Abstract
Endoscopic base of skull surgery has been growing in acceptance in the recent past due to improvements in visualisation and micro instrumentation as well as the surgical maturing of early endoscopic skull base practitioners. Unfortunately, these demanding procedures have a steep learning curve. A physical simulation that is able to reproduce the complex anatomy of the anterior skull base provides very useful means of learning the necessary skills in a safe and effective environment. This paper aims to assess the ease of learning endoscopic skull base exposure and drilling techniques using an anatomically accurate physical model with a pre-existing pathology (i.e., basilar invagination) created from actual patient data. Five models of a patient with platy-basia and basilar invagination were created from the original MRI and CT imaging data of a patient. The models were used as part of a training workshop for ENT surgeons with varying degrees of experience in endoscopic base of skull surgery, from trainees to experienced consultants. The surgeons were given a list of key steps to achieve in exposing and drilling the skull base using the simulation model. They were then asked to list the level of difficulty of learning these steps using the model. The participants found the models suitable for learning registration, navigation and skull base drilling techniques. All participants also found the deep structures to be accurately represented spatially as confirmed by the navigation system. These models allow structured simulation to be conducted in a workshop environment where surgeons and trainees can practice to perform complex procedures in a controlled fashion under the supervision of experts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of endoscopic techniques in base of skull surgery has been growing in acceptance in the recent past. Progressively more complex procedures are being performed from the anterior base of skull to the craniocervical junction via endoscopic techniques [1–4].
These demanding procedures have a steep learning curve. In addition to the comprehensive knowledge of anatomy in this region, surgeons also have to be conversant with a myriad of instruments such as navigation tools, drills and debriders as well as develop the ability to work within a confined space using all these devices [5, 6].
Endoscopic base of skull procedures are frequently performed as a team comprising an ENT surgeon and a neurosurgeon. The development of surgical skills of these teams usually progress from CSF leak repairs and pituitary surgery to anterior base of skull surgery and finally to procedures involving the clivus, C1 and C2 or extending laterally from the sphenoid [1, 2, 4, 7]. Currently, training and familiarisation remains restricted to either lab-based cadaveric workshops or on the job training during live surgery. Eight simulation-based training offers an attractive and feasible alternative to learning these techniques in a safe and effective way [9–11]. The Accreditation Council for Graduate Medical Education (ACGME) has recently mandated simulation-based training as part of the requirements for general surgical training programmes [12]. In line with this, a number of authors have proposed various simulation models including 3D printed models as a basis for training in a wide range of surgical competencies [13].
The advancing technology of 3D printing has enabled simulation models to be created for complex anatomical pathology with the necessary accuracy, feel and tactile feedback [14]. This paper is an extension from our previously published work on the technical aspects, validity and accuracy of 3D printed models in simulating nasal and skull base anatomy and now being able to use models created in this manner to conduct skills workshops [15, 16].
Basilar invagination is an uncommon condition where the odontoid peg is displaced in a cranial direction into the foramen magnum. This leads to the crowding of structures passing through the foramen causing compression of the lower brain stem or upper cervical spinal cord. In the past this problem was managed microsurgically utilising the transoral route where the anterior margin of the foramen magnum, anterior arch of C1 and odontoid peg was removed. More recently, these procedures are carried out endoscopically via a transnasal route by a team consisting of neurosurgeons and ENT surgeons. The training curve for such procedures is quite steep and thus is a good example of the type of surgical procedure surgeons would benefit from prior model-based training and exposure.
Aiming to achieve this objective, multiple models of a patient with platy-basia and basilar invagination were created from the original MRI and CT imaging data of the patient. The models were used as part of a complex skull base training workshop for ENT surgeons with varying degrees of experience in endoscopic base of skull surgery, from trainees to experienced consultants. The objective of this workshop was to assess the ease of learning endoscopic skull base exposure and drilling techniques using an anatomically accurate physical model with a pre-existing pathology created from actual patient data.
Materials and methods
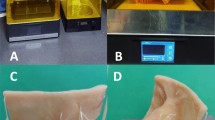
Imaging data (MRI and CT) of a patient with basilar invagination, who was previously operated on, was selected and the various anatomical structures were segmented and converted into STL format using in-house software (BIOMODROID CBMTI UM©). This data was subsequently used to print an actual replica of the head and upper cervical spine using a 3D printer (Stratasys Connex 500 USA®) (Fig. 1).
