Abstract
Atrophic rhinitis (AR) is a chronic inflammation of the nose characterized by an atrophy of the nasal mucosa. This is typically associated with an impaired sense of smell and a subjective sensation of poor nasal breathing. The aim of this study is to assess chemosensory function in patients suffering from AR using psychophysical testings and event-related potentials (ERP) responses. A cohort of nine patients was extensively studied. Eight out of nine had secondary AR sequela of a bilateral total inferior turbinectomy whereas one patient had a primary AR. All the patients had a clinical evaluation using Sniffin’ Sticks test and a retro-olfaction test and an electrophysiological evaluation based upon ERPs obtained after both olfactory and trigeminal stimuli. All the patients complained of a poor nasal breathing and presented a distortion of the chemosensory function. Actually, the orthonasal psychophysical testing showed that four patients out of nine had anosmia, three out of nine had hyposmia and two out of nine were normosmic. All the patients demonstrated retro-olfaction scores inferior to the normal values. The chemosensory ERP showed that seven patients had no olfactory response whereas six had no trigeminal response. Four patients had neither olfactory nor trigeminal ERP response. In conclusion, this study demonstrates that most patients with AR secondary to a total bilateral inferior turbinectomy have a reduction of the chemosensory function measured objectively by psychophysical testings and ERP. Moreover, the trigeminal responses were absent in all the cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrophic rhinitis (AR) is a chronic inflammation of the nose characterized by an atrophy of the nasal mucosa including the glands, the blood vessels, the turbinate bones and the nerve elements supplying the nose. The clinical examination reveals nasal cavities filled with foul smelling crusts which are green or dark green (Fig. 1). Patients usually complain of dryness of the nose, a subjective sensation of paradoxical nasal obstruction and loss of smell.
Endoscopic and CT scan view. Endoscopic view of the right (a) and left (b) nasal fossae. We can note a postoperative status, with subtotal inferior turbinectomy. The mucosa is atrophic, crusty and we can note mucopurulent rhinorhea (IT inferior turbinate, *nasal septum). c, d CT scan of a patient suffering from secondary atrophic rhinitis. Both coronal (c) and axial (d) planes show a post operative status, with a bilateral total inferior turbinectomy in c, and both inferior and middle bilateral turbinectomy in d
AR can be primary (idiopathic) or secondary
Primary atrophic rhinitis (PAR) is also called as rhinitis fetida or rhinitis sicca or ozena. PAR is particularly rare in European countries. Its etiology is not so clear. Many factors are supposed to play a role such as infection by Klebsiella ozaenae, Staphylococcus aureus, Coccibacillus, Proteus mirabilis, Escherichia coli, Bacillus mucosus. But autoimmunity, chronic infection of the sinuses, endocrine factors, poor nutritional status, heredity and iron deficiency anemia are other possible contributing factors [1, 2].
Secondary atrophic rhinitis (SAR) may result from chronic infection, head and neck radiotherapy, Sjögren’s syndrome, or even granulomatous disease [2]. Another common major cause of SAR is an excessive and extensive sinonasal surgery with complete resection of the inferior turbinates combined or not with a middle turbinectomy (Figs. 1c, d, 2). Such a radical procedure may lead to the development of an empty nose syndrome. There is no clear consensus to describe this syndrome. Classically, the clinical examination shows widely open nasal fossae with atrophic tissue and abundant crusts. The patients may complain of a paradoxical nasal obstruction, but can also report various unspecific symptoms, such as dryness of the nose, post nasal dripping, difficulties to breathe, headaches sleep disorder and impairment of the sense of smell [3]. Chemosensory dysfunction may vary from quantitative disorder (hypo-anosmia) to qualitative one, with cacosmia [2, 3]. The incidence of SAR after surgery is a matter of debate and varies from author to author. Passali et al. [4] reported an incidence of 22% of “atrophy” following a turbinectomy, Oburra [5] noted 15% of mucosal atrophy following a bilateral turbinectomy and Manzoor et al. [6] noted 13% incidence of AR following a total inferior turbinectomy. On the other hand, other authors did not report any disturbing symptoms related to turbinate resection [7, 8].
In AR, two of the most common symptoms are the subjective sensation of poor nasal breathing and the smell dysfunction. In the literature, the paradoxical impairment of nasal breathing is classically explained by a non-physiological airflow through the nasal fossae, due to a decreased resistance in the nasal fossae and a redistribution of the nasal airflow. This leads to a poor stimulation of both the olfactory and trigeminal nerves [2, 9].
