Abstract
The Zuckerkandl tubercle is a residue from the embryological development of the thyroid gland. Although it is undeniably well known in surgery, this is not so among otolaryngologists. Our objective is to highlight the importance of the Zuckerkandl tubercle, as it has proven to be a reliable point of reference to locate the upper parathyroid, the lower thyroid artery and the recurrent nerve. In order to study the Zuckerkandl tubercle, we made a prospective analysis of the posterolateral border of the thyroid lobes in 107 thyroidectomies (88 total thyroidectomies and 19 hemithyroidectomies) carried out by the same surgeon; in total, 195 thyroid lobes were analysed. The Zuckerkandl tubercle was certainly detected in 155 thyroid lobes (79.48 %). The Zuckerkandl tubercle was most frequent in the right thyroid lobe (P = 0.06). When the Zuckerkandl tubercle was present, we localised the upper parathyroid due to its relationship with the tubercle in 80 right thyroid lobes (95.23 %) and in 65 left (91.54 %). On 147 occasions (94.83 %), the recurrent nerve was directed towards the cricothyroid membrane beneath the Zuckerkandl tubercle, laterally to the tracheal surface in relation with the Berry ligament. The lower thyroid artery and some of the distal branches, such as the recurrent nerve, also ran under the Zuckerkandl tubercle. The areolar tissue underlying the Zuckerkandl tubercle is difficult to dissect, and so this protuberance constitutes a surgical difficulty but it is fundamentally helpful to find those important structures that must be preserved in thyroid surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Zuckerkandl tubercle (ZT) is a protuberance which arises from the posterolateral border of thyroid lobes (TL). It was described by Madelung [1] in 1879 and by Zuckerkandl [2] in 1902, and this last author named it the processus posterior glandulae thyroideae. In 1919, Dunhill [3] makes reference to the fact that, on the posterolateral border of the TL, a protuberance is frequently found, more or less pedicled, and surrounded by areolar tissue which is difficult to dissect and which it is necessary to enucleate together with the TL, to avoid recurrence of the symptoms which indicated surgery. In 1938, Gilmour [4] described the relationship between the ZT and the upper parathyroid, and the recurrent nerve.
Curiously, this formation, of undoubted anatomosurgical importance, did not attract the attention of head and neck surgeons over the succeeding 50 years. Reeve et al. [5], in his study of 2,052 thyroidectomies carried out between 1975 and 1985, re-established the knowledge of the ZT; and recommended total thyroidectomy instead of the subtotal in vogue at the time, which left the lateral border of TL as a remnant along with the ZT. From there on, publications began to appear referring to the TZ [6–8] and to the difficulties of its location, above all in the multi-nodular goitre [9–12]. We have observed this tubercle in many thyroidectomies, but until we read the work of Gauger et al. [13], we were not aware that this formation had its own ‘personality’ and has been known about since the late 19th century.
Our objective is to highlight the importance of the ZT among head and neck surgeons, since we maintain that it is a reliable reference point in the localisation of the upper parathyroid, the lower thyroid artery and the recurrent nerve. The ZT—even today—is not well known, is passed over, being considered merely an additional formation in the frequently irregular posterolateral outline of the TL. Such that, for example, in two recent essays on thyroid surgery, one concedes considerable surgical importance to the TZ [14], while the other does not even mention it [15].
Materials and methods
In our service, around 100 thyroidectomies are carried out every year, the figure being exactly 111 in 2011.
We designed a prospective/descriptive study of the ZT in 107 successive thyroid surgeries (2009–2011), carried out by the same surgeon. There were 105 patients, 84/105 women (80.00 %) and 21/105 men (20.00 %). The average age was 54 years, ranging between 15 and 84.
The extent of the surgery was decided in ORL—Endocrinology clinical sessions. There were 88/107 total thyroidectomies (82.24 %), and 19/107 hemithyroidectomies (17.75 %). Of the hemithyroidectomies, 11/19 were right and 8/19 left. So we were able to analyse 195 TL, 99 right and 96 left. We only included total thyroidectomies and hemithyroidectomies in the study, excluding operations considered “not new” which had been carried out to complete partial techniques undertaken in other services and that had developed the illness a posteriori in the remaining thyroids.
Our technique is always complete extracapsular dissection of the TL; in our service, we do not carry out subtotal thyroidectomies. The pathological anatomy of the surgical specimen diagnosed the following as the principal illness: Multinodular goitre in 62/105 (59.04 %), Carcinoma in 28/105 (26.66 %) of which 25 were papillary and 3 follicular, Graves-Basedow disease in 7/105 (6.66 %), Adenoma in 5/105 (4.76 %) and Hashimoto’s Thyroiditis in 3/105 (2.85 %). Frequently, carcinomas coexisted in a multinodular goitre. Eight patients, in addition to the principal diagnosis, also suffered from Hashimoto’s Thyroiditis.
In the dissection of the border of the posterolateral of the TL, we observe whether the ZT existed or not. In order to recognise the ZT, both form and position were considered. Palpation helps to differentiate the ZT from a thyroid nodule; the nodules are approximately spherical and have a firmer consistency.
We studied the percentage of cases in which the ZT was certainly detected and when it appeared in the right TL (RTL) and when in the left (LTL). There are cases in which we found formations which “seemed to be” the ZT, but were not so, and in these cases we considered the ZT as doubtful. And so, modifying the Pelizzo et al. [8] classification, we established the following: grade 0 when the ZT was not recognised; grade 1 where, due to minimum size or other circumstance, we were not certain it was ZT (ZT doubtful, excluded from the study); grade 2 the ZT of less than 10 mm axis; grade 3 between 10 and 20 mm; grade 4 greater than 20 mm (Table 1).
In those cases where the ZT was certainly recognised, we noted its relationship with the upper parathyroid gland.
With the external surface of the ZT dissected, we eased it from its distal extremity with Mosquito forceps or hook exteriorising and separating it towards the middle line. This allows us to examine the areolar tissue under the ZT; between this, the Berry ligament and the laryngotracheal axis. Once the dissection is completed, we noted the situation of the thyroid artery and the recurrent nerve in relation to the ZT.
The results were incorporated into the data base. These were obtained from notes made immediately following the operations, measurements of the surgical specimen and photographs of the most significant details. The calculations were made to six decimal places, but only the first two were noted.
Results
Of the 195 TL considered (99/195 RTL and 96/195 LTL), we located the ZT in 155/195 (79.48 %). In the RTL, ZT existed in 84/99 (84.84 %) and in the LTL in 71/96 (73.95 %). We observed that the ZT was detected more frequently in the right side (P = 0.06). The ZT was not detected in 40/195 TL (20.51 %).
We found the upper parathyroid immediately cranial to the ZT in 145/155 cases (93.54 %) (Fig. 1). Separating the sides, with reference to the ZT, we located the upper parathyroid in 80/84 RTL (95.23 %) and in 65/71 LTL (91.54 %).
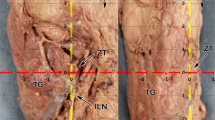
On 147/155 occasions (94.83 %) the recurrent nerve was directed upwards covered by the ZT (Figs. 2, 3); the nerve followed a channel under the ZT and of the mass of the TL and lateral to the surface of the trachea and the Berry ligament. Generally, the lower thyroid artery and some of its branches, in conjunction with the recurrent nerve, also occur below the ZT; although other arterial branches rise across the external surface of the TL and the ZT.
The recurrent nerve was apparent as soon as the ZT is separated on 109/147 occasions (74.14 %): 62/109 times in the RTL (56.88 %) and 47/109 times in the left (43.11 %). It was necessary to dissect the areolar tissue under the ZT to locate the nerve in 38/147 TL (25.85 %), 20 RTL and 18 LTL (Fig. 4).
As we have said, the recurrent nerve is found with regard to its relationship with the ZT in 147/155 (94.83 %). Considering all the cases, when the recurrent nerve was not apparent, we did not insist in looking in 12/195 TL (6.15 %).
