Abstract
Purpose
To evaluate the practice patterns among centers and physicians worldwide regarding sentinel lymph node biopsies (SLNB) in cervical cancer (CC) patients.
Method
A validated 35-item questionnaire regarding SLNB in CC supported by the Gynecologic Cancer Intergroup (GCIG), and sponsored by the North-Eastern German Society of Gynaecologic–Oncology (NOGGO) was sent to all major gynecological cancer societies across the globe for further distribution from October 2015 and continued for a period of 7 months.
Results
One hundred and sixty-one institutions from around the world participated. One hundred and six (66%) of the participants were from university centers and 111 (69%) were gynecologic oncologists. One hundred and fifty-two (97%) performed lymphadenectomy (LNE) and 147 (94%) did so systematically; 97 (60%) used SLNB, due to lower morbidity (73%), reliability (55%) and time-saving (27%). In cases of positive SLNB (pN+), 39% of respondents stopped the operation and sent the patient for chemoradiation (CRT), 45% completed pelvic and paraaortic LNE, whereas 26% went on to perform a radical hysterectomy (RH) and systematic pelvic and paraaortic LNE. In case of negative SLNB (pN0), 39% of institutions still performed a systematic pelvic and paraaortic LNE.
Conclusion
In this survey worldwide, SLNB adoption is an encouraging 60%, yet ample differences exist regarding strategy, and to a lower extent the techniques used. Lack of experience is the most common reason SLNB is not performed. Efforts to increase surgical education on SLNB technique and multicenter prospective trials providing evidence-based guidelines are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer (CC) is the third most common female cancer worldwide and the fourth leading cause of cancer death in women. In recent years, the number of young women with CC, which is particularly prevalent in developing countries, has increased.
Metastatic lymph node involvement (pN+) of the pelvic lymph nodes (LNs) is the main prognostic factor in early-stage cervical cancer (ESCC): 5-year overall survival in stage IB1 with and without pN+ is 75.9% vs. 94.8%, respectively [1].
LN status evaluation cannot be reliably determined pre-operatively, hence pelvic lymphadenectomy (LNE) is a pivotal part of the treatment for most patients with CC [2]. As a matter of fact, the new 2018 FIGO staging has now introduced the LN status [3]. However, notwithstanding the introduction of minimally invasive techniques such as laparoscopy and robotic surgery, LNE continues to be associated with substantial morbidity [4].
The reported incidence of pN+ in patients with ESCC is 0–4.8% in FIGO stage IA, less than 15% in patients with stage IB < 2 cm, and 12–27% in stage IIA [5]. Thus, > 95% of stage IA do not need full LNE and the majority of patients with ESCC will not benefit from a pelvic LNE. Conversely, they are at risk of suffering from a variety of potential complications such as venous thromboembolism, or lymphocyst formation, and life-long sequelae comprising of neuropathy and lower extremity lymphedema (LEL).
Sentinel lymph node biopsy (SLNB) has been effectively adopted for many years now and is currently the standard of care in patients with breast cancer (BC), vulvar cancer, and melanoma [6,7,8].
Numerous studies and publications have extensively documented both the feasibility of SLNB identification in patients with CC, as well as its validity mostly in selected patients, particularly in cases of tumors < 2 cm [9, 10]. Yet there is still much debate, and no international agreement has been reached as for the role of SLNB in the treatment of ESCC.
The main goal of this investigation was to evaluate physician practices on a global stage regarding the current use of SLNB in CC patients. Additionally, the potential interest of the gynecological world in taking part in future clinical studies about SLNB was determined.
Materials and methods
The present study was initiated by the North-Eastern-German Society of Gynaecologic-Oncology (NOGGO), was officially backed by the Gynecologic Cancer Intergroup (GCIG), and was also officially supported by the main gynecological oncologic societies and study groups worldwide.
After receiving approval from NOGGO, a full mailing list of all candidate members of major international gynecological cancer societies was obtained. Subsequently, the survey was posted online (https://de.surveymonkey.com/s/SLN_cervicalcancer) and mailed to the above-stated oncologic centers for further distribution from October 12, 2015 to May 06, 2016. Respondents could freely choose which format to use.
The 35-item questionnaire, focused on the LNE and SLNB in CC patients and validated in the German language, was defined based on interdisciplinary workshops and previous studies in other malignancies. It was tested by ten physicians for reproducibility and could be completed anonymously in an estimated 15 min time. Many questions were to be answered in a multiple-choice fashion.
To encourage participation, all 27 study group members were sent two mailings of the survey and a reminder. All collected data were stored by an institutional research department at the institution of one of the authors. The entire questionnaire can be found in the supplement file of this article (Appendix 1).