Following these statements, we may thus hypothesize that the complete resection of the turbinates (in SAR) or the replacement of the nasal mucosa and/or olfactory neuroepithelium (in case of PAR or SAR) by a squamous cell metaplasia may lead to an impairment of olfactory and trigeminal functions.
The aim of this study was to evaluate the chemosensory function in patients suffering from AR using psychophysical olfactory testing’s and chemosensory event-related potential (ERP) recordings in order to demonstrate whether or not there is any objectified repercussion of the AR on their olfactory and trigeminal function.
Patients and methods
A cohort of nine patients suffering from AR was included in this study. There were six women and three men. The mean age was 47.4 year old (range 28–63 years).
The patients complained of: (paradoxical) nasal obstruction, olfactory disorder, headaches, rhinorrhea, and dry nose. Two or more of these symptoms with a clear demonstration of an atrophic mucosa and crusts in the nasal cavities were required to ascertain the diagnosis of AR.
Eight patients underwent an extensive sinonasal surgery whereas only one had PAR.
All patients had a clinical examination, psychophysical olfactory testing (both orthonasal and retronasal test) and chemosensory ERP recordings (both after olfactory and trigeminal stimulation).
Psychophysical olfactory testing
Psychophysical testing of the orthonasal olfactory function was performed with the validated Sniffin’ Sticks test [10]. Odors are presented to patients in felt-tip pens, which are placed approximately 2 cm in front of both nostrils allowing a bi-rhinal stimulation. This test encompasses three different approaches. First, the odor threshold is assessed with n-butanol with stepwise dilutions in a row of 16 felt tip pens. Second, patients are asked to discriminate odors 16 times. Third, a row of 16 odors is presented to the patients together with a list of four verbal descriptors that are used by the subjects to identify individual odors. To judge olfactory function, results from testing of odor threshold (T), odor discrimination (D) and odor identification (I) are added together to provide a total TDI score. For healthy subjects the TDI score at the 10th percentile is 30.3 for ages from 16 to 35 years, 27.3 for ages from 36 to 55 years, and 19.6 for patients >55 years. Functional anosmia is diagnosed if the TDI score is <16. With a score between 16 and normal age-related value, patients are considered hyposmic. Retronasal olfactory performances were also evaluated with a row of 20 different odors intraorally presented following a standardized method as well [11].
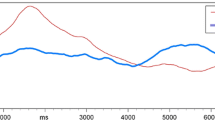
Chemosensory ERPs
Chemosensory function was also assessed with chemosensory, late near-field ERP elicited with relatively specific olfactory (2-Phenyl ethyl alcohol) and trigeminal stimuli (CO2). The frequency spectrum of the chemosensory ERPs is 2–8 Hz. We used a sampling frequency of 256 Hz, low pass filtering of 20 Hz and high pass filtering of 0.01 Hz. Recording sites were located in the midline in clinical circumstances (positions Fz, Cz and Pz of the international 10/20 system), referenced to linked mastoids. For averaging, typically 10–30 records are used. The number of artifact free recording must be >60% in order to allow analysis. The pre-trigger period is 500 ms and post-trigger sampling is 1,500 ms [12]. The outlet piece of the olfactometer was placed in the right nostril just behind the nasal valve 2–4 mm from the nares. In many clinical situations, electrophysiological responses are usually interpreted as being present or not, which is heuristically determined [13]. In this study, the analysis of the ERPs was performed in a dichotomic way, the N1P2 complex being present or absent if demonstrated in the amplitudes and latencies described in the literature [13].
Investigations were approved by the institutional ethical committee. Written inform consent was obtained from all patients.
Results
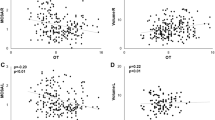
Table 1 lists the clinical symptoms reported by the patients. As expected, distorted olfactory perception and poor nasal breathing were the most frequently symptoms encountered. The psychophysical testing showed that four patients were anosmic, three were hyposmic and two were normosmic. All patients demonstrated retronasal olfaction scores inferior to the normal value. Taking into consideration the orthonasal and retronasal scores, all patients had a chemosensory dysfunction. On the chemosensory ERP seven patients out of nine had no olfactory responses. The only two patients that exhibited olfactory responses were females of 28 and 30 years old of age. They were categorized as hyposmic patients according to the orthonasal scores. Trigeminal ERPs were not recorded in six of nine patients. If we look at both olfactory and trigeminal responses, four patients had no olfactory or trigeminal responses, two had olfactory but no trigeminal responses and two had trigeminal but no olfactory responses. None of them had both olfactory and trigeminal response. Thus, none of the patients were considered as normal at the electrophysiological level. A detailed description of the results is given in Table 2.