All models had the nose printed in soft pliable material. The central septum was printed with a central firm core covered by a soft material to mimic the human septum. In keeping with the objective of learning skull base exposure and drilling techniques, the anterior nasal structures were made as simple as possible and the turbinates were not reproduced. On the other hand posteriorly, all structures from the sphenoid keel to the C2–C3 junction was segmented and recreated in an accurate fashion. The “bony” surface was coated with a similar soft pliable material that could be incised and reflected from the underlying “bone” to mimic the mucosa of the posterior naso-pharynx.
Five models were created and each was operated on by teams consisting of three surgeons. Prior to the workshop, the participants were given a comprehensive lecture on the standard endoscopic endonasal approach to access the craniocervical junction as well as to resect the lower third of the clivus, anterior arch of C1 and peg of C2. They were given a list of key steps to achieve and were also asked to list the level of difficulty while learning these steps using the simulated model.
The key steps included:
-
1.
Registration of model and endoscope to the image guidance system.
-
2.
Introduction of the endoscope and identification of the mucosal membrane.
-
3.
Incision of the mucus membrane.
-
4.
Identification of key structure including clivus and anterior arch of C1.
-
5.
Drilling the lower third of the clivus, the anterior arch of C1 and the peg of C2 (Fig. 2a, b).
-
6.
Exposing the dura from the lower clivus to the arch of C2 (Fig. 3a, b).
-
7.
Performing the procedure under image guidance control.
All participants were required to assess the difficulty level of learning these steps using the model based on a 5-point Likert scale.
Results
There were 15 workshop participants, consisting of qualified ENT surgeons from the Asia Pacific region, with an average post-qualification experience of 18.7 years. The surgeons have been exposed to base of skull surgery for an average of 7.5 years each.
The surgeons were divided into groups of 3 to a workstation that consisted of the model as well as an image guidance station (Medtronic S7®), endoscope system (Karl Storz®) and necessary equipment to perform the operation that included drills, debriders and other surgical tools.
The majority of the participants found the models suitable for registration and navigation. All participants also found the deep structures to be accurately represented spatially as confirmed by the navigation system as they went along with the procedures (Table 1).
In the assessment of tissue structure a low mean score of 2.7 was obtained for nasal structures, while transnasal access and handling of mucosal layer including incision received a mean score of 3.3 and 3.1, respectively.
A score of 4.4 was obtained for the use of power tools on the models inclusive of the high speed drill. All other parameters scored a mean of 4.0. The overall score for the model as a mean to simulate advanced endoscopic work on the clivus was 4 out of 5.
Discussion
As operations increase in complexity, the need for suitable simulation becomes more pressing. In the field of base of skull endoscopy, such simulators are scarce [17–19]. Training on cadavers has been the mainstay but as highlighted in previous publications, they lack in pathology and are not readily available around the world [8, 16, 20]. Running suitable training modules is also cost sensitive and utilising cadavers would require the presence of devices that are only used for this singular purpose and cannot be used in patients [21].
Endoscopic skull base training, as mentioned earlier has a long and steep learning curve. The training plan can be divided into three distinct phases. The trainee usually concentrates on learning the basics of endoscopic surgery in Phase 1 by doing anterior nasal procedures such as functional endoscopic sinus surgery (FESS). Once competent, the trainee moves to Phase 2, where the more challenging cases are handled, e.g., endoscopic pituitary surgery and CSF leak repair. Finally, the advanced trainee moves to Phase 3, which involves learning extended anterior skull base endoscopic procedures. The time taken to move from one phase to the next is variable, usually dependent on case volume and exposure. Simulation models may reduce the time taken to gain this experience.
Presently the number of training models in the area of skull base surgery is limited. Phase 1 training involving endoscopic sinus surgery is best simulated on a cadaver. Specialised models like S.I.M.O.N.T (Sinus Model Otorhino Neuro Trainer; Pro Delphus, Recife, Brazil) are relatively rudimentary and suitable for Phase 1 and 2 anterior nasal works but not for the more advanced extended skull base work. It also lacks anatomical pathology [22].
The 3D models described here comes with anatomical pathology incorporated, making training realistic and relevant. The presence of pathology as depicted in a CT or MRI image in the model creates a clear objective of the simulation programme. The presence of the necessary anatomical structures and the management of these structures as they would be handled in actual surgery is the second advantage. Finally the ability of these models to create the necessary tactile feedback together with the required hand eye coordination is an important and valuable feature.
Due to their spatial accuracy, these models allow detailed simulation of an endoscopic skull base surgery from registration of the image guidance system to the complete surgical procedure. This allows surgeons beginning their exposure to these forms of operation to perform an operation uninterrupted. This is in contrast to present training where trainees would have performed the operation under supervision and will often require multiple operations before a single complex procedure such as the above mentioned is completed. On the other hand, surgeons with experience usually perform their first complex procedure on actual patients often relying on their previous experience in managing simpler procedures and prior training on cadavers. Therefore, such a model has the potential to provide both groups with customised simulation of the intended procedure in complete safety prior to performing the actual operation.
Our workshop participants ranged in experience from trainees to experienced consultants. Their overall experience with using the models were very favourable, especially in learning certain crucial steps like image guidance navigation and using power tools for endoscopic drilling. The low scores were limited to anterior nasal anatomy and transnasal access, both of which were not the objective of this model. The general consensus of the participants was that the model was very realistic and useful in learning a complex procedure, in a repetitive fashion with ease and safety. Without doubt, endoscopic surgery, especially when performing complex procedures in the skull base region require good hand eye coordination. This becomes more difficult as these surgeries are performed by teams of surgeons (usually consisting of neurosurgeons and ENT surgeons), therefore multiplying the pair of hands and eyes that need to be coordinated optimally. The use of these models also allows teams of surgeons to work together coordinating their actions as it is a common occurrence in actual surgery.
Limitation
The present drawback with these models is that they lack blood and cerebrospinal fluid that are often important factors that makes surgery vivid and challenging. Second, while these models have the necessary tissue layer and tactile feedback they still do not fully replicate actual tissue.
Conclusion
3D printed models with pathology now allow structured simulation to be conducted in a safe workshop environment where surgeons and trainees can practice performing complex procedures under the supervision of experts.
References
Castelnuovo P, Dallan I, Battaglia P, Bignami M (2010) Endoscopic endonasal skull base surgery: past, present and future. Eur Arch Otorhinolaryngol 267(5):649–663. doi:10.1007/s00405-009-1196-0 Epub 2010 Jan 9
Shin M, Kondo K, Saito N (2012) Neuroendoscopic transnasal surgery for skull base tumors: basic approaches, avoidance of pitfalls, and recent innovations. Neurol Med Chir (Tokyo) 52(10):697–703
Wagenmann M, Schipper J (2011) The transnasal approach to the skull base. From sinus surgery to skull base surgery. GMS Curr Top Otorhinolaryngol Head Neck Surg 10:Doc08. doi:10.3205/cto000081 Epub 2012 Apr 26
Solares CA, Ong YK, Snyderman CH (2010) Transnasal endoscopic skull base surgery: what are the limits? Curr Opin Otolaryngol Head Neck Surg 18(1):1–7. doi:10.1097/MOO.0b013e3283350035
Berhouma M, Baidya NB, Ismaïl AA, Zhang J, Ammirati M (2013) Shortening the learning curve in endoscopic endonasal skull base surgery: a reproducible polymer tumor model for the trans-sphenoidal trans-tubercular approach to retro-infundibular tumors. Clin Neurol Neurosurg 115(9):1635–1641. doi:10.1016/j.clineuro.2013.02.013 Epub 2013 Mar 5
Mori K, Yamamoto T, Oyama K, Ueno H, Nakao Y, Honma K (2008) Modified three-dimensional skull base model with artificial dura mater, cranial nerves, and venous sinuses for training in skull base surgery: technical note. Neurol Med Chir (Tokyo) 48(12):582–587 discussion 587–8
Stamm AC, Pignatari SS, Vellutini E (2006) Transnasal endoscopic surgical approaches to the clivus. Otolaryngol Clin North Am 39(3):639–656 xi
Zuckerman JD, Wise SK, Rogers GA, Senior BA, Schlosser RJ, DelGaudio JM (2009) The utility of cadaver dissection in endoscopic sinus surgery training courses. Am J Rhinol Allergy 23:218–224
Kakizawa Y, Hongo K, Rhoton AL Jr (2007) Construction of a three-dimensional interactive model of the skull base and cranial nerves. Neurosurgery 60:901–910
Ruthenbeck GS, Hobson J, Carney AS, Sloan S, Sacks R, Reynolds KJ (2013) Toward photorealism in endoscopic sinus surgery simulation. Am J Rhinol Allergy 27(2):138–143. doi:10.2500/ajra.2013.27.3861
Malekzadeh S, Pfisterer MJ, Wilson B, Na H, Steehler MK (2011) A novel low-cost sinus surgery task trainer. Otolaryngol Head Neck Surg 145(4):530–533. doi:10.1177/0194599811413373 Epub
Accreditation Council for Graduate Medical Education (ACGME) (2011) Common program requirements. http://www.acgme.org/acgmeweb/Portals/0/dh_dutyhoursCommonPR07012007pdf
McGurk M, Amis AA, Potamianos P, Goodger NM (1997) Rapid prototyping techniques for anatomical modelling in medicine. Ann R Coll Surg Engl 79(3):169–174
Waran V, Devaraj P, Hari Chandran T, Muthusamy KA, Rathinam AK, Balakrishnan YK, Tung TS, Raman R, Rahman ZA (2012) Three-dimensional anatomical accuracy of cranial models created by rapid prototyping techniques validated using a neuronavigation station. J Clin Neurosci 19(4):574–577. doi:10.1016/j.jocn.2011.07.031 Epub 2012 Feb 3
Waran V, Menon R, Pancharatnam D, Rathinam AK, Balakrishnan YK, Tung TS, Raman R, Prepageran N, Chandran H, Rahman ZA (2012) The creation and verification of cranial models using three-dimensional rapid prototyping technology in field of transnasal sphenoid endoscopy. Am J Rhinol Allergy 26(5):e132–e136. doi:10.2500/ajra.2012.26.3808
Waran V, Narayanan V, Karuppiah R, Owen SL, Aziz T (2014) Utility of multimaterial 3D printers in creating models with pathological entities to enhance the training experience of neurosurgeons. J Neurosurg 120(2):489–492. doi:10.3171/2013.11.JNS131066 Epub 2013 Dec 10
Chen G, Ling F (2010) A new plastic model of endoscopic technique training for endonasal transsphenoidal pituitary surgery. Chin Med J (Engl) 123(18):2576–2579
Acar B, Gunbey E, Babademez MA, Karabulut H, Gunbey HP, Karasen RM (2010) Utilization and dissection for endoscopic sinus surgery training in the residency program. J Craniofac Surg 21(6):1715–1718. doi:10.1097/SCS.0b013e3181f3c73b
Wiet GJ, Stredney D, Wan D (2011) Training and simulation in otolaryngology. Otolaryngol Clin North Am 44(6):1333–1350. doi:10.1016/j.otc.2011.08.009 viii–ix
Krisht AF, Yoo K, Arnautovic KI, Al-Mefty O (2005) Cavernous sinus tumor model in the canine: a simulation model for cavernous sinus tumor surgery. Neurosurgery 56(6):1361–1365 discussion 1365–6
Snyderman C, Kassam A, Carrau R, Mintz A, Gardner P, Prevedello DM (2007) Acquisition of surgical skills for endonasal skull base surgery: a training program. Laryngoscope 117(4):699–705
Nogueira JF, Stamm AC, Lyra M, Balieiro FO, Leão FS (2008) Building a real endoscopic sinus and skull-base surgery simulator. Otolaryngol Head Neck Surg 139(5):727–728. doi:10.1016/j.otohns.2008.07.017
Acknowledgments
This work was supported by University of Malaya via the High Impact Research Grant (H-50001-00-A000026) granted to Professor Vicknes Waran. Neither University Malaya nor the grant committee had a direct role in the study design; collection, analysis or interpretation of data; writing of the report; and the decision to submit this paper for publication.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video 1: Demonstration of odontoid drilling in the model (MPG 7596 kb)
Rights and permissions
About this article
Cite this article
Narayanan, V., Narayanan, P., Rajagopalan, R. et al. Endoscopic skull base training using 3D printed models with pre-existing pathology. Eur Arch Otorhinolaryngol 272, 753–757 (2015). https://doi.org/10.1007/s00405-014-3300-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3300-3