Abstract
Confocal laser endomicroscopy (CLE) is an imaging technique that uses miniaturized fiberoptic probes to allow real-time histological imaging of human tissue. An application of CLE in otorhinolaryngology has hardly been investigated so far. In our study, we analyzed the applicability of CLE to visualize cancerous and healthy tissue of the head and neck region. Formalin-fixed tissue specimens from 135 head and neck squamous cell carcinoma (HNSCC) patients and 50 healthy controls were investigated using CLE with and without topical application of acriflavine. Four head and neck surgeons, four pathologists, and four laymen evaluated the CLE images of the HNSCC cases regarding the tumor localization and its border to healthy tissue. The tumor localization and the tumor border were correctly identified in 97 % by the pathologists, 85 % by the head and neck surgeons, and 70 % by the laymen. The main difference in evaluation results was seen in the correct identification of the tumor site (p < 0.05), while there was no significant difference in the identification of the tumor border. CLE is a valuable tool for real-time histological imaging of HNSCCs. It can help to visualize the tumor border and, thereby, facilitate a more precise tumor surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Head and neck squamous cell carcinomas (HNSCCs) belong to the six most common cancers worldwide and account for approximately 5 % of all human malignancies [1]. In the majority of cases, the patients are treated with a surgical tumor resection. Depending on the stage of disease and the general condition of the patient, surgical treatment is followed by radiation, chemoradiation or radiotherapy combined with the anti-EGFR antibody cetuximab [2]. Thereby, a complete resection of the tumor is essential for the patients’ prognosis [3] and is usually controlled intraoperatively by rapid section histology. However, this technique implies a delay of the surgical procedure and necessitates an additional resection of tissue to achieve a histological verification of tumor-free resection margins.
Confocal laser endomicroscopy (CLE) is an imaging technique that can provide so-called “optical biopsies”, i.e., microscopic information of tissue in real-time with a resolution down to 1 μm and a 1000-fold magnification. CLE uses a combination of confocal microscopy technique and the detection of tissue fluorescence using a laser excitation source [4]. In surgery as well as endoscopic examinations, the microscope can thus be brought into the patient using a rigid or flexible laser light probe instead of bringing the patient‘s tissue to the microscope. First studies highlighted the potential benefit of CLE for noninvasive real-time histological imaging in gastroenterology [5–11], gynecology [12, 13], urology [14, 15], pneumology [16–18], and neurosurgery [19, 20]. However, there are only a few studies comprising small numbers of patients in the field of head and neck surgery [21, 22]. White et al. first described in 1999 the application of CLE in the head and neck region of 6 healthy controls and described its morphological correlations with corresponding H&E stained tissue sections [23]. This first description of CLE imaging of the head and neck region was followed by several in vitro [24–28] and in vivo studies [29–40] focusing on the noninvasive detection of HNSCCs using CLE [40]. While, in some of these studies, the tissue autofluorescence seemed to be sufficient to provide valuable CLE images [23–25, 27, 29, 33, 35, 37, 38], an improvement of tissue contrast was reported in other studies using topically or systemically applied fluorescent dyes as acriflavine, fluorescein, 5-aminolaevulinic acid, proflavine or hypericin [26, 28, 30–32, 34, 36, 38, 40]. However, all of these studies mainly addressed the applicability of CLE for the real-time imaging of the tumor’s histoarchitecture in comparison with healthy tissue of the head and neck region. No study has investigated so far if CLE can also be used to visualize the border between cancerous and adjacent healthy tissue, which would be highly beneficial in head and neck cancer surgery. Also, all mentioned studies are limited to a comparably small number of patients with a patient number of less than 50.
In this study, we investigated on 185 tissue samples from 135 HNSCC patients and 5ß healthy controls (1) if CLE can be used to visualize the histological structures of healthy and cancerous tissue of the head and neck region, (2) if the topical application of acriflavine can improve the tissue contrast, and (3) if CLE can be applied to visualize the tumor margins of HNSCCs to adjacent healthy tissue.