We carried out intra-operative monitoring of the recurrent nerve in 169/195 (86.66 %) cases; in the rest (13.44 %), either the electrode tubes were not used or their collocation was incorrect, or—following the criteria of not insisting on looking for the nerve when not found—the nerve did not appear following a prudent search. That is to say, that in those cases where intra-operative neuro-monitoring was foreseen (184), it was not used in 10/184 (5.43 %) where the recurrent nerve was not located.
Following the dissection of 195 TL (105 patients) we had unilateral definitive recurrent nerve paralysis in one case (0.95 %), and in nine cases (8.57 %) there was slight or complete transitory unilateral paralysis.
On the right side, the recurrent nerve ran laterally to the ZT on six occasions. This occurred because the nerve formed an angle of about 30° on the right with the laryngotracheal axis, so it can run laterally to a small ZT. In only one case did the recurrent nerve run above the ZT.
The recurrent nerve, in almost half the cases (41 %), divided into two or more branches before penetrating the cricothyroid membrane, being divided or not had no influence on the position of the nerve with regard to the ZT. As occurs with the upper parathyroid gland, help in locating the recurrent nerve with reference to the ZT is somewhat clearer and more frequent on the right side.
Considering the 155/195 ZT located, 32/155 (20.64 %) had less than 10 mm at the greater axis (grade 2); 115/155 (74.19 %) were between 10 and 20 mm (grade 3); only 8/155 (5.16 %) were more than 20 mm (grade 4).
The ZT is situated on the posterolateral border of the TL; in 109/155 of the cases (70.32 %) it is slipped behind the trachea (Fig. 1). Although we have found cases in which the ZT is extended behind the oesophagus (which, when it occurs, is easier to see in the LTL), we cannot quantify these occurrences statistically.
Discussion
In our surgical experience, the ZT clearly helps in the detection of the upper parathyroid gland and the allied recurrent nerve/lower thyroid artery. The embryology of the thyroid gland explains the origin of the ZT and its relationship to the upper parathyroid gland and the recurrent nerve.
The development of the thyroid gland occurs from a medial primordium and two lateral primordial [16, 17], beginning at the end of the 3rd week of gestation and is completed in the 10th week. The medial primordium, exceptionally, of endodermic origin, appears from the oropharyngeal medial line in the 3rd or 4th week and gives way to follicular thyroid tissue. The lateral primordium comes from the ultimobranchial body (which derives from the ventral portion of the 5th pharyngeal branchial pouch in about the 5th week of gestation [6, 18]); it contains the parafollicular cells which originated in the neural crest, and are of neuroectodermic origin, and secrete calcitonin. In the 10th week, the right and left lateral primordium are incorporated into the medial primordium and constitute the total of the thyroid gland [6, 17]. The incorporation of the ultimo-branchial body to the medial primordium produces a protuberance in the posterolateral border of the thyroid lobe, which we know as the ZT.
The dorsal wing of the 4th endobronchial pouch forms the upper parathyroid gland [6, 18]. The ultimobranchial body along with the upper parathyroid gland joins to the thyroid gland for its descent down the neck, and this explains the constant relationship between the parathyroid gland upper with the ZT. In our observations, the upper parathyroid gland is located immediately cranial to the ZT and not below it, as is sometimes described [6].
The lower parathyroid gland drops towards the neck accompanied by the thymus gland, and is situated definitively in a caudal position to the thyroid lobe, with no constant relationship with the ZT, which can be considered certain regarding its location in surgery.
The recurrent nerve stems from the vagus; it develops from the mesenchyme of the 4th and 5th pharyngeal pouch, and goes round the 4th aortic arch [18]. For this reason, the lower thyroid artery—which has its origin in this 4th aortic arch—is found next to the nerve in a varying relationship, passing the nerve, over, under or between arterial branches.
As is well known, in its migration the descending thyroid gland leaves a stem, which joins it to the pharyngeal ground, which is the Hiss thyroglossal canal. This canal from the 2nd month, fragments and dissolves. A vestige of thyroglossal canal joined to the thyroid gland frequently persists, which is the Lalouette pyramidal lobe.
