Abstract
Apneic patients have hypotonia of the lingual and supra-hyoid muscles. The dysfunction of theses muscles leading to a collapse of the upper airway is responsible for the apnea. The goal of this study, designed as a before-after trial, is to determine the effect of lingual and supra-hyoid muscle strengthening on obstructive sleep apnea. Thirty-four patients with obstructive sleep apnea were included (consecutive sample). Only 16 patients completed the study. The treatment consisted of 30 sessions of transcutaneous neuromuscular stimulation administered to the submental region associated with muscular exercises. The effect on apneic events was analyzed with a polysomnography before and after the treatment. Thirteen patients could be analyzed for the statistical studies. The mean apnea-hypopnea index (AHI) decreased from 32.9 to 20.6 (Wilcoxon rank test: P=0.017). Seven patients ended the study with an AHI of less than 10, and three more patients decreased their AHI by more than 50%. This treatment significantly decreased the AHI in most of the patients. A larger study with more patients and with a long-term follow-up is necessary to determine the place of physiotherapy in the treatment of obstructive sleep apnea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea is caused by a collapse of the upper airway during sleep. Nasally applied continuous positive airway pressure (nCPAP) is the treatment of choice for this syndrome. However, nCPAP is restricting for the patients, and the acceptance rate is estimated to be 60–70% [1]. Other treatment options (e.g., pharyngoplasty or mandibular advancement devices) aim to correct the anatomic perturbations that lead to this collapse. Nevertheless, some authors have shown that physiological dysfunctions such as muscle hypotonia are at the root of these anatomical perturbations [2, 3, 4]. A new treatment option, neuromuscular stimulation (NMS), has been developed for the obstructive sleep apnea syndrome (OSAS) in order to prevent pharyngeal muscle hypotonia during sleep [5, 6, 7, 8, 9, 10, 11, 12, 13].
In all these studies, the patient sleeps with a device that stimulates the genioglossus muscle during an apneic event in order to release the obstruction and hence to reduce the AHI. We have developed a different approach. We tried through daytime physiotherapy with NMS and muscular exercises to strengthen the supra-hyoid and lingual muscles in order to avoid the nocturnal obstructive events.
Materials and methods
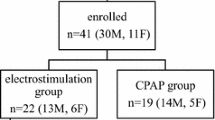
Thirty-four patients (25 men and 9 women) with an obstructive sleep apnea syndrome known to exist for at least 2 years were recruited via the Center of Sleep Disorders from the University Hospital St. Pierre in Brussels. Inclusion criteria were: AHI between 10 and 80, absence of a major morphologic abnormality (retrognathia, Pierre-Robin syndrome), absence of bucco-pharyngeal surgery and absence of drug or alcohol addiction. The age of the patients varied from 29 to 75. Seven patients already had been treated with nCPAP and two patients with a mandibular advancement device.
The patients were treated over 10 weeks with three weekly sessions of NMS. These sessions consisted of 30 min of NMS with skin electrodes in the submental region (using the Compex Sport-P device, Compex Medical SA, Switzerland) with biphasic pulses of 0.16 ms with a frequency of 33 Hz for a period of 9 s every 18 s. We asked the patient to choose the intensity of the stimulation just below the pain threshold with a minimal intensity of 25 mA. Besides these sessions of NMS, we asked them to execute a daily session of muscular exercise. We asked them alternatively to blow, stick out their tongue, whistle and push their tongue against the hard palate for 20 min.
A polysomnography was carried out before and after the 10 weeks of treatment. According to the American Academy of Sleep Medicine Task Force (1999) [14], apnea was defined as cessation of oronasal airflow for >10 s, and hypopnea was defined as a reduction of >50% of oronasal airflow lasting >10 s, or a clear airflow reduction associated with an arousal lasting >10 s. The patients’ weights were also recorded before and after the treatment. The Wilcoxon paired rank sum test was used to compare the pre- and post-therapeutic AHIs. A two-tailed P-value of 0.05 was considered statistically significant.