Discussion
The nasal fossa has double innervations: the trigeminal and the olfactory systems. Most odorants stimulate both of these systems [14]. The trigeminal nerve, via its maxillary and ethmoid branches is responsible for the thermoalgesic sensation, such as touch, burning, cooling and pain and gives the airflow sensation [14]. These trigeminal fibers mainly innervate the inferior turbinate tissues. Nevertheless, we still do not know which kind of trigeminal stimulation gives airflow sensation [15, 16]. The olfactory nerve has its free nerve endings located in the olfactory neuroepithelium. It is generally agreed that the olfactory neuroepithelium is located in the upper part of the nasal cavity, on the dorsal aspect of the nasal vault, septum and superior turbinate. But a recent study by Leopold et al. [17] using electro-olfactogram and biopsies has showed that the olfactory neuroepithelium is also distributed more anteriorly, and is present close to the anterior insertion of the middle turbinate and in the mucosa of the middle turbinate. In addition, we know that trigeminal and olfactory systems interact closely with each other to determinate odorous sensations. Indeed, it is well known that interaction between olfactory and trigeminal system has a powerful influence on odor and trigeminal perception [18–20]. Studies have shown that the olfactory loss changes the processing of trigeminal mediated information, giving a decreased responsiveness to trigeminal stimulation [13, 21, 22]. This reduced trigeminal sensitivity is due to the lack of central-nervous interactions. Nevertheless, on peripheral level, adaptive mechanisms exist that lead to increase in trigeminal responsiveness [23]. Following these statements we may thus hypothesize that the complete resection of the turbinates (in SAR) or the replacement of the nasal mucosa and/or olfactory neuroepithelium (in case of PAR or SAR) by a squamous cell metaplasia may lead to an impairment of olfactory and trigeminal functions.
In this study, psychophysical evaluation of patients shows decreased TDI score in Sniffin’ Sticks test and decreased retro-olfaction score for the majority of patients, demonstrating a sense of smell impairment. More over chemosensory ERP were absent after both olfactory and trigeminal stimulation for the vast majority of the patients.
These results corroborate well with the sensation of impairment of the sense of smell frequently reported by the patients with AR [2, 3]. Surprisingly very few objective information exist on this topic in the literature and this study was undertaken to provide these objective data.
In this cohort, only two patients had olfactory ERP. These patients were hyposmic considering the scores obtained at the Sniffin’ sticks tests. They were young women (28 and 30 years old). This finding is probably supported by the fact that women exhibit higher olfactory performances than men, and that there is a significant effect of age and sex for olfactory ERP. Indeed, it is well documented in the literature that the amplitudes of olfactory ERP decrease with the age, while the latencies increase [24–27]. In addition, women exhibit higher amplitudes of late positive complex inside the responses compared to males [24]. Therefore it is not surprising that we recorded olfactory ERP for them. On the contrary, two patients exhibited a normal score in Sniffin’ Sticks test although no olfactory ERP was recorded. This might be explained considering a study conducted by Lötsch et al. [28] in which it is established that the chances to record an olfactory ERP increase with the Sniffin’ stick score and that the probability to detect an olfactory ERP becomes greater than 50% as the TDI score is upper than 22.6. But even with a high score, the probability not to detect an olfactory ERP is present and we may advance that in AR patients the changes in the nasal airflow passing through the nasal fossae may be an explanation. Nevertheless, we admit that the absence of OERP in the majority of patients is controversial and may be considered as biased as one of the inclusion criteria was olfactory disorder, and also because some patients had extensive sinonasal surgery for chronic rhino-sinusitis. Finally, as shown on Fig. 1, patients exhibited rhinorrhea and crusts, and thus may have multiplicity of reasons why chemosensory function is abnormal.
Considering trigeminal ERP, they are absent in six patients out of nine although they are frequently recorded in cohort of patients having an olfactory dysfunction. Except for technical problems, trigeminal ERP are recorded in the vast majority of the patients with an olfactory dysfunction if the integrity of the inferior turbinates is demonstrated [12, 13]. Indeed, studies on the evaluation of trigeminal function in anosmic and hyposmic patients suggest that their trigeminal sensitivity is decreased [13, 22]; nevertheless, trigeminal ERP can still be recorded in these patients, which is not the case in AR, even at suprathreshold levels. Thus, AR patients constitute a unique cohort of subjects having no trigeminal ERP among the different groups of patients with a chemosensory dysfunction. Another group is the very few patients who underwent a surgical removal of the trigeminal nerve or sensory ganglia [29].