Materials and methods
Tissue samples and study design
Formalin-fixed tissue samples from 135 HNSCC patients and 50 healthy control patients were investigated in this study. The clinical diagnoses in the HNSCC group were laryngeal cancer (n = 26), tonsil cancer (n = 26), tongue base cancer (n = 24), hypopharyngeal cancer (n = 15), tongue cancer (n = 10), cancer of the soft palate (n = 8), cancer of the pharyngeal wall (n = 7), cancer of the floor of the mouth (n = 6), cancer of the buccal mucosa (n = 3), and nasopharyngeal cancer (n = 1). The samples from the healthy control group comprised tissue of the nasal respiratory mucosa (n = 12), tonsil (n = 8), thyroid gland (n = 7), parotid gland (n = 6), lymph nodes (n = 3), skeletal muscle of the soft palate (n = 3), mucosa of the lip (n = 2), buccal mucosa (n = 2), parathyroid gland (n = 1), and elastic cartilage from the ear (n = 1). The local Medical Association ethics review committee approved the scientific use of the patients’ tissue and clinical data (index number 207/10). The study has been performed in compliance with the Helsinki Declaration and its later amendments. Written informed consent was obtained from all patients.
Confocal laser endomicroscopy
All 185 FFPE tissue samples were investigated with confocal laser endomicroscopy using the Cellvizio® system (Mauna Kea Technologies, Paris, France; cost: 140,000 € for the analysis system). All investigated tissue samples were already taken before during surgical procedures. Thereby, an ultrahigh-definition probe (Cellvizio® Gastro Flex; Mauna Kea Technologies, Paris, France; tip diameter 2.7 mm, length 3 m, resolution 3.5 μm, field of view of 600 μm, depth 100 μm; 5000 € per probe) was gently moved over the tissue surface of the ex vivo samples with slight pressure providing short movies with a temporal resolution of 12 frames per second. To analyze a potential improvement of tissue contrast using fluorescent dyes, all 185 tissue specimens were investigated with CLE with and without topical application of acriflavine hydrochloride 0.05 % (Sigma Aldrich, Melbourne, Australia). Acriflavine was dropped on the tissue surface following a rinse with lactated Ringer‘s solution after an incubation time of 10 s and an immediate investigation with CLE. For 20 selected cases (15 HNSCC cases and 5 control cases), fresh-frozen specimens were investigated with CLE as well and compared with the CLE images from the corresponding FFPE samples to evaluate the effect of formalin fixation on CLE imaging quality. In this study, microprobes were not used to identify tumor margins in vivo.
As every microprobe can be used 20 times, the cost per patient/tissue sample CLE analysis is about 250 € (apart from the acquisition cost).
Evaluation of CLE images
Following CLE imaging, representative images from the movies of the 135 HNSCC cases were chosen that illustrate the tumor tissue and its border to adjacent healthy structures. These images were evaluated by four head and neck cancer surgeons with only marginal experience in histomorphology, four pathologists with large experience in histomorphology and four laymen without any experience in histomorphology. The laymen group consisted of four university graduates without any medical education. Before starting the evaluation, all examiners were introduced into the morphological characteristics of CLE imaging using a uniform series of CLE images and the corresponding H&E stained tissue sections from 12 keratinizing and 12 nonkeratinizing HNSCC cases as well as 12 healthy control cases. The evaluation itself then consisted in marking the tumor site with a star and drawing a line at the supposed border between cancerous and healthy tissue (see Fig. 6). The evaluation of the 135 HNSCC cases was performed immediately after the training procedure. As gold standard for defining the tumor margin in the investigated tissue samples, H&E stained sections of the respective FFPE tissue were made, and the tumor border and the tumor localization were marked by a pathologist who was not involved in the evaluation of the CLE images.
Histological analysis
For morphological control, the tissue samples were paraffin-embedded, cut into 5 μm sections and H&E stained using a standard protocol. For taking photographs, the Nikon Eclipse TE2000-S inverted microscope, the Nikon Digital Sight DS-5Mc camera, and the NIS-Elements AR software version 3.0 (Nikon; Tokyo, Japan) were used.