Results
Fifteen patients stopped the treatment after some sessions because it was too restricting. Three patients were excluded because they were not reliable. Among the 16 patients who completed the study, the mean AHI decreased from 31 to 24 after the study (see Table 1). Eight patients out of 16 ended the study with an AHI <10. Among these 16 patients, 3 gained weight during the treatment and increased their BMI by more than 10%. We analyzed the results for the 13 patients with a steady weight. The mean AHI decreased from 32.9 before the study to 20.6 after the study, and the median AHI from 28.9 to 8.6. This decrease was statistically significant (P=0.017). Seven patients (54%) ended the study with an AHI <10, and nine patients decreased their AHI by more than 50%. If one of these two factors was considered as an outcome of recovery, 77% (10/13) of the patients could be considered to be cured. If we classed the patients in subgroups considering the AHI before the treatment, the results were better when the pre-therapeutic AHI was low (Table 1): AHI: 10–20:100% recovery (n=5); AHI: 20–40:75% recovery (n=4); AHI >40:50% recovery (n=4).
Discussion
It is well known that the upper airway dilator muscles are important in the pathogenesis of OSAS [1, 2, 3, 4]. In some apneic patients, these muscles demonstrate a dysfunction (electromyographic wave amplitudes reduced, delayed contraction or abnormal response to stimuli) [2]. Therefore, we felt it would be interesting to attempt a treatment with physiotherapy in order to strengthen these muscles. We have not found any study of this kind in the literature.
Several studies have been published about neuromuscular stimulation (NMS) in OSAS [5, 6, 7, 8, 9, 10, 11, 12, 13]. The goal of these studies was to develop a device that stimulates dilator muscles (especially the genioglossus muscle) during sleep when an apnea occurs in order to terminate it. Miki et al. [8] first described the potential role of NMS in OSAS. They stimulated the genioglossus muscle with skin electrodes when a hypopnea lasted more than 4 s. This stimulation could then break the apneic event. With this device, the authors could significantly reduce the AHI. They also showed that the use of this device during several consecutive nights led to a reduction of the AHI for the next nights without the device [9]. These observations could be explained by the effect of strengthening of the genioglossus muscle by repeated stimulations and then confirmed our hypothesis on the role of the physiotherapy in OSAS. This study was criticized in the literature, and in 1992, Edmonds et al. [6] showed with sleep analysis that the reduction of the AHI was due to the arousal of the patient caused by the stimulation of the genioglossus muscle. Therefore, this stimulation did not improve the quality of sleep. Edmonds and al. showed that this stimulation with skin electrodes caused a contraction of the dilator airway muscles as well as their antagonists. Since then, other similar studies have been made with conflicting results [10, 11]. More recently, Schwartz et al. [13] showed that a selective stimulation of the genioglossus with fine wire electrodes placed intramuscularly increased the airflow, while selective stimulation of the hyoglossus or styloglossus muscles decreased the airflow. Mann et al. [5] also showed that NMS with hook wires inserted percutaneously in the genioglossus muscle significantly increased the diameter of the hypopharyngeal airway. Other studies have been made with direct hypoglossal nerve stimulation. The authors clipped a stimulator on the hypoglossal nerve or on the branch that supplies the genioglossus muscle. They could demonstrate an increase of the airflow [12] or a decrease of the AHI [11, 13] in patients with such implants. These studies are controversial because a chronic direct stimulation raises concern about the risk of nerve injury [5].
The aim of our study was completely different because our approach involves the strengthening of the lingual and supra-hyoid muscles during daytime in order to reduce the AHI and not to treat the apneic event with a device during sleep. Therefore, the stimulation of the dilator muscles of the upper airway as well as their antagonists does not prevent the global muscular strengthening. Thus, our study does not require a selective stimulation of specific muscles, which simplifies the treatment.
The results of this study are promising. Indeed, the mean AHI decreased from 32.9 to 20.6, and seven patients ended the study with an AHI <10. The results are statistically significant. If we define a success as a drop of more than 50% or an AHI <10, the success rate is 77%. This treatment seems to be more efficient for patients who have a mild OSAS. Indeed, when the pre-therapeutic AHI is between 10 and 20, the success rate is 100%. This rate drops when the pre-therapeutic AHI increases: 75 and 50% with a pre-therapeutic AHI between 20 and 30, and over 30, respectively. The long-term efficiency of this treatment is not known, but probably decreases when the treatment is stopped. This treatment is restricting for the patients, with three sessions of physiotherapy a week. This explains the low rate of compliance we obtained (47%). One patient, who did not gain weight, increased the AHI after the treatment. Maybe the polysomnography was not realized in good conditions, but it may be a side effect of the treatment with an increase of the local muscular mass. In order to determine the exact role of physiotherapy in OSAS, a larger study with a longer follow-up is necessary.
Conclusions
Physiotherapeutic treatment based on NMS and muscular exercises could have a place in the treatment of OSAS, particularly in the mild cases. Indeed, this treatment could help to prevent the muscular hypotonia that settles progressively in the OSAS. In order to determine the real efficacy and the potential place of this treatment in this disease, a larger study with a long-term follow-up is necessary
References
Verse T, Pirsig W (2001) New developments in the therapy of obstructive sleep apnea. Eur Arch Otorhinolaryngol 258:31–37
Blumen M, Chabolle F, Rabischong E et al (1998) Dilator muscles of the pharynx and their implication in the sleep apnea syndrome of obstructive type. Review of the literature. Ann Otolaryngol Chir Cervicofac 115:73–84
Veldi M, Vasar V, Hion T et al (2002) Myotonometry demonstrates changes of lingual musculature in obstructive sleep apnea. Eur Arch Otorhinolaryngol 259:108–112
Schwartz AR, O’Donnell CP, Baron J (1998) The hypotonic upper airway in obstructive sleep apnea: role of structures and neuromuscular activity. Am J Respir Crit Care Med 157:1051–1057
Mann EA, Burnett T, Cornell S et al (2002) The effect of neuromuscular stimulation of the genioglossus on the hypopharyngeal airway. Laryngoscope 112:351–356
Edmonds LC, Daniels BK, Stanson AW et al (1992) The effects of transcutaneous electrical stimulation during wakefulness and sleep in patients with obstructive sleep apnea. Am Rev Resp Dis 146:1030–1036
Schwartz AR, Eisele DW, Hari A et al (1996) Electrical stimulation of the lingual musculature in obstructive sleep apnea. J Applied Physiol 81:643–652
Miki H, Hida W, Chonan T et al (1989) Effects of submental electrical stimulation during sleep on upper airway patency in patients with obstructive sleep apnea. Am Rev Resp Dis 140:1285–1289
Hida W, Okabe S, Miki H et al (1994) Effects of submental stimulation for several consecutive nights in patients with obstructive sleep apnoea. Thorax 49:446–452
10. Guilleminault C, Powell N, Bowman B et al (1995) The effect of electrical stimulation on obstructive sleep apnea. Chest 107:67–73
Decker MJ, Haaga J, Arnold JL et al (1993) Functional electrical stimulation and respiration during sleep. J Applied Physiol 75:1053–1061
Eisele DW, Smith PL, Alam DS et al (1997) Direct hypoglossal nerve stimulation in obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 123:57–61
Schwartz AR, Bennet ML, Smith PL et al (2001) Therapeutic electrical stimulation of the hypoglossal nerve in obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 127:1216–1223
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–669
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lequeux, T., Chantrain, G., Bonnand, M. et al. Physiotherapy in obstructive sleep apnea syndrome: preliminary results. Eur Arch Otorhinolaryngol 262, 501–503 (2005). https://doi.org/10.1007/s00405-004-0806-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-004-0806-0