature reported that video-endoscopic thyroid surgery increased costs of treatment [12, 20]. Our study result demonstrated correspondingly that the mean total cost of the TGET was significantly higher than the COT group. In subcategory analysis, the operative room cost was the only influencing factor to determine the total cost of the operation, while medication and hospitalized costs were not. The most likely explanation could be the direct correlation between operative time and cost, which was obviously more in the TGET group. In addition, the video-endoscopic and hemostat equipments for TGET were included in the costs of the operation. The costs of TGET would decline if the endoscopic thyroid surgeon surpasses the learning curve and carries out the operation in a shorter time.
Although, the study was conducted under a randomized controlled approach, our data had limitations associated with a number of uncontrolled factors. The surgeon and associate variations influence the intraoperative outcomes notably. Even though, the operations were either operated by the author, or supervised by the author or the same institute faculties, who were standardized for the procedure, the varying people and circumstances would determine the study results. Regarding of cosmetic outcome evaluation, surgical wound healing takes a minimum of 6 months and occasionally up to 2 years to become fully settled. The study period of wound satisfaction lasted for 6 months that is the beginning stage of scar maturation. A longer period of time is needed to evaluate the long term cosmetic outcomes, as they may change over time. Drain placement for thyroid surgery is a debatable issue among surgeons in common practice. Some surgeons, who do not use drains for thyroid lobectomy, consider that it might improve cosmetic outcome, and has a bearing on the duration of hospital stay as well as the requirements for pain relief. In the study groups, the drain was placed, for all cases, as indicated in the institute procedure protocol. This would have some effects to the results of cosmetic, hospitalized days, and pain scores.
In the place of study, the costs of the operation were charged with reference to the standard rates of the government university hospital, which directly relies on the resources consumed. Whereas the health care reimbursement refers to the Thai diagnostic related group (DRG) fee that subsidizes a same rate for either a traditional thyroidectomy or thyroidectomy with any technology. The difference between actual expended costs and reimbursements results in a negative financial balance to the hospital and will be even worse if robotic surgery takes place in the near future. The proper rates of reimbursement should be revised to be proportionate with the expenses of innovative surgery.
Conclusions
Comparing to COT, TGET provides better cosmetic outcomes and is comparable of estimated blood loss, pain, complication, and hospitalization. TGET spends more in operative time which determines the higher total costs of treatment.
References
Yoon JH, Park CH, Chung WY (2006) Gasless endoscopic thyroidectomy via an axillary approach: experience of 30 cases. Surg Laparosc Endosc Percutan Tech 16(4):226–231
Kang S-W, Jeong JJ, Yun J-S, Sung TY, Lee SC, Lee YS, Nam K-H, Chang HS, Chun WY, Park CS (2009) Gasless endoscopic thyroidectomy using trans–axillary approach; surgical outcome of 581 patients. Endocr J 56(3):361–369
Bhargav PRK, Kumbhar US, Satyam G, Gayathri KB (2013) Gasless single incision trans-axillary thyroidectomy: the feasibility and safety of a hypo-morbid endoscopic thyroidectomy technique. J Minim Access Surg. 9(3):116–121
HakimDarail NA, Lee SH, Kang S-W, Jeong JJ, Nam K-H, Chung WY (2014) Gasless transaxillary endoscopic thyroidectomy: a decade on. Surg Laparosc Endosc Percutan Tech 00(00):1–5
Ji YB, Song CM, Bang HS, Lee SH, Park YS, Tae K (2014) Long-term cosmetic outcomes after robotic/endoscopic thyroidectomy by a gasless unilateral axillo-breast or axillary approach. J Laparoendosc Adv Surg Tech A. 24(4):248–253
Yoon JH, Park CH, Chung WY (2006) Gasless endoscopic thyroidectomy via an axillary approach: experience of 30 cases. Surg Laparosc Endosc Percutan Tech 16(4):226–231
Lee H, Lee J, Sung KY (2012) Comparative study comparing endoscopic thyroidectomy using the axillary approach and open thyroidectomy for papillary thyroid microcarcinoma. World J Surg Oncol 10(1):269
Cao F, Xie B, Cui B, Xu D (2011) Endoscopic vs. conventional thyroidectomy for the treatment of benign thyroid tumors: a retrospective study of a 4-year experience. Exp Ther Med 2(4):661–666
Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, Nam K-H, Chang HS, Chung WY, Park CS (2009) Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol 100(6):477–480
Miccoli P, Berti P, Raffaelli M, Materazzi G, Baldacci S, Rossi G (2001) Comparison between minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery 130(6):1039–1043
Chung YS, Choe J-H, Kang K-H, Kim SW, Chung K-W, Park KS, Han W, Noh D-Y, Oh SK, Youn Y-K (2007) Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg 31(12):2302–2306 discussion 2307–8
Cabot JC, Lee CR, Brunaud L, Kleiman DA, Chung WY, Fahey TJ, Zarnegar R (2012) Robotic and endoscopic transaxillary thyroidectomies may be cost prohibitive when compared to standard cervical thyroidectomy: a cost analysis. Surgery 152(6):1016–1024
Liu J, Song T, Xu M (2012) Minimally invasive video-assisted versus conventional open thyroidectomy: a systematic review of available data. Surg Today 42(9):848–856
Liu S, Qiu M, Jiang DZ, Zheng XM, Zhang W, Shen HL, Shan CX (2009) The learning curve for endoscopic thyroidectomy: a single surgeon’s experience. Surg Endosc Other Interv Tech 23:1802–1806
Kwak HY, Kim SH, Chae BJ, Song BJ, Jung SS, Bae JS (2014) Learning curve for gasless endoscopic thyroidectomy using the trans-axillary approach: cUSUM analysis of a single surgeon’s experience. Int J Surg. 12(12):1273–1277
Bokor T, Kiffner E, Kotrikova B, Billmann F (2012) Cosmesis and body image after minimally invasive or open thyroid surgery. World J Surg 36(6):1279–1285
Ikeda Y, Takami H, Sasaki Y, Takayama J, Niimi M, Kan S (2002) Comparative study of thyroidectomies. Endoscopic surgery versus conventional open surgery. Surg Endosc 16(12):1741–1745
Tan CTK, Cheah WK, Delbridge L (2008) “Scarless” (in the neck) endoscopic thyroidectomy (SET): an evidence-based review of published techniques. World J Surg 32:1349–1357
Duncan TD, Rashid Q, Speights F, Ejeh I (2009) Transaxillary endoscopic thyroidectomy: an alternative to traditional open thyroidectomy. J Natl Med Assoc 101:783–787
Dhiman SV, Inabnet WB (2008) Minimally invasive surgery for thyroid diseases and thyroid cancer. J Surg Oncol 97(8):665–668
Acknowledgments
We thank Nannapat Pruphetkeaw who performed the statistical analysis of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethic Committee at Faculty of Medicine, Prince of Songkla University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Jantharapattana, K., Maethasith, J. Transaxillary gasless endoscopic thyroidectomy versus conventional open thyroidectomy: a randomized study. Eur Arch Otorhinolaryngol 274, 495–500 (2017). https://doi.org/10.1007/s00405-016-4242-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4242-8