Statistical analysis
All results are presented as frequency and rate. Associations were evaluated using chi-squared test, Fisher’s exact test or Kendall’s tau b where appropriate. All data were analyzed using IBM® SPSS® Statistics 23 (SPSS Inc., Chicago, IL) and p < 0.05 was considered statistically significant.
Results
Answers from 161 centers from four continents were completed and returned to NOGGO. Groups were: Western and Southern Europe (WSE) (Belgium, Netherland, France, Italy, Spain, Israel) 35.4%; Central Europe (CE) (Austria, Germany, Switzerland) 24.2%; Northern Europe (NE) (Denmark, Finland, Sweden, Norway) 6.8%; Anglo-Saxons (Ireland, UK, USA, Canada, Australia, New Zealand) 14.9%; Asia (Japan, Korea) 5%; and Other (Mexico, and unknown) 13.7%.
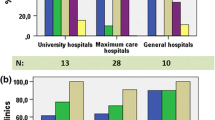
Roughly two-thirds of respondents (66.6%) were from university clinics (106/161), 1 in 4 (24.4%) was a teaching hospital (39/161) and 1 in 12 (8%) was a tertiary care level center (13/161). Two out of three participants (69.2%) were gynecologic oncologists (111/161).
According to the average volume of patients treated annually over a period of 3 years, and also specifically in the last year, eight subgroups were evaluated, from ≤ 20 to ≥ 300 patients. 57.8% of centers (93/161) had an average of up to 80 patients per year; 7.5% of centers (12/161) had treated > 100 patients over the last year.
Answers were analyzed consecutively and comparisons were drawn among the various regions of the world, among centers with different patient volumes, as well as with regard to the kind of institution, i.e. university vs general hospitals, and the subspecialty of the participant gynecologist, i.e. gynecologist oncologist vs general gynecologist.
For the sake of brevity in this paper, these different groups will be referred to as the following when needed: A (geographically), B (volume), C (type of center), and D (subspecialty).
LNE (97.4%) (152/156) and precisely mainly a systematic LNE (94.8%) (147/155) was common to all participants (A–D). However, SLNB use in CC was 60.6% (97/160) with nadir values as low as 30% in Northern Europe (NE), where imaging was instead relied upon (43%).
In addition, participants (A–D) carried out the procedure extremely seldom alone (0.8%), and generally replied that the most usual reason for not performing SLNB was lack of experience (> 40%). Other regions of the world (88.9%) (p 0.031), low-volume centers (57.7%) (p 0.024), and general gynecologists (60.9%) (p 0.032) were definitively more prone to give this latter answer (Table 1).
Laparoscopy represented the most frequent surgical approach (60%), though in CE and Asia laparotomy was used more frequently. Robotic assistance was prevalent in NE (90%) and Anglo-Saxons (45.8%) (p < 0.001), in high-volume centers (55.6%) (p < 0.001), in university settings (37.7%) (p 0.002), and among gynecologist oncologists (35.1%) (p 0.040).
For all respondents (A–D), overwhelmingly, lower morbidity (> 60–100%), with the exception of NE (33.3%) (p 0.128), and increased reliability (50–73%), apart from CE (21.7%) (p 0.007), general gynecologists (30.8%) (p 0.005) and non-university settings (39.3%) (p 0.045), were deemed the main advantages of SLNB (Table 1).
Additionally about one in four participants praised the reduced surgical time of the technique, compared to that of systematic LNE (15–35%). NE on the other hand considered SLNB neither faster (0%) nor associated with lower morbidity (33%).
SLNB was neither extremely popular for obese patients (16.5%) nor for elderly patients (16.5%): Anglo-Saxons (6.3%) and low-volume institutions (4.3%) were even less likely to use it in this latter group of patients (Table 1).
SLNB was generally more frequently performed for cancers ≤ 2 cm (46.9%) and ≤ 4 cm (43.8%) regardless of histologic grade, and lymph (L) and vascular (V) status. Only CE and Asia preferred it for lower grade (G1–G2) (> 33%) (p 0.001), as well as non-university centers (26.8%) (p 0.009) and to a lower extent general gynecologists (29.6%) (p 0. 038) (Table 2).
No group set age limits for SLNB; however, remarkably few participants used it for patients desiring to preserve fertility (5.2%).
Low-volume centers (39.1%) and non-university hospitals (42.9%) (p 0.008) predominantly performed SLNB in patients with no history of previous treatment; conversely, Anglo-Saxons (43.8%) and Asia (50%) were using it more frequently independent of previous cancer therapy. Responders (A–D) were split with 45% waiting for final histology, as opposed to 55% relying on frozen section (FS): specifically Anglo-Saxons (33.3%) (p 0.115), high-volume institutions (45.5%) (p 0.107), and gynecologist oncologists (20.6%) (p 0.093) associated frozen section (FS) with SLNB only when this would change their management, i.e. in fertility-sparing cases.