The general lack of knowledge about the ZT is surprising. Wang [19] studied the position of 312 upper parathyroid glands in 160 necropsies, and in the anatomical references cited, there is no mention of the ZT. Pelizzo et al. [8] in 1998 published an interesting piece on the ZT, yet, in an earlier publication (1993) [20] it is not mentioned; it had probably been seen repeatedly in their operations but since they had no account of previous references of its existence, it was passed over.
In this investigative study, it is important that surgical operations and the study of the ZT are always carried out by the same surgeon; certain subjectivity is inevitable at the moment of recognising the ZT, this subjectivity notably increases in external assessment done by different observers.
If the ZT is as surgically important as we claim, why is it not known by many surgeons and otolaryngologists? In the first place, it is due to their not having an account of the detailed anatomical theory. It is also due to its being positioned on the posterolateral border of the TL (to the cricoid level and first tracheal rings, generally slipping behind them), to see it, it is necessary to trace the gland outward, so that the posterolateral border loses its form and position (Figs. 1, 4, 5). Its being surrounded by dense areolar tissue and close to the Berry ligament makes recognition and dissection of the ZT difficult; this surgical moment is the key point in the preservation of the recurrent nerve (Fig. 4).
The ZT is the expression of the lateral primordium of the thyroid gland at its point of union with the medial primordium; it is a vestige of the lateral primordium in the same way that the Lalouette pyramidal is a vestige of the thyroglossal diverticulum. We do not recognise the ZT in a considerable percentage of cases (20.51 %), probably because, the development of the lateral primordium can diffuse and disappear inside the TL.
The thyroid nodules can make identification of the ZT difficult [11]. One reason why the ZT is sometimes not recognised is that surgery frequently carried out on multinodular goitres, and occasionally a nodule, could outline the posterolateral border of the TL and camouflage the ZT. We have commented that, in addition to its inspection function, palpation helps to distinguish the ZT from a thyroid nodule.
The ZT is present in a varying number of cases (in our study, in 155/195; 79.48 %), but it is always relatively frequent, some consider that it exists in all thyroid glands [21]. In our study, the ZT is recognised to a significantly greater number in right TL (84.84 %) than in left TL (73.95 %); this difference (P = 0.06) may be due to events conditioned by the fusion of the right and left lateral primordium with the central primordium.
In our criteria, the CT or MR imagery in axial projections, coronal or sagittal in opposition to some claims [12], do not serve in the determination of whether the ZT are made retrovisceral; frequently in imagery it can be seen how the most posterior limit of the lateral border of the TL is inserted behind the trachea and/or oesophagus, but we cannot determine whether it is in fact the ZT or another portion of the same border.
The ZT may be important in oncogenesis; being the development point of these parafollicular cells may be the origin de medullary carcinoma [6, 18, 22]. Although this may occasionally be the case, it is not demonstrated; we think that, when parafollicular cells are diffused into the thyroid parenchyma, the medullary carcinoma does not necessarily have to be situated in the ZT.
Some authors consider that the ZT produces compression symptoms, in up to 58.3 % in those which measured more than 1 cm [5, 12]. Except in an occasional rare case in very demonstrative magnetic resonance, we do not believe a more reliable method exists by which we may see whether tracheal or oesophagus compression is produced by the ZT or by the union of the TL, with this last being the most likely.
The gradation system published in 1998 by Pelizzo et al. [8] is the most commonly commented upon, even in the most up to date publications [23], we believe that it is useful and practical because of its simplicity. The modifications we propose are: grade 1 should be made up of those cases in which, because of minimum size or other circumstances, we cannot be sure that a swelling on the border of the TL really is a ZT (doubtful ZT), and that those ZT greater than 20 mm should constitute a separate group (grade 4) (Table 1).