Statistical analysis
For statistical analysis, a Kruskal–Wallis test was used applying the commercially available software Statistical Package for the Social Sciences v. 17.0 (IBM, Chicago, IL, USA), XLStat Pro (Addinsoft, New York, NY, USA) and GraphPad Prism (GraphPad Software Inc., La Jolla, CA, USA). p values < 0.05 were considered statistically significant (α = 0.05). In the figures, statistically significant results are marked with *(p ≤ 0.05), **(p ≤ 0.01) or ***(p ≤ 0.001). Statistically nonsignificant results are marked with “ns”.
Results
Visualization of healthy tissue of the head and neck region
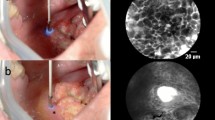
First, we investigated formalin-fixed tissue specimens of the head and neck region taken from 50 patients without a head and neck tumor. Thereby, even detailed histolomorphological structures as skeletal muscle fibers, adipose tissue, collagen fibers, and lymphoid tissue could be visualized down to the cellular level (see Fig. 1). Collagen fibers, the elastic internal membrane of vessels and lymphocytes showed the highest intensity of autofluorescence, whereas for nonkeratinizing squamous epithelium, gland tissue, and peripheral nerves, a much weaker fluorescence signal was detected.
Visualization of head and neck squamous cell carcinomas
Also, formalin-fixed tissue samples from 135 HNSCC patients were investigated with CLE seeking to visualize the tumor morphology as well as the border between the tumor and adjacent healthy tissue (see Fig. 2). With CLE, we could reliably differentiate keratinizing from nonkeratinizing tumors, as keratinizing tumors showed not only a higher intensity of autofluorescence but also, in most cases, the characteristic formation of keratin pearls. However, we found that a keratinizing surface of the tumor interfered with imaging quality in some cases of extensively keratinizing growth pattern with a keratin surface thicker than 50 μm leading to a slightly reduced resolution of CLE images taken from deeper structures. However, the quality of the images was still high enough to allow the identification of cellular structures and to differentiate tumor tissue from adjacent healthy tissue.
To exclude that the process of formaldehyde fixation substantially altered the autofluorescence of the tissue detected with CLE, we compared the CLE images of fresh-frozen tissue, formalin-fixed tissue, and formalin-fixed, paraffin-embedded tissue from the same patient for 15 representative HNSCC cases and five healthy control cases. Thereby, only marginal differences were seen when comparing the CLE images with a minimally weaker tissue contrast in native tissue due to a slightly decreased range of brightness as compared with FFPE tissue (see Fig. 3), though histomorphological structures could as easily been differentiated in the CLE images of native tissue as in the CLE images of FFPE tissue.
CLE images are shown for native (fresh frozen, left column), formalin-fixed (middle column), and formalin-fixed paraffin embedded tissue (right column) from skeletal muscle of the soft palate (a), a keratinizing (b), and a nonkeratinizing squamous cell carcinoma (c). CLE images are shown in ×40 magnification
Identification of tumor localization and tumor margins
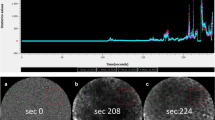
In the next step, the CLE images from all 135 HNSCC cases were evaluated by four head and neck surgeons with only marginal experience in histomorphology, four pathologists with wide experience in histomorphology, and four laymen without any experience in histomorphology. In detail, the examiners had to manually draw a line in the CLE images where they would suppose the border between the tumor and adjacent healthy tissue and to mark the tumor site with a star (see Fig. 4). Before starting the evaluation, all examiners were introduced into the morphological characteristics of CLE imaging using a uniform series of CLE images and images from corresponding H&E stained tissue sections for 12 keratinizing and 12 nonkeratinizing HNSCC cases as well as 12 healthy control cases.