Serial sectioning (SS) during FS was the norm (97–100%); immuno-histochemistry (IHC) use was also very common (86–100%), apart from Asia (50%) (p 0.179).
Except for low-volume institutions (78.9%) (p 0.022), all participants (A–D) were consistent in answering that FS identified more frequently macro-metastasis (MTS) (80–100%), micro-MTS (µMTS) (45–65%) and finally isolated tumor cells (ITC) (13–25%), respectively.
SLNB pN+ most often defined µMTS (78%), MTS (61%), and rarely ITC (19%).
Vice versa and interestingly, respondents (A–D) showed markedly different strategies following FS evaluation of SLNB.
In the case of FS pN+, 39% stopped the operation after SLNB and opted for chemoradiation (CRT), 45% completed pelvic and paraaortic LNE, and 26% went on to perform LNE and radical hysterectomy (RH). Asia (80%) (p 0.056), high-volume centers (54.5%) (p 0.394), and general gynecologists (45.5%) (p 0.011) more commonly turned to this latter approach, as opposed to NE (0%) (Table 3).
Respondents (A–D) were almost equally split in case of FS pN0 SLNB, with 39% completing a systematic LNE and 41.6% avoiding any additional LN removal: NE was the only exception with 100% additional systematic LNE.
Likewise, participants were divided when asked about their behavior in the presence of enlarged LNs at the time of SLNB pN0: 55.7% simply removed them, and always in the case of NE (100%), 38% added systematic LNE, and 6.3% left them, relying solely on SLNB, with a peak of 40% in Asia (40%).
Anglo-Saxons and Asia (56.3% and 63.7%, respectively) (p 0.090), high-volume hospitals (58.3%) (p 0.132) and gynecologic oncologists (40.8%) (p 0.243) used indocyanine green (ICG) more frequently (Table 4).
Site and modality of tracer injection were relatively standardized, apart from Anglo-Saxons who rarely (6.3%) and WSE who often (66.7%) (p 0.042) used intracervical deep injection (Table 4).
The majority of respondents (72–100%) did not use colposcopic assistance to inject the tracer, and never high-volume centers (100%); only exceptions were SWE and CE with 20.6% and 31.8%, respectively, of no users (p 0.090). Finally, low-volume centers rarely injected in four quadrants (30.4%) (p 0.024) (Table 4).
Almost 90% of respondents (A–D) used scintigraphy to detect SLN.
University centers tended to have a longer interval between tracer injection and LNs removal (p 0.005) (Table 4).
Low-volume groups (61.9%) (p 0.009) and general gynecologists (66.7%) (p 0.014) were less aware of their detection rate.
About 40% of respondents (A–D) had ongoing trials, > 90% agreed to participate in a SLNB retrial, and 96.5% was ready to support international study concepts about the role of SLNB in the management of CC.
Discussion
This study is the largest international survey on the current practice patterns of SLNB use in CC. Even though the overwhelming majority of centers across the globe perform LNE in CC, SLNB is not yet part of routine treatment of this malignancy.
No major differences were seen among centers worldwide, among different volume hospitals, between university and non-academic institutions, or gynecologic oncologists versus general gynecologists regarding SLNB use in CC. Only NE, to some extent, showed inconsistent results, i.e. NE seldom used SLNB (30%) and always performed systematic LNE in cases of FS pN0 SLNB. Additionally, our investigation highlights the differences regarding the techniques of SLNB in CC.
Moreover respondents around the globe after both FS pN0 and FS pN+ SLNB had markedly different therapeutic strategies.
Following FS pN+ SLNB, 39% of respondents (A–D) opted for CRT, yet Asia, high-volume centers and general gynecologists seldom aborted the RH (45–80%).
Conversely, in cases of FS pN0 SLNB equally frequent strategies, such as additional systematic LNE (39%) or no further LNs removal (41.6%), were used (A–D).
FIGO staging in CC is and remains clinical, relying on clinical factors such as tumor dimension < or > 4 cm. Indeed, tumor size correlates closely with increased pN+; hence, precise evaluation of LNs is important as therapeutic decisions are made [11].
The development and adoption of laparoscopy, and its intrinsic lower associated morbidity have additionally contributed to the standardization of LNE as part of a thorough staging of CC, now regarded as irreplaceable, leading some groups to advocate its use in extreme cases [12].
LNE is to be considered both the ultimate diagnostic tool, since it allows upstaging in up to 43% of patients, as well an important therapeutic step in the management of CC, according to the number and location of removed LNs in case of MTS and µMTS [13, 14].
There is increasing evidence that SLNB in ESCC is accurate in detecting pN+, with results equivalent to breast cancer (BC), vulvar cancer and melanoma, tumors for which this method is an accepted standard of care [15, 16]. SLNB has been incorporated in the National Comprehensive Cancer Network (NCCN) treatment algorithm of CC, and is now increasingly adopted.