Conclusions
The ZT is certainly detected in the posterolateral border of the TL in a high percentage of thyroidectomies (79.48 %). The ZT is somewhat more frequent in the RTL than in LTL (P = 0.06). The ZT represents a clear difficulty in thyroidectomies since its dissection is usually difficult and laborious. Identifying the ZT when it exists is of fundamental help in the location/preservation of the recurrent nerve and of the upper parathyroid gland.
References
Madelung OW (1879) Anatomisches und Chirurgischen über die Glandula Thyreiodea Acessoria. Arch Klin Chir 24:71–107
Zuckerkandl E (1902) Nebst Bemerkungen über die Epithelkörperchen des Menschen. Anat Hefte LXI:61–82
Dunhill TP (1919) Some considerations on the operation for exophthalmic goitre. Br J Surg 7:195–210
Gilmour JR (1938) The gross anatomy of the parathyroid glands. J Pathol 46:133–149
Reeve TS, Delbridge L, Cohen A, Crummer P (1987) Total thyroidectomy. Ann Surg 206:782–786
Chevallier JM, Martelli H, Wind P (1995) La découverte chirurgicale des glandes parathyroïdes et du nerf laringe récurrent. Ann Chir 49:04–296
Dubost C (1991) Les parathyroïdes Endocrinologie chirurgicale. MEDSI/McGraw-Hill, Paris, pp 55–96
Pelizzo MR, Toniato A, Gemo G (1998) Zuckerkandl’s tuberculum: an arrow pointing to the recurrent laryngeal nerve. J Am Coll Surg 187:333–336
Leow CK (1999) Zuckerkandl’s tuberculum. J Am Coll Surg 188:334–336
Gamsenjaeger EW, Schweizer I (1999) Zuckerkandl’s tuberculum in thyroid surgery. J Am Coll Surg 188:336–337
Koςak S, Aydintug S (1999) Zuckerkandl’s tuberculum. J Am Coll Surg 188:333–337
Hisham AN, Aina IN (2000) Zuckerkandl’s tubercle of the thyroid gland in association with pressure symptoms: a coincidence or consequence? Aust NZ J Surg 70:251–253
Gauger PG, Delbridge LW, Thompson NW, Crummer P, Reeve TS (2001) Incidence and importance of the tubercle of zuckerkandl in thyroid surgery. Eur J Surg 167:249–254
Gamsenjaeger E (2009) Atlas of thyroid surgery, 1st edn. Thieme Medical Publishers, New York, pp 25–41
Terris DJ, Gourin ChG (2009) Thyroid and parthyroid diseases, 1st edn. Thieme Medical Publishers, New York, pp 81–89
Skandalakis JE, Gray SW, Todd NW (1994) The pharynx and its derivatives. In: Skandalakis JE, Gray SW (eds) Embryology for surgeons, 2nd edn. Williams and Wilkins, Baltimore, pp 27–31
Mansberger AR, Wei JP (1993) Surgical embryology and anatomy of the thyroid and parathyroid glands. Surg Clin North Am 73:727–746
Mirilas P, Skandalakis JE (2003) Zuckerkandl’s Tubercle. Aníbal ad Portas 196:796–801
Wang ChA (1976) The anatomic basis of parathyroid surgery. Ann Surg 183:271–275
Pelizzo MR, Toniato A, Briguglio F (1993) Acceso laterale in chirurgia tiroidea. Minerva Chir 48:189–191
Bliss RD, Gauger PG, Delbridge LW (2000) Surgeon’s approach to the thyroid gland. Surgical anatomy and the importance of technique. World J Surg 24:891–897
Williams ED, Toyn CE, Harach HR (1989) The ultimobranquial gland and congenital thyroid abnormalities in man. J Path 159:135–141
Sheaham P, Murphy MS (2011) Thyroid Tubercle of Zuckerkandl: Importance in Thyroid Surgery. Laryngoscope 121:2335–2337
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gil-Carcedo, E., Menéndez, M.E., Vallejo, L.A. et al. The Zuckerkandl tubercle: problematic or helpful in thyroid surgery?. Eur Arch Otorhinolaryngol 270, 2327–2332 (2013). https://doi.org/10.1007/s00405-012-2334-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-2334-7