As we said before, the loss of olfactory function may result from a multiplicity of reasons in this cohort of patients that is why we will not extend on that. The absence of trigeminal ERP responses is an interesting finding. This might be explained by the resection of the inferior and/or middle turbinate (Fig. 1). Indeed, the rich innervations of the inferior turbinates with trigeminal fibers make them responsible in a large part for the trigeminal sensation. Also, the removal of the inferior and/or middle turbinates dramatically changes the airflow pattern. Indeed, in healthy nose, the airflow is mainly along the floor of the nasal fossae and between the nasal septum and the middle turbinate with only 10–15% of the air passing through the olfactory cleft [9, 30, 31]. In an atrophic nose, Garcia et al. [9] have shown, using computational fluid dynamics techniques, that most of the air flows along the upper half of the nose. This will lead to increased water fluxes and consequently to high levels of mucus evaporation. This drying effect of the airflow is also accused for being responsible for the replacement of the normal nasal epithelium and/or olfactory neuroepithelium by a squamous metaplasia, inflicting considerable damages to trigeminal nerve endings and olfactory receptor neurons [9, 30–32]. Nevertheless, our results should be tempered by the fact that this study relies on a small number of patients. It should thus be interesting to investigate electrophysiological responses in a more important cohort of patients. In particular, exploring separately a cohort of PAR and SAR would be an interesting issue. It would also be interesting to study patients with inferior turbinectomy, performed for a nasal obstruction without concomitant sinus disease to investigate their olfactory function without the bias of a chronic inflammation within the paranasal sinus cavities.
Finally, we cannot demonstrate a clear correlation between both the type of surgery or clinical examination and the results of the olfactory and trigeminal testing. A possible explanation could be an interindividual variability. This might be reflected by different degrees of squamous metaplasia among the patients, a difference in the trigeminal and olfactory nerve endings distribution or even more differences in the innate olfactory capacities among the patients.
These variabilities among patients could also explain why not all the patients complain of AR after a radical and excessive sinonasal surgery. Patient-related factors and other undefined factors could certainly play a role and merits further research.
Conclusion
In conclusion, this study demonstrated an objective impairment of the sense of smell in patients suffering from AR using chemosensory testing and ERP. Actually, nearly all of the patients had no chemosensory responses. For us, this is an additional argument to state that radical surgery and particularly turbinectomies should not be performed to treat nasal obstruction because of the inconveniences it generates.
References
Jaswal A, Jana AK, Sikder Biswajit, Nandi TK, Sadhukhan SK, Das A (2008) Novel treatment of atrophic rhinitis: early results. Eur Arch Otorhinolaryngol 265(10):1211–1217
Hildenbrand T, Weber RK, Brehmer D (2011) Rhinitis sicca, dry nose and atrophic rhinitis: a review of the literature. Eur Arch Otorhinolaryngol 268(1):17–26. doi:10.1007/s00405-010-1391-z
Houser SM (2007) Surgical treatment for empty nose syndrome. Arch Otolaryngol Head Neck surgery 133(9):858–863
Passali D, Lauriello M, Anselmi M, Bellussi L (1995) Treatment of hypertrophy of the inferior turbinate: long term result in 382 patients randomly assigned to therapy. Ann Otol Rhinol Laryngol 108:569–575
Oburra HO (1995) Complications following bilateral turbinectomy. East Afr Med J 72:101–102
Manzoor T, Asghar A, Aslam S, Ali M, Ayub W (2008) Partial inferior turbinectomy; a better management option for hypertrophied inferior turbinates. Prof Med J 15(4):512–517
Ophir D (1990) Resection of obstructing inferior turbinates following rhinoplasty. Plast Reconstruct Surg 85:724–727
Cook PR, Begegni A, Bryant WC, Davis WE (1995) Effect of partial middle turbinectomy on nasal airflow and resistance. Otolaryngol Head Neck Surg 113:413–419
Garcia GJ, Bailie N, Martins DA, Kimbell JS (2007) Atrophic rhinitis: a CFD study of air conditioning in the nasal cavitty. J Appl Physiol 103(3):1082–1092