Evaluation results of CLE images are shown for head and neck surgeons (left column), pathologists (middle column), and laymen (right column) regarding a correct localization of the tumor and its margins (a), a wrong localization of the tumor (b), a wrong localization of the tumor margins (c), and a wrong localization of the tumor site and margins (d). The error bars indicate the standard deviation
After this initial training in CLE morphology, a correct marking of the tumor border and the tumor localization was achieved in 97 % of cases by the pathologists, in 85 % of cases by the head and neck surgeons and in 70 % of cases by the laymen (see Fig. 5). While there was no significant difference between the three groups regarding the correct identification of the tumor border, we found highly significant differences in the right localization of the tumor site with the best result for the pathologists, followed by the head and neck surgeons and the laymen. Thereby, a correct marking of the tumor border as well as the tumor localization was achieved in 97 % of cases by the pathologists, in 85 % by the head and neck surgeons, and in 70 % by the laymen (see Fig. 5).
CLE images are shown for interstitial connective tissue with collagen fibers (a), a small vessel (b), skeletal muscle of the soft palate (c) and a nonkeratinizing HNSCC (d) with (right column) and without topical application of acriflavine (left column). All images were taken from FFPE tissue samples and are shown in ×40 magnification
Comparison of autofluorescence and acriflavine staining
As in many studies, a topical application of acriflavine was recommended to achieve an improvement of tissue contrast, and we repeated the CLE analysis for all 185 formalin-fixed tissue samples with an additional topical application of acriflavine before starting the measurement with the CLE probe. Herein, the topical application of acriflavine did not substantially improve the visualization of histomorphological structures of healthy or cancerous tissue. As acriflavine predominately stains the nuclei of the cells, we found a suppression of the autofluorescence of collagen fibers (see Fig. 6a, d) and the elastic internal membrane of vessels (see Fig. 6b). In contrast, the nuclei of fibrocytes and tumor cells showed a much stronger fluorescent signal (see Fig. 6b, d).
Discussion
Head and neck squamous cell carcinomas represent 5 % of all human cancers worldwide with an incidence of 350,000 new cases each year [1, 41–43]. For the majority of patients, surgery is the treatment of choice and followed by an adjuvant treatment including radiation, radiochemotherapy or radioimmunotherapy where necessary. Thereby, a complete resection of the tumor (R0) is essential for therapeutic success and crucially influences the patients’ prognosis [3]. As rapid section histology engages some time until the result is available and necessitates an additional resection of tissue, CLE is a promising technique to overcome these challenges and allow an intraoperative noninvasive real-time histological imaging [21, 22]. In our study, we investigated the applicability of CLE for the imaging of healthy and cancerous tissue of the head and neck region with an emphasis on the visualization of the tumor margins.
First, we investigated healthy and cancerous tissue of the head and neck region and compared the quality of CLE images with corresponding H&E stained tissue slides. Thereby, we could show that CLE can visualize histomorphological characteristics of head and neck tissue with a high quality and a resolution down to the cellular level without any need for a topical pretreatment of the tissue with fluorophores. In contrast to these findings, many other studies recommended the use of topically or systemically applied fluorescent dyes to improve tissue contrast [26, 28, 30–32, 34, 36, 38, 40]. Thereby, most authors prefer a topical application of acriflavine or a topical or systemic application of fluorescein. However, one has to consider that systemically or topically applied fluorescein is neither approved by the Food and Drug Administration (FDA) nor the European Medicines Agency (EMA) for a use apart from diagnostic angiography and angioscopy of the retina and iris vasculature [6], though the risks seem to be low [6, 44]. For acriflavine, mutagenic effects have been reported [45]. Because of the lacking admission by the approval agencies, the potential risks for the patients’ health, and the only marginal improvement of tissue contrast, we do not advise to use any fluorescent dyes for CLE imaging of the head and neck region in vivo.
Following the analysis of all 185 FFPE tissue samples with CLE, representative images from the recorded CLE files were selected and evaluated by four head and neck surgeons, four pathologists, and four laymen regarding the tumor localization and the tumor margins. Thereby, the pathologists reached the highest rate of correct classification, followed by the head and neck surgeons and the laymen. Certainly, these evaluation results cannot be generalized due to the limited number of examiners and the different experience in histomorphology between and inside the groups of evaluators, though it is obvious that pathologists also generally show the widest experience in evaluating histological images, and thus should have the highest chance for a correct interpretation of CLE videos or images. As, in our study, the relatively small number of 36 CLE images that was used for the initial training in CLE morphology was sufficient even for the laymen to reach a rate of correct classification in 70 %, it seems to be realistic that additional training could shorten the gap between head and neck surgeons and pathologists.
One limitation of this study is that we had to restrict our examinations to formalin-fixed tissue samples due to the missing applicability of fresh-frozen tissue for all included patients. This limits the transferability of our results to the intraoperative situation due to the different constitution and molecular tissue structure caused by formaldehyde-induced protein and DNA crosslinking and the resulting change of tissue autofluorescence. However, we have shown that there are only marginal differences in CLE morphology mainly regarding the range of brightness when comparing fresh-frozen and formalin-fixed tissue from the same patients (see Fig. 3) without any difference in the resolution of the CLE images. Accordingly, we assume that our results on ex vivo specimens are largely transferable to an in vivo situation.
Beneath, as the images for the evaluation were taken from recorded video frames, there is a potential selection bias. Thus, it cannot be excluded that the evaluation results based on the selected images differ from an evaluation of the whole frames as they would be used in the operating room. To show that also in an in vivo situation, the probe can not only image the tumor border at different portions of the tumor but also feasibly follow along the surface of tissue to define a surgical margin, we added an exemplary video showing this tracking of the tumor border along the tissue surface with CLE as supplementary material (Video S1).
When considering a transfer of CLE imaging to the operating room as a tool to visualize tumor tissue and its margins, one has to consider that the correct interpretation of CLE images needs some experience in histomorphology. As shown in our study, head and neck surgeons themselves will probably not be able to identify the tumor site and its margins with a sufficient reliability to guarantee tumor-free resection borders. Consequently, the knowledge of a pathologist would be needed for the correct interpretation of CLE images. One possibility to overcome this challenge could be a direct transfer of the intraoperatively gained CLE data using a wireless network to the pathologist who can than advise the surgeon how to proceed. Thus, head and neck surgeon and pathologist could discuss CLE images during the operation to spare time and functionally important tissue. Another potential application of CLE in the future could be to analyze the expression of molecular biomarkers by the tumor cells in real time as first studies have shown that antibody-linked fluorophores can specifically be detected with CLE in vivo [9, 10].
However, one has to consider the technical limitations when applying CLE for the intraoperative identification of tumor margins. Due to the limited depth of view of approximately 60 μm, tumors that show a predominately submucosal growth pattern could be missed. Furthermore, the presence of mucus, bleedings or coagulated areas could impair CLE imaging in an intraoperative situation [35]. Beneath that, one has to consider that so far there exists no CLE microprobe specifically designed for an intraoperative use in the head and neck region with tumors often located at awkward areas, e.g., the tongue base. However, the Cellvizio® GastroFlex™ microprobe that was used in our study is very flexible with a small diameter of only 2.7 mm and should, therefore, maneuverable enough to get to any localization of the upper aerodigestive tract. Furthermore, there are nine further kinds of CLE microprobes available with a variable tip diameter, length, resolution, field of view, and depth (Table S1), so that depending on the anatomical localization and the diagnostic requirements, the technical specifications can be adapted, though an in vivo study will be needed to investigate if CLE is an appropriate technique to visualize the localization and margins of HNSCCs in the intraoperative situation.
Conclusion
Taken together, our study has shown that CLE constitutes an easily applicable technique for noninvasive real-time histological imaging of healthy and cancerous tissue of the head and neck region at a cellular level and that the border between the tumor and healthy tissue as well as the localization of the tumor can reliably be identified by physicians with increasing success depending on their experience in histomorphology. Hence, CLE imaging is a promising tool for head and neck cancer surgery obtaining real-time optical biopsies and has the potential to improve the quality of surgical treatment.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Marur S, Forastiere AA (2008) Head and neck cancer: changing epidemiology, diagnosis, and treatment. Mayo Clin Proc 83:489–501
Chiesa F, Mauri S, Tradati N, Calabrese L, Giugliano G, Ansarin M, Andrle J, Zurrida S, Orecchia R, Scully C (1999) Surfing prognostic factors in head and neck cancer at the millenium. Oral Oncol 35:590–596
Goetz M (2012) Confocal Laser Endomicroscopy: Applications in clinical and translational science—a comprehensive review. ISRN Pathol. doi:10.5402/2012/387145
Wallace MB, Sharma P, Lightdale C, Wolfsen H, Coron E, Buchner A, Bajbouj M, Bansal A, Rastogi A, Abrams J, Crook JE, Meining A (2010) Preliminary accuracy and interobserver agreement for the detection of intraepithelial neoplasia in Barrett’s esophagus with probe-based confocal laser endomicroscopy. Gastrointest Endosc 72:19–24
Wallace MB, Meining A, Canto MI, Fockens P, Miehlke S, Roesch T, Lightdale CJ, Pohl H, Carr-Locke D, Löhr M, Coron E, Filoche B, Giovannini M, Moreau J, Schmidt C, Kiesslich R (2010) The safety of intravenous fluorescein for confocal laser endomicroscopy in the gastrointestinal tract. Aliment Pharmacol Ther 31:548–552
Polglase AL, McLaren WJ, Skinner SA, Kiesslich R, Neurath MF, Delaney PM (2005) A fluorescence confocal endomicroscope for in vivo microscopy of the upper- and the lower-GI tract. Gastrointest Endosc 62:686–695
Kiesslich R, Burg J, Vieth M, Gnaendiger J, Enders M, Delaney P, Polglase A, McLaren W, Janeli D, Thomas S, Nafe B, Galle PR, Neurath MF (2004) Confocal laser endoscopy for diagnosing intraepithelial neoplasias and colorectal cancer in vivo. Gastroenterology 127:706–713
Goetz M, Ziebart A, Foersch S, Vieth M, Waldner MJ, Delaney P, Galle PR, Neurath MF, Kiesslich R (2010) In vivo molecular imaging of colorectal cancer with confocal endomicroscopy by targeting epidermal growth factor receptor. Gastroenterology 138:435–446
Foersch S, Kiesslich R, Waldner MJ, Delaney P, Galle PR, Neurath MF, Goetz M (2010) Molecular imaging of VEGF in gastrointestinal cancer in vivo using confocal laser endomicroscopy. Gut 59:1046–1055
Meining A, Saur D, Bajbouj M, Becker V, Peltier E, Höfler H, von Weyhern CH, Schmid RM, Prinz C (2007) In vivo histopathology for detection of gastrointestinal neoplasia with a portable, confocal miniprobe: an examiner blinded analysis. Clin Gastroenterol Hepatol 5:1261–1267
Carlson K, Pavlova I, Collier T, Descour M, Follen M, Richards-Kortum R (2005) Confocal microscopy: imaging cervical precancerous lesions. Gynecol Oncol 99(3 Suppl 1):S84–S88
Tan J, Quinn MA, Pyman JM, Delaney PM, McLaren WJ (2009) Detection of cervical intraepithelial neoplasia in vivo using confocal endomicroscopy. BJOG 116:1663–1670
Wiesner C, Jäger W, Salzer A, Biesterfeld S, Kiesslich R, Hampel C, Thüroff JW, Goetz M (2011) Confocal laser endomicroscopy for the diagnosis of urothelial bladder neoplasia: a technology of the future? BJU Int 107:399–403
Sonn GA, Jones SN, Tarin TV, Du CB, Mach KE, Jensen KC, Kiao JC (2009) Optical biopsy of human bladder neoplasia with in vivo confocal laser endomicroscopy. J Urol 128:1299–1305
Fuchs FS, Zirlik S, Hildner K, Schubert J, Vieth M, Neurath MF (2013) Confocal laser endomicroscopy for diagnosing lung cancer in vivo. Eur Respir J 41:1401–1408
Lane PM, Lam S, McWilliams A, Leriche JC, Anderson MW, Macaulay CE (2009) Confocal fluorescence microendoscopy of bronchial epithelium. J Biomed Opt. doi:10.1117/1.3103583
Thiberville L, Moreno-Swirc S, Vercauteren T, Peltier E, Cavé C, Bourg Heckly G (2007) In vivo imaging of the bronchial wall microstructure using fibered confocal fluorescence microscopy. Am J Respir Crit Care Med 175:22–31
Snuderl M, Wirth D, Sheth SA, Bourne SK, Kwon CS, Ancukiewicz M, Curry WT, Frosch MP, Yaroslavsky AN (2013) Dye-enhanced multimodal confocal imaging as a novel approach to intraoperative diagnosis of brain tumors. Brain Pathol 23:73–81
Charalampaki P, Javed M, Daali S, Heiroth HJ, Igressa A, Weber F (2015) Confocal laser endomicroscopy for real-time histomorphological diagnosis: our clinical experience with 150 brain and spinal tumor cases. Clin Neurosurg 62(Suppl 1):171–176
Abbaci M, Breuskin I, Casiraghi O, De Leeuw F, Ferchiou M, Temam S, Laplace-Builhé C (2014) Confocal laser endomicroscopy for non-invasive head and neck cancer imaging: a comprehensive review. Oral Oncol 50:711–716
Volgger V, Conderman C, Betz CS (2013) Confocal laser endomicroscopy in head and neck cancer: steps forward? Curr Opin Otolaryngol Head Neck Surg 21:164–170
White WM, Rajadhyaksha M, González S, Fabian RL, Anderson RR (1999) Noninvasive imaging of human oral mucosa in vivo by confocal reflectance microscopy. Laryngoscope 109:1709–1717
Clark AL, Gillenwater AM, Collier TG, Alizadeh-Naderi R, El-Naggar AK, Richards-Kortum RR (2003) Confocal microscopy for real-time detection of oral cavity neoplasia. Clin Cancer Res 9:4714–4721
Just T, Stave J, Boltze C, Wree A, Kramp B, Guthoff RF, Pau HW (2006) Laser scanning microscopy of the human larynx mucosa: a preliminary, ex vivo study. Laryngoscope 116:1136–1141
Abbaci M, Temam S, Casiraghi O, Vielh P, Bosq J, Fouret P, Laplace-Builhé C (2009) Characterization of laryngeal carcinoma by confocal endomicroscopy. Head Neck Oncol 1(Suppl 1):O14. doi:10.1186/1758-3284-1-S1-O14
Muldoon TJ, Roblyer D, Williams MD, Stepanek VM, Richards-Kortum R, Gillenwater AM (2012) Noninvasive imaging of oral neoplasia with a high-resolution fiber-optic microendoscope. Head Neck 34:305–312
Vila PM, Park CW, Pierce MC, Goldstein GH, Levy L, Gurudutt VV, Polydorides AD, Godbold JH, Teng MS, Genden EM, Miles BA, Anandasabapathy S, Gillenwater AM, Richards-Kortum R, Sikora AG (2012) Discrimination of benign and neoplastic mucosa with a high-resolution microendoscope (HRME) in head and neck cancer. Ann Surg Oncol 19:3534–3539
Farahati B, Stachs O, Prall F, Stave J, Guthoff R, Pau HW, Just T (2010) Rigid confocal endoscopy for in vivo imaging of experimental oral squamous intraepithelial lesions. J Oral Pathol Med 39:318–327
Zheng W, Harris M, Kho KW, Thong PS, Hibbs A, Olivo M, Soo KC (2004) Confocal endomicroscopic imaging of normal and neoplastic human tongue tissue using ALA-induced-PPIX fluorescence: a preliminary study. Oncol Rep 12:397–401
Thong PS, Kho KW, Zheng W, Harris M, Soo KC, Olivo M (2007) Development of a laser confocal endomicroscope for in vivo fluorescence imaging. J Mech Med Biol. doi:10.1142/S0219519407002108
Thong PS, Olivo M, Kho KW, Zheng W, Mancer K, Harris M, Soo KC (2007) Laser confocal endomicroscopy as a novel technique for fluorescence diagnostic imaging of the oral cavity. J Biomed Opt 12:014007
Maitland KC, Gillenwater AM, Williams MD, El-Naggar AK, Descour MR, Richards-Kortum RR (2008) In vivo imaging of oral neoplasia using a miniaturized fiber optic confocal reflectance microscope. Oral Oncol 44:1059–1066
Haxel BR, Goetz M, Kiesslich R, Gosepath J (2010) Confocal endomicroscopy: a novel application for imaging of oral and oropharyngeal mucosa in human. Eur Arch Otorhinolaryngol 267:443–448
Pogorzelski B, Hanenkamp U, Goetz M, Kiesslich R, Gosepath J (2012) Systematic intraoperative application of confocal endomicroscopy for early detection and resection of squamous cell carcinoma of the head and neck: a preliminary report. Arch Otolaryngol Head Neck Surg 138:404–411
Thong PS, Tandjung SS, Movania MM, Chiew WM, Olivo M, Bhuvaneswari R, Seah HS, Lin F, Qian K, Soo KC (2012) Toward real-time virtual biopsy of oral lesions using confocal laser endomicroscopy interfaced with embedded computing. J Biomed Opt. doi:10.1117/1.JBO.17.5.056009
Pierce MC, Schwarz RA, Bhattar VS, Mondrik S, Williams MD, Lee JJ, Richards-Kortum R, Gillenwater AM (2012) Accuracy of in vivo multimodal optical imaging for detection of oral neoplasia. Cancer Prev Res (Phila) 5:801–809
Just T, Pau HW (2013) Intra-operative application of confocal endomicroscopy using a rigid endoscope. J Laryngol Otol 127:599–604
Contaldo M, Poh CF, Guillaud M, Lucchese A, Rullo R, Lam S, Serpico R, MacAulay CE, Lane PM (2013) Oral mucosa optical biopsy by a novel handheld fluorescent confocal microscope specifically developed: technologic improvements and future prospects. Oral Surg Oral Med Oral Pathol Oral Radiol 116:752–758
Nathan CAO, Kaskas NM, Ma X, Chaudhery S, Lian T, Moore-Medlin T, Shi R, Mehta V (2014) Confocal laser endomicroscopy in the detection of head and neck precancerous lesions. Otolaryngol Head Neck Surg 151:73–80
Cooper JS, Porter K, Mallin K, Hoffman HT, Weber RS, Ang KK, Gay EG, Langer CJ (2009) National cancer database report on cancer of the head and neck: 10-year update. Head Neck 31:748–758
Barnes L, Eveson JW, Reichart P, Sidransky D (2005) Pathology and genetics of head and neck tumors. World Health Organization Classification of Tumors. IARC Press, Lyon
Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB (2003) Cancer incidence in five continents, vol VIII. IARC Press, Lyon
Shahid MW, Crook JE, Meining A, Perchant A, Buchner A, Gomez V, Wallace MB (2011) Exploring the optimal fluorescein dose in probe-based confocal laser endomicroscopy for colonic imaging. Interv Gastroenterol 1:166–171
Burleson GR, Caulfield MJ, Pollard M (1979) Ozonation of mutagenic and carcinogenic polyarmoatic amines and polyaromatic hydrocarbons in water. Cancer Res 39:2149–2154
Acknowledgments
We thank Samira Daali, Mehreen Javed, Ulrike Bechtel and Monika Hoffmann for their excellent technical assistance. This study was supported by a HOMFORexzellent grant to M.L. and by Siemens AG.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
This study was funded by a HOMFOR grant to M.L. and Siemens AG. Both sponsors had no influence on the study design, the collection, analysis and interpretation of data, writing of the report, and the decision to submit the article for publication.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Linxweiler, M., Kadah, B.A., Bozzato, A. et al. Noninvasive histological imaging of head and neck squamous cell carcinomas using confocal laser endomicroscopy. Eur Arch Otorhinolaryngol 273, 4473–4483 (2016). https://doi.org/10.1007/s00405-016-4145-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4145-8