Abstract
The level of success of neurovascular decompression in ponto-cerebellar angle for hemifacial spasm and trigeminal neuralgia has already established the reality of the pathology to explain such symptoms. However, cochlear nerve compression syndrome by vascular loop is still a controversial topic. We have performed a retrospective cases review with long-term follow-up (5–7 years) concerning the results of microvascular decompression surgery of the cochlear nerve via an endoscopy assisted retrosigmoid approach on 15 patients suffering from unilateral incapacitating tinnitus with abnormal auditory brainstem response and an offending vessel on magnetic resonance imaging. During the surgery, a vascular compression was found on every patient. In a long-term follow-up, 53.3% (8 cases) of our tinnitus cases improved and 20% (3 cases) of them were completely cured. The ABR returned to normal in all patients who had good clinical results (diminished or disappeared tinnitus). When a vertebral artery loop (5 cases) was concerned we obtained 80% of good clinical results. No one showed amelioration or sudden aggravation of their hearing. Three cases required surgical correction of cerebrospinal fluid leak and one case developed spontaneously regressive swallowing problems. Such microvascular decompression surgery of the cochlear nerve appears to be successful in treating incapaciting tinnitus in particular when a vertebral artery loop is observed. Therefore, in such a case, one might recommend neurovascular decompression surgery, keeping in mind that the complications of this surgery should be minimized by a careful closure of the retrosigmoid approach. In order to ensure a better selection of patient more accurate cochlear nerve monitoring and functional MRI should be a promising assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the significant success rate of the microvascular decompression surgery (introduced by Jannetta in the 1970s), the reality of neurovascular conflicts into the ponto-cerebellar angle is now undeniable. In fact, over 80% of our results have been successful for the trigeminal neuralgia and over 90% for the hemifacial spasm [1, 2]. Nevertheless, the microvascular decompression surgery of the cochlear nerve for incapacitating tinnitus remains a controversial subject for many reasons.
First of all, many diseases can cause tinnitus; so it is difficult to select the patients who really depend on this pathology. Secondly, tinnitus is a subjective symptom with central and psychological components. Therefore, and according to Adams [3], the fact that VIII compression syndrome provokes an isolated and disabling tinnitus remains a hypothesis too vague to justify surgery. In fact, the percentages of success of VIII decompression surgery in literature are still low, success rates varying from 40 to 77% [4–6], and the criteria to evaluate such results are not received a full agreement.
Our goal for this study was to select a homogeneous group of patients suffering from incapacitating tinnitus who underwent endoscopy-assisted microvascular decompression through a retrosigmoid keyhole approach.
Materials and methods
We carried out a retrospective study on a cohort of patients operated from 1994 to 2001. All patients were operated by the same senior surgeon. Fifteen patients formed the cohort (8 women–7 men) and the average age was 57 years old, ranging from 37 to 71 years old. The mean duration of tinnitus evolution just before surgery was 3.2 years (1–8 years). The follow-up period was 5–7 years (a mean 6 years).
The inclusion criteria required in such study were the following:
-
1.
Incapaciting tinnitus: Tinnitus must be unilateral, resistant to medical treatment and disabling, i.e., disturb patient’s daily activities (work-entertainment) and sleeping period, whatever the tinnitus types.
-
2.
Auditory brainstem response (ABR) alterations: ABR were altered among all patients with either an increased latency or a complete waves de-synchronization.
-
3.
A neurovascular conflict on magnetic reconance imaging (MRI): The MRI (T2 CISS sequences) showed in all patients a VIII neurovascular conflict defined by an orthogonal contact between the nerve and the blood vessel which provoked a nerve’s pathway distortion.
Pure-tone audiometry was performed pre-operatively and several times post-operatively. In the preoperative period, three patients (20%) had normal hearing (threshold ≤ 20 dB for frequencies ≤ 4 kHz) in the affected (later operated) ear before the operation. Twelve patients (80%) had a pre-operative sensorineural hearing loss. The mean threshold (average hearing loss at 0.5, 1, 2 and 4 kHz) was 38.5 dB ranging 22–85 dB.
The ABR were elicited using 80 and 90 dB clicks. An increased latency (I–III > 0.2 ms relative to that of the nonaffected ear, according to Möller [4]) was found in ten patients and a complete waves de-synchronization (peak I and/or III could not be identified) was found in five patients.
Caloric testing was performed to evaluate vestibular function pre-operatively and at long-term follow-up. This videonystagmography test has pointed out, preoperatively, two cases with vestibular hyporeflexia on tinnitus side.
All the patients were operated on by a minimal invasive retrosigmoid approach and with the adjunctive use of endoscopy:
A burr hole is placed and enlarged into a craniectomy (approximately 2–1.5 cm in diameter) whose borders are the transverse sinus superiorly and the sigmoid sinus laterally. The dura is opened in a U-shaped after hyperventilation to diminish CSF pressure. The microscope is introduced into the field and the cerebellum depressed spontaneously and progressively without use of retractor. Cerebrospinal fluid aspiration of the cerebellopontine angle cistern will also relax the cerebellum and provide adequate exposure. Endoscopy allows a good visualisation of any vascular compression (i.e., arteries and veins). Microvascular decompression for disabling tinnitus requires exposure of the entire eighth cranial nerve. The cerebellar flocculus is sharply dissected from the eighth nerve, fully exposing it from the brainstem to the porus acusticus.
Veins may be coagulated and divided, but arteries must be preserved and are, therefore, mobilized away from the nerve and kept in place by implants of Teflon [Teflon mesh, 10.2 × 10.2 cm plates (Bard® PTFE, Impra Inc., USA)]. Multiple pieces of soft-shredded teflon felt are used to shield the nerve and prevent later migration of the blood vessels.
The post-surgical evaluation was based on the patient’s own assessment of their relief of tinnitus obtained from patient records. The patients were divided into four groups according to this evaluation:
-
1.
Totally free of tinnitus.
-
2.
Improved (diminution of tinnitus).
-
3.
No change.
-
4.
Worse.
Results
In the immediate post-surgical period, tinnitus had disappeared in 8 cases out of 15 and had diminished in 2 cases out of 15, representing 66% positive results. At long-term follow-up, over 5 years, tinnitus had definitively disappeared in 3 cases out of 15 and decreased in 5 cases out of 15 which represent 53.3% of satisfactory results (Table 1). When a vertebral artery loop (n = 5) was concerned: three cases were totally free of tinnitus, one was improved and only one had no change. When AICA or PICA loops (n = 10) were concerned: only four cases were improved, and six had no change.
No tinnitus case worsened and no correlation was found between the tinnitus duration before surgery, the characters of tinnitus (pulsatile, high- middle- or low frequency) and the overall results.
The ABR returned to normal (I–III ≤ 0.2 ms relative to that of the nonoperated side) in all patients who had good clinical results (diminished or disappeared tinnitus) (Table 1).
In the postoperative period, no one showed improvement or sudden aggravation of their hearing. However, when we analyze the median of pure tone averages (PTA, i.e., average hearing loss at 0.5, 1, 2 and 4 kHz) in pre-operative (35.2 dB), post-operative (36.5 dB) and long-term follow-up (39 dB), we notice some degree of impairment of the auditory threshold [statistically significant differences between the three values (Wilcoxon test: P < 0.001)].
We did not establish any kind of relation between preoperative hearing and the results on tinnitus.
In the postoperative period, no patient complained of balance problems. Furthermore, from the two patients with vestibular hyporeflexia on tinnitus side, one has shown persistence of hyporeflexia with stable tinnitus and the second one shown vestibular test normalization with no tinnitus.
Out of 15 patients, the main side effect was a cerebrospinal fluid leak in 3 cases. They required additional surgery to close mastoid air cells inadvertently opened during surgical approach. In addition, we had one case of a spontaneous regressive swallowing problem due to the dissection of the lower cranial nerves.
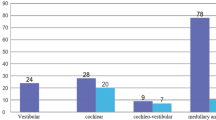
During surgery, we found several types of offending vessels (Table 1; Figs. 1, 2, 3). AICA and/or its collaterals (subarcuata artery) are the most common offending structures, 9 cases out of 15 (60%).
The imaging analysis compared with peroperative findings allows us to confirm the high level of sensitivity and specificity of the MRI assessment (Fig. 3), except when a small vascular element is involved like the subarcuata artery (Table 1).
Discussion
Despite precise and restrictive selection criteria (15 decompressions of VIII surgeries for tinnitus during our study vs. 700 decompressions of V and VII during the same period), the results obtained were limited and similar to those usually found in literature with a success rate from 40 to 77% [4–6]. Okamura et al. [7] have described results surprisingly higher with 94% of good results after surgery. Nevertheless, their patients’ selection process was different with intermittent tinnitus associated with vertigo or hearing loss instead of permanent incapacitating tinnitus encouraging surgical procedures. Ryu et al. [8] showed 65.5% satisfactory results when pre-surgery hearing remains. In our study, we have not found any connection between pre-surgery hearing and tinnitus results.
Which hypothesis can we bring forward to explain the lower results in auditory nerve from those after decompression of V or VII?
In fact, the etiologies of tinnitus are numerous and the clinical or para-clinical criteria explaining a neurovascular conflict with the cochlear nerve are still undefined. Our study demonstrates that when positive clinical results exist with reduction or disappearance of tinnitus, the ABR normalized. ABR alteration seems to be essential to propose surgery. Imaging is also required to objectively and precisely locate and differentiate an offending vessel from a normal vascular loop, which is very common in an asymptomatic patient [9]. Furthermore, the MRI is mandatory to exclude other pathologies (e.g., neurinoma) which may cause tinnitus [10].
The complexity of the surgery may also explain these results. Firstly, because the vascular compression can be found on all portions of the cochlear nerve cistern way. For the cochlear nerve, the location of the transitional glial zone (Obersteiner–Redlich zone) of the nerve is variable on the course of the nerve from the root entry zone to the intracanalar portion (including the cisternal portion and the meatus) [11]. Secondly, because the vascular conflicts due to the AICA (blood vessel foremost often responsible) are not always mobilized in safety (loop inside the internal auditory canal, AICA in clamp, AICA between the facial nerve and the cochlear nerve, labyrinthine arteries fixing the loop). In our study, when AICA or PICA loops were concerned (10 cases) we only obtained 40% of good clinical results. On the contrary, we obtained 80% of good clinical results when a vertebral artery loop was concerned (5 cases). Therefore, the decompression appears to be easier when a vertebral artery loop is concerned.
Such decompression can be achieved with the adjunctive use of endoscopy. Actually, the endoscopy allows a magnified vision of the ponto-cerebellar angle and the entire cochlear nerve way without distortion of the neurovascular structures. It is essential to know the exact course of the offending vessel and the way to safely mobilize these structures. It gives excellent definition of perforating blood vessels, VIII nerve and its root entry zone, which in many cases is superior to that achieved with microscope [12].
The cochlear nerve is particularly fragile to any surgical maneuver. All manipulations are risky and this is obvious when using cochlear monitoring. Which structures are involved in the generation of tinnitus? Moller [13] recorded directly on cochlear nerve composed action potentials (CAP) and demonstrated that CAP on patients with neurovascular conflict and tinnitus were not different from CAP from patients without tinnitus. One of the plausible hypotheses is that changes, which provoke tinnitus are not produced in the auditory nerve but in most rostral structures of the auditory nervous system. It appears undeniable that tinnitus can be caused by contact between a blood vessel and the auditory nerve; the abnormal neural activity which it results from is probably amplified at most rostral structures level which become hyperactive (some nervous nucleus of ascendant auditory way).
The vascular compression of the cochlear nerve is a clinical entity as trigeminal neuralgia and hemifacial spasm. However, its definition and assessment is more delicate and need further improvement. In addition, the central hyperactivity, which is revealed by the neurovascular conflict, is so far impossible to evaluate. So it does not allow us to predict effectiveness of the decompression surgery. So far, on a long-term follow-up of our selected patients 20% (3 out of 15 patients) were cured and about 50% (8 out of 15) were improved. This study demonstrated that unilateral incapacitating tinnitus with altered ABR and visualization of a neurovascular conflict on MRI can be cured by a surgical microvascular decompression. The successful clinical results are correlated to a normalization of ABR, which seems more easily obtained when a vertebral artery loop is concerned. Therefore, one might recommend neurovascular decompression surgery for severe tinnitus only when a vertebral artery loop is observed. Taking into account that a more careful closure of the retrosigmoid approach should prevent from CSF leakage, the complications of this surgery should be minimized. In order to ensure a better selection of patient more accurate cochlear nerve monitoring and functional MRI should be a promising assessment [14, 15].
References
El-Garem HF, Badr-El-Dine M, Talaat AM, Magnan J (2002) Endoscopy as a tool in minimally invasive trigeminal neuralgia surgery. Otol Neurotol 23:132–135
Badr-El-Dine M, El-Garem HF, Talaat AM, Magnan J (2002) Endoscopically assisted minimally invasive microvascular decompression of hemifacial spasm. Otol Neurotol 23:122–128
Adams CBT (1989) Microvascular compression: an alternative view and hyposthesis. J Neurosurg 57:1–12
Moller MB, Moller AR, Jannetta PJ et al (1993) Vascular decompression surgery for severe tinnitus: selection criteria and results. Laryngoscope 103:421–427
Brookes GB (1996) Vascular-decompression surgery for severe tinnitus. Am J Otol 17:569–576
Vasama JPI, Moller MB, Moller AR (1998) Microvascular decompression of the cochlear nerve in patients with severe tinnitus. Preoperative findings and operative outcome in 22 patients. Neurol Res 20:242–248
Okamura T, Kurokawa Y, Ikeda N et al (2000) Microvascular decompression for cochlear symptoms. J Neurosurg 93:421–426
Ryu H, Yamamoto S, Sugiyama K (1998) Neurovascular compression syndrome of the eight cranial nerve. What are the most reliable diagnostic signs? Acta Neurochir (Wien) 140:1279–1286
Makins AE, Nikolopoulos TP, Ludman C et al (1998) Is there a correlation between vascular loops and unilateral auditory symptoms? Laryngoscope 108:1739–1742
Weissman JL, Hirsch BE (2000) Imaging of tinnitus: a review. Radiology 216:342–349
Lang J (1981) Facial and vestibulocochlear nerve. Topographic anatomy and variations. In: Samii M, Jannetta PJ (eds) The cranial nerves. Springer, Heidelberg, pp 363–377
Wackym PA, King WA, Meyer GA et al (2002) Endoscopy in neuro-otologic surgery. Otolaryngol Clin North Am 35:297–323
Moller AR, Moller MB, Jannetta PJ et al (1992) Compound action potentials recorded from the exposed eight nerve in patients with intractable tinnitus. Laryngoscope 102:187–197
Legatt AD (2002) Mechanisms of intraoperative brainstem auditory evoked potential changes. J Clin Neurophysiol 19:396–408
MelcherJR, Sigalovsky IS, Guinan JJ et al (2000) Lateralized tinnitus studied with functional magnetic resonance imaging: Abnormal inferior colliculus activation. J Neurophysiol 83:1058–1072
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guevara, N., Deveze, A., Buza, V. et al. Microvascular decompression of cochlear nerve for tinnitus incapacity: pre-surgical data, surgical analyses and long-term follow-up of 15 patients. Eur Arch Otorhinolaryngol 265, 397–401 (2008). https://doi.org/10.1007/s00405-007-0471-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-007-0471-1