Bats et al. in a randomized trial in SLNB-negative patients (SENTICOL 2, NCT01639820) tested both quality of life (QoL) and safety matters: SLNB can indeed be used to identify which patients will highly benefit from a complete LNE from the ones in whom the procedure would potentially cause unnecessary iatrogenic damage with no therapeutic advantage [17].
A recent analysis of published studies reported a detection rate (DR) of 95% and sensitivity of 100% for SLNB in CC < 2 cm [18].
Cibula et al. described high sensitivity and low false negative rate (FNR) of SLNB when sentinel LNs were detected bilaterally, and proposed that this procedure and ultrastaging should become standard practice in the surgical management of ESCC [19]. The group at the MD Anderson Cancer Center recently stated: “We believe it is time to change the standard of care for women with early-stage cervical cancer to SLN biopsy only” [20].
Results with SLNB in ESCC are promising. Supporters of this technique praise its rapidity and reliability in selected patients, along with its decreased morbidity; its opponents, vice versa, question its feasibility, and highlight the paucity of sufficient scientific evidence, or even their deeper trust in imaging techniques [21, 22].
Skeptics point out the high FNR, the importance of precise knowledge of LNs status in the parametrium, as well as the possible atypical site of pN+, which can be missed by SLNB. Further they question the use of SLNB in bulky tumors or locally advanced cervical cancer (LACC) with massive lymph node involvement, the role of SLNB being different in ESCC as opposed to LACC [23,24,25,26].
Moreover, SLNB detractors also mention the additional costs of ultrastaging and subsequent therapy due to presence of µMTS, whereas unnecessary adjuvant treatment has also a price for the patients [25].
The debate about SLNB in CC is further complicated by the current uncertainty and lack of understanding of the clinical role of some additional pieces of information, i.e. µMTS or ITC, thus “questioning” the need for ultrastaging [22, 27,28,29,30,31]. Indeed despite pN0 some groups still advocate in particular cases to perform a systematic LNE, or question the real meaning of pN0 with HPV detection in sentinel nodes [32].
Last but not least, fear of skip MTS, though rare, the current limits of FS evaluation of SLNB in CC, despite the long proven feasibility and role of SLNB in breast and vulvar cancers, and melanoma, together with the absence of widespread acceptance of the few existing prospective studies have hindered international agreement on this procedure and its diffusion in clinical practice [27, 33,34,35].
Nonetheless, SLNB has potential advantages. It could reduce blood loss, operative time, increase identification of pN+ through ultrastaging, as well as allow for potential detection of an alternative lymphatic drainage site, and reduce morbidity [36].
SLNB in CC is still in its infancy and can well be defined as a work in progress. The lack of standardized strategies and the current ample differences in technique reflect more personal surgeon’s experience and preferences; hence, authors’ opinions are still very heterogeneous and evolving [10, 18, 33].
For this reason and to optimize SLNB results, it is important to use algorithm and to carefully select patients pre-operatively [31, 37]. This includes evaluation of tumor size, the surgeon’s learning curve and experience, histologic type, lymphovascular space invasion (LVSI), pre-operative treatment, body mass index (BMI), bilaterality, as well as the availability of reliable intra-operative pathological investigation, i.e. ultrastaging, and the standardization of the method including type, volume and timing of injection of the tracers, before SLNB could be used routinely [10, 18, 27,28,29,30,31, 37, 38].
Worldwide, ESCC treatment strategies are far from being standardized and are currently under new scrutiny. In addition, stage-related mortality rates for CC in richer countries despite its marked decreased incidence have remained relatively stable; hence, controlled radicality and patient’s tailored treatment to cut down unnecessary iatrogenic morbidity are mandatory [11, 22, 39]. Likewise, despite the pivotal role of LNs status in the treatment of CC, the mere fact that > 2/3 of ESCC patients will be pN0 and will not profit from a complete LNE, but will potentially suffer life-long sequelae, is forcing the debate over the future role of SLNB in CC, and even more so with respect to subcategories such as obese and elderly patients [10, 39].
Unfortunately, there is still limited awareness of therapy associated with QoL in CC patients. A previous SGO survey on FS evaluation of LNs in CC showed that RH abortion in case of pN+ is still rare (21%) [40]. Similarly, a quarter to four fifths of centers in our study still performs RH and systematic LNE in pN+ SLNB patients, who are bound to receive additional CRT.
Nonetheless, the implementation of new techniques (ICG) could speed up the use and acceptance of SLNB in the diagnostic and therapeutic CC algorithm [37, 38].
Our study has several flaws.
The primary limitation is sampling bias. Despite a much larger expected amount of responses worldwide, many countries were represented by a very limