Abstract
Purpose
The incidence of placenta accreta spectrum (PAS; pathologic diagnosis of placenta accreta, increta or percreta) continues to rise in the USA. The purpose of this study is to compare the hemorrhagic morbidity associated with PAS with and without a placenta previa.
Methods
This was a retrospective cohort study of 105 deliveries from 1997 to 2017 with histologically confirmed PAS comparing outcomes in women with and without a coexisting placenta previa. We used the Wilcoxon rank sum test to compare continuous data and Chi-square or Fisher’s exact test for categorical data. We also performed log-binomial regression to calculate risk ratios adjusted for depth of invasion (aRR) and 95% confidence intervals (CI).
Results
We identified 105 pregnancies with PAS. Antenatal diagnosis of PAS was higher in women with coexisting placenta previa (72.3%) than those without (6.9%, p < 0.001). Women with coexisting placenta previa had greater median estimated blood loss and more units of packed red blood cells transfused (both p ≤ 0.03). Women with placenta previa were more likely to undergo a hysterectomy (RR 2.7; 95% CI 1.8–3.8) and be admitted to the intensive care unit (aRR 3.3; 95% CI 1.1–9.6).
Conclusions
Among women with PAS, those with a coexisting placenta previa experienced greater hemorrhagic morbidity compared to those without. In addition, PAS without placenta previa typically was not diagnosed prior to delivery. This study further supports the recommendation for multi-disciplinary planning and assurance of resources for pregnancies complicated by PAS. In addition, our results highlight the need for mobilization of resources for those pregnancies where PAS is not diagnosed until delivery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Placenta accreta spectrum (PAS), encompassing the terms placenta accreta, increta, and percreta; abnormally invasive placenta; morbidly adherent placenta; and invasive placentation, is a leading cause of life-threatening obstetric hemorrhage [1]. As such, PAS is a significant contributor to maternal morbidity. Most specifically, the risk of hemorrhagic morbidity for women with PAS is quite high, with up to 90% of women receiving a blood transfusion and 40% requiring more than 10 units of packed red blood cells [2]. Along with the increasing cesarean delivery rate in the USA, there has been a 30% increase in rate of PAS from 2000 to 2011 among women with prior cesarean deliveries [3,4,5,6].
While women with PAS are at risk for significant morbidity and mortality, little is known about the role of a coexisting placenta previa in terms of hemorrhagic risk. Given that previa is an independent risk factor for hemorrhage, pregnancies complicated by PAS and placenta previa may carry a compounded risk of hemorrhagic complications beyond that experienced with PAS alone. Therefore, we evaluated pregnancies with histologically confirmed PAS and compared the perinatal hemorrhagic morbidity among pregnancies complicated by placenta previa to those without. We hypothesized that PAS with placenta previa is associated with increased hemorrhagic morbidity compared to PAS without previa.
Materials and methods
This was a retrospective cohort study of women with histologically confirmed PAS who delivered at a single tertiary referral medical center from January 1, 1997 to July 18, 2017. We identified cases by querying our Department of Pathology’s clinical database for the term ‘creta’ and reviewing pathology reports to confirm the diagnosis of PAS. If the diagnosis of PAS was unclear based on review of the pathology report, slides from the case were examined by a perinatal pathologist (JLH) to determine inclusion. Histologic accreta was defined as the presence of placental villi adjacent to myometrial muscle without intervening decidua. Increta was defined as placental villi adjacent to myometrial muscle without intervening decidua, and irregular thinning of the underlying myometrium, and degeneration of muscle with edema and a cellular inflammatory response. Percreta was defined as increta with infiltration of trophoblast into adipose tissue beyond the uterine serosa or in the parametrium, or histologic features of increta within one millimeter of a surgical disruption of the uterine wall. Cases of cesarean scar dehiscence were identified and distinguished from percreta. Although such cases have a thin anterior lower uterine segment with focal areas of surgical disruption, that tissue is composed entirely of fibrotic tissue rather than smooth muscle; as such, these were labeled as increta. In cases of delivered placentas without a hysterectomy specimen, the histologic diagnosis of PAS was based on the presence of adherent myometrium adjacent to placental villi without intervening decidua. Adherent myometrial fibers along the maternal surface of the placenta within decidua were not diagnosed as accreta [7].
We confirmed the presence or the absence of placenta previa by either review of the pathology report of a hysterectomy specimen or review of ultrasound report preceding delivery. Previa was defined as the placenta overlying or abutting the internal cervical os. Low-lying placentas were included in the previa group, defined as placental edge measuring within two centimeters of the internal cervical os.
We abstracted demographic information, medical history, characteristics, and outcomes of the index pregnancy from the medical record. Antenatal suspicion of PAS was based on prenatal ultrasound records. The prenatal ultrasound diagnosis of suspected PAS was based on the presence of the following previously published ultrasound markers: the absence of hypoechoic retroplacental zone, multiple placental lacunae (vascular spaces), the presence of bridging vessels, and retroplacental myometrial thickness less than one millimeter [8].
Our primary outcome was blood product transfusion, which was defined as receiving one or more of the following within 48 h of delivery: packed red blood cells, fresh frozen plasma, platelets, cryoprecipitate, and cell salvage. Our secondary outcomes included the transfusion of individual products within 48 h of delivery, number of units transfused, estimated perinatal blood loss, hysterectomy, and admission to the intensive care unit. We obtained the type and volume of blood products from blood bank records and estimated blood loss from operative reports and delivery notes. Starting in 2015, we implemented a routine protocol of weighing surgical sponges for cases of PAS to better estimate blood loss; prior to that, blood loss was estimated by conventional means.
Data are presented as median (interquartile range) or proportion. We used the Wilcoxon rank sum test to compare continuous data and the Chi-square or Fisher’s exact test for categorical data. We also performed log-binomial regression to calculate risk ratios (RR) and 95% confidence intervals (CI). We considered depth of invasion and number of prior cesarean deliveries as potential confounders; however, the low incidence of some outcomes restricted our ability to adjust for both. Thus, models are adjusted only for depth of invasion. Data were analyzed with SAS 9.4 (SAS Institute Inc., Cary, NC). All tests were two-sided, and p values < 0.05 denoted statistical significance. All procedures performed in studies involving human participants were in accordance with Beth Israel Deaconess Medical Center Institutional Review Board (protocol #: 2017P-000607) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent process was waived given the retrospective nature of this study.
Results
We identified 334 potential cases of PAS through our database query, of which 115 were histologically confirmed. Of the 219 potential cases that were excluded, three were hysterectomy specimens from non-pregnant patients, one was missing delivery outcome data, and 215 were identified in the query for ‘creta’ because the pathology report included comments such as “no evidence of accreta” or “rule out accreta.” Of the 115 cases of histologically confirmed PAS, 10 were excluded due to pregnancy termination, leaving 47 (44.8%) pregnancies with coexisting previa and 58 (55.2%) without. Women with and without previa were similar with regard to baseline characteristics such as age, race/ethnicity and body mass index. However, women with previa were more likely to report current smoking, less likely to be nulliparous and more likely to have had a prior cesarean delivery as compared to women without previa. Among women with a prior cesarean delivery, 71.4% of those with previa and 66.7% of those without previa had a history of low transverse cesarean incision. Demographic characteristics and relevant obstetric and surgical history are shown in Table 1.
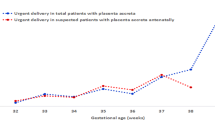
Antenatal suspicion of PAS occurred more often for women with previa (72.3%) compared to those without (6.9%); those with previa also were more likely to experience antenatal bleeding (both p < 0.001). Nearly, all women with PAS and a coexisting previa underwent cesarean delivery (97.9%). Median gestational age at delivery was earlier among pregnancies with previa. Prenatal and intrapartum characteristics are shown in Table 2.
The median preoperative hemoglobin was significantly lower for women with previa [11.2 (10.7–12.1)] compared to those without previa [12.1 (11.5–12.9); p = 0.001]. Among women with PAS, 85.1% with previa required a blood product transfusion compared to 37.9% without previa (p < 0.001). After adjusting for depth of invasion, women with previa were twice as likely (aRR 2.0, 95% CI 1.3–3.1) to receive a transfusion of any blood product compared to women without previa. Furthermore, among those with a preoperative hemoglobin less than 11, the risk of transfusion was 1.5 (95% CI 0.88–2.7) for women with previa compared to those without, adjusted for depth of invasion. Among women with a preoperative hemoglobin of 11 or higher, the risk of transfusion was 2.3 (95% CI 1.3–3.8) for women with previa compared those without, adjusted for depth of invasion. When evaluating individual blood products, women with previa were more likely to receive packed red blood cells, platelets, and cryoprecipitate; however, the groups were similar with regard to the incidence of transfusion of fresh frozen plasma and use of cell salvage. The incidences and risk ratios for blood product transfusion are shown in Table 3. Among those who received packed red blood cells, the median number of units received was significantly higher for those with previa [6.0 (3.0–12.0)] than those without [3.5 (2.0–6.0); p = 0.03]. The median number of units of fresh frozen plasma received was similar for women with previa [4.0 (2.0–10.5)] and those without [3.0 (2.0–6.0); p = 0.53)]. Similarly, there was no difference in the median units of cryoprecipitate received by those with previa [2.0 (2.0–5.0)] and those without [3.0 (1.0–6.0); p = 1.0].
Median estimated perinatal blood loss in women with and without previa was 3500 (2000–6500) mL and 1200 (800–2100) mL, respectively (p < 0.001). Compared to those without previa, those with previa experienced a significantly higher incidence of hysterectomy and intensive care unit admission (Table 3).
Discussion
Our findings support the hypothesis that women with PAS and a coexisting placenta previa have greater hemorrhagic morbidity than those without previa. Pregnancies complicated by both PAS and previa were twice as likely to require a transfusion of at least one blood product compared to pregnancies without previa. Specifically, those with previa were more likely to receive packed red blood cells, platelets, and cryoprecipitate. Women with PAS and previa also had a higher risk of hysterectomy and intensive care unit admission.
In one prior study evaluating the presence of “massive blood loss and transfusion,” defined as ≥ 5000 ml estimated blood loss or receiving ≥ 10 units of red blood cells, among women with PAS, the researchers reported that those with previa were more likely to have large volume transfusion compared to those without, suggesting previa in the setting of PAS increases the risk of massive transfusion [9]. In addition, a secondary analysis from a multicenter trial of academic medical centers on the association of hemorrhagic morbidity and primary cesarean delivery showed that women with previa were more likely to receive a transfusion of packed red blood cells and to undergo a hysterectomy than those without previa, though none of the women had PAS [10]. This study suggests that among pregnancies without PAS, previa is an independent risk factor for hemorrhagic morbidity. Our findings are consistent with both of these studies. In addition, women with previa had lower preoperative hemoglobin than those without previa, but the risk of transfusion was still higher in the previa group among those with higher preoperative hemoglobin, highlighting the increased hemorrhagic morbidity of those with previa and emphasizing the importance of prenatal diagnosis and preparation.
Prenatal diagnosis of PAS is associated with decreased maternal morbidity compared to intrapartum diagnosis and allows for preoperative planning and care [11, 12]. One intervention that has been shown to improve outcomes and reduce hemorrhagic morbidity in the setting of PAS is a multi-disciplinary team approach [13, 14]. A multi-disciplinary approach is supported by a recent joint consensus statement by the American College of Obstetricians and Gynecologist and the Society of Maternal–Fetal Medicine, as well as the evidence-based guidelines from the International Society for Abnormally Invasive Placenta [14, 15]. In our cohort, only four women without previa (6.9%) had a prenatal diagnosis of PAS, which highlights the difficulty of diagnosing PAS in the absence of previa. If we could improve diagnosis of PAS in the absence of previa, thus allowing for planned multi-disciplinary care, we suspect hemorrhagic morbidity for these women could be even further reduced.
Our study has limitations. First, some of our outcomes are subjective; specifically, the need for transfusion and estimated blood loss are often physician-dependent. Due to the retrospective study design, we could not assess adherence to standard guidelines for transfusion, which may have changed over the course of the study period, and we were limited to data that were available in the medical record. In particular, information regarding early ultrasounds and other early prenatal care was not available for some patients in this cohort due to our institution serving as a referral center. In addition, the ability to temporize bleeding by various measures (balloon tamponade, interventional radiologic procedure, direct over-sewing of the placenta bed) could influence the decision to transfuse. If uterine preservation was attempted, this could have resulted in additional transfusion while this was being performed. We were unable to abstract all details of attempted uterine preservation for this study. Given that previa is a known risk factor for peripartum hemorrhage, regardless of PAS, those with previa may have been more likely to be transfused due to heightened physician awareness and concern. In regards to the pathologic evaluation, there is no agreed upon nomenclature or definitions for PAS and its subcategories within the international pathology community. Although there was uniformity within our cases, with each being reviewed independently, our findings may not be generalizable to other institutions where pathologic criteria differ. Further, the generalizability of our findings may be limited as our study was performed at a single institution that serves as a regional referral center for PAS.
Importantly, our study also has several strengths. All cases of PAS and previa were histologically confirmed. Our samples were collected over two decades, which lessened the likelihood of uniform treatment of the diagnosis and increased the likelihood of management variation, which may better approximate clinical care. To our knowledge, this is the first study to attempt to assess the individual risk of a previa with PAS as it pertains to maternal hemorrhagic morbidity.
Though women with PAS and coexisting previa had a higher risk of hemorrhagic morbidity compared to women with PAS alone, both groups had a high absolute risk of hemorrhage, as measured by blood product transfusion, and intensive care unit admission. This not only highlights the importance of prenatal diagnosis and preparation for delivery involving a multi-disciplinary team, but also emphasizes the need to design protocols for blood supply management at non-specialty medical centers. Given most cases of PAS without previa in our cohort were not diagnosed prenatally, we suspect that the majority of these cases in the USA are similarly undiagnosed and deliver at non-specialty medical centers. Future work is needed to improve prenatal diagnosis of PAS to ensure multi-disciplinary delivery planning and reduction in hemorrhagic morbidity.
References
Sheiner E, Sarid L, Levy A, Seidman DS, Hallak M (2005) Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Maternal Fetal Neonatal Med 18(3):149–154. https://doi.org/10.1080/14767050500170088
O’Brien JM, Barton JR, Donaldson ES (1996) The management of placenta percreta: conservative and operative strategies. Am J Obstet Gynecol 175(6):1632–1638
Creanga AA, Bateman BT, Butwick AJ, Raleigh L, Maeda A, Kuklina E, Callaghan WM (2015) Morbidity associated with cesarean delivery in the United States: is placenta accreta an increasingly important contributor? Am J Obstet Gynecol 213(3):384.e1–384.e11. https://doi.org/10.1016/j.ajog.2015.05.002
Wu S, Kocherginsky M, Hibbard JU (2005) Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol 192(5):1458–1461. https://doi.org/10.1016/j.ajog.2004.12.074
Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA et al (2006) Maternal morbidity associated with repeat cesarean deliveries. Obstet Gynecol 107(6):1226–1232. https://doi.org/10.1097/01.AOG.0000219750.79480.84
Grobman WA, Gersnoviez R, Landon MB, Spong CY, Leveno KJ, Rouse DJ et al (2007) Pregnancy outcomes for women with placenta previa in relation to the number of prior cesarean deliveries. Obstet Gynecol 110(6):1249–1255. https://doi.org/10.1097/01.AOG.0000292082.80566.cd
Linn RL, Miller ES, Lim G, Ernst LM (2015) Adherent basal plate myometrial fibers in the delivered placenta as a risk factor for development of subsequent placenta accreta. Placenta 36(12):1419–1424. https://doi.org/10.1016/j.placenta.2015.10.004
Belfort MA (2010) Placenta accreta. Am J Obstet Gynecol 203(5):430–439. https://doi.org/10.1016/j.ajog.2010.09.013
Wright JD, Pri-Paz S, Herzog TJ, Shah M, Bonanno C, Lewin SN et al (2011) Predictors of massive blood loss in women with placenta accreta. Am J Obstet Gynecol 205(1):38.e1–38.e6. https://doi.org/10.1016/j.ajog.2011.01.040
Gibbins KJ, Einerson BD, Varner MW, Silver RM (2018) Placenta previa and maternal hemorrhagic morbidity. J Matern Fetal Neonatal Med 31(4):494–499
Warshak CR, Ramos GA, Eskander R, Benirschke K, Saenz CC, Kelly TF et al (2010) Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. Obstet Gynecol 115(1):65–69. https://doi.org/10.1097/AOG.0b013e3181c4f12a
Eller AG, Porter TF, Soisson P, Silver RM (2009) Optimal management strategies for placenta accreta. BJOG 116(5):648–654. https://doi.org/10.1111/j.1471-0528.2008.02037.x
Shamshirsaz AA, Fox KA, Salmanian B, Diaz-Arrastia CR, Wesley Lee, Wycke Baker et al (2015) Maternal morbidity in patients with morbidly adherent placenta treated with and without a standardized multidisciplinary approach. Am J Obstet Gynecol 212:218.e1–218.e9. https://doi.org/10.1016/j.ajog.2014.08.019
Collins SL, Alemdar B, van Beekhuizen HJ, Bertholdt C, Braun T, Calda P et al (2019) Evidence-based guidelines for the management of abnormally invasive placenta: recommendations from the International Society for Abnormally Invasive Placenta. Am J Obstet Gynecol 220(6):511–526
American College of Obstetricians and Gynecologists and Society for the Maternal-Fetal Medicine (2018) Obstetrics care consensus: placenta accreta spectrum. Obstet Gynecol 132(6):e259–e275
Acknowledgements
This work was conducted with support from Harvard Catalyst|The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health.
Funding
The work was conducted with support from the Charles Koch Foundation.
Author information
Authors and Affiliations
Contributions
BMM: data curation, methodology support, and writing of the manuscript. RW: data curation and critical editting of the manuscript. AMR: data curation, methodology support and critical editing of the manuscript. AMM: data analysis, methodology support, project administration and critical editing of the manuscript. MRH: study conception, analysis support, project supervision and critical editing of the manuscript. JLH: data curation, methodology support and critical editing of the manuscript. MHS: data curation and critical editing of the manuscript. SAS: study conception, funding aquisition, methodology, project supervision and criticial editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mulla, B.M., Weatherford, R., Redhunt, A.M. et al. Hemorrhagic morbidity in placenta accreta spectrum with and without placenta previa. Arch Gynecol Obstet 300, 1601–1606 (2019). https://doi.org/10.1007/s00404-019-05338-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05338-y