Hummel T, Kobal G, Gudziol H, Mackay-Sim A (2007) Normative data for the Sniffin Sticks including test of odor identification, odor discrimination and or odor thresholds: an upgrade based on a group of more than 3000 subjects. Eur Arch Otorhinolaryngol 264:237–243
Heilmann S, Strelle G, Rosenheim K, Damm M, Hummel T (2002) Clinical assessment of retronasal olfactory function. Arch Otolaryngol Head Neck Surg 128:414–418
Rombaux P, Mouraux A, Collet S, Eloy P, Bertrand B (2009) Usefulness and feasibility of psychophysical and electrophysiological olfactory testing in the rhinology clinic. Rhinology 47:23–35
Hummel T, Barz S, Lötsch J, Roscher S, Kettenmann B, Kobal G (1996) Loss of olfactory function leads to a decrease of trigeminal sensitivity. Chem Senses 21:75–79
Doty RL, Brugger WPE, Jurs PC, Orndorff MA, Snyder PJ, Lowry LD (1978) Intranasal trigeminal stimulation from odours volatiles: psychometric responses from anosmic and normal humans. Physiol Behav 20:175–185
Hummel T, Livermore A (2002) Intranasal chemosensory function of the trigeminal nerve and aspects of its relation to olfaction. Int Arch Occup Environ Health 75:305–313
Wrobel BB, Leopold DA (2005) Olfactory and sensory attributes of the nose. Otolaryngol Clin North Am 38(6):1163–1170
Leopold DA, Hummel T, Schwob JE, Hong SC, Knecht M, Kobal G (2000) Anterior distribution of human olfactory epithelium. Laryngoscope 110:417–421
Livermore A, Hummel T (2005) The influence of training on chemosensory event-related potentials and interactions between the olfactory and trigeminal systems. Chem Senses 29:41–51
Cain WS, Murphy C (1980) Interaction between chemoreceptive modalities of odour and irritation. Nature 284:255–257
Bensafi M, Frasnelli J, Reden J, Hummel T (2007) The neural represention of odor is modulated by the presence of a trigeminal stimulus during odor encoding. Clin Neurophysiol 118:696–701
Iannilli E, Gerber J, Frasnelli J, Hummel T (2007) Intranasal trigeminal function in subjects with and without and intact sense of smell. Brain Res 1139:235–244
Rombaux P, Mouraux A, Keller T, Hummel T (2008) Trigeminal event related potentials in patients with an olfactory dysfunction. Rhinology 46(3):170–174
Frasnelli J, Hummel T (2007) Interactions between the chemical senses: trigeminal function in patients with olfactory loss. Int J Psychophysiol 65(3):177–181
Stuck BA, Frey S, Freiburg S, Hörmann K, Zahnert T, Hummel T (2006) Chemosensory event-related potentials in relation to side of stimulation, age, sex, and stimulus concentration. Clin Neurophysiol 117(6):1367–1375
Hummel T, Barz S, Pauli E, Kobal G (1998) Chemosensory event-related potentials change as a function of age. Electroencephalogr Clin Neurophysiol 108:208–217
Covington J, Geilser M, Polich J, Murphy C (1999) Normal aging and odor intensity effects on the olfactory event-related potentials. Int J Psychophysiol 32:205–214
Morgan CD, Covington JW, Geisler MW, Polich J, Murphy C (1997) Olfactory event-related potentials: older males demonstrate the greatest deficits. Electroencephalogr Clin Neurophysiol 104:351–358
Lötsch J, Hummel T (2006) The clinical significance of electrophysiological measures of olfactory function. Behav Brain Res 170:78–83
Hussner A, Frasnelli J, Welge-Lüssen A, Reiss G, Zahnert T, Hummel T (2006) Loss of trigeminal sensitivity reduces olfactory function. Laryngoscope 116(8):1520–1522
Subramaniam RP, Richardson RB, Morgan KT, Kimbell JS, Guilmette RA (1998) Computational fluid dynamics simulations of inspired airflow in human nose and nasopharynx. Inhal Toxicol 10:91–120
Wolf M, Naftali S, Schroter RC, Elad D (2004) Air-conditioning characteristics oft he human nose. J Laryngol Otol 118:87–92
Boyce J, Eccles R (2006) Do chronic changes in nasal airflow have any physiological or pathological effect on the nose and paranasal sinuses? A systematic review. Clin Otolaryngol 31:15–19
Conflict of interest
The authors have no conflict of interest regarding this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00405-011-1752-2
Rights and permissions
About this article
Cite this article
Huart, C., Eloy, P., Collet, S. et al. Chemosensory function assessed with psychophysical testing and event-related potentials in patients with atrophic rhinitis. Eur Arch Otorhinolaryngol 269, 135–141 (2012). https://doi.org/10.1007/s00405-011-1670-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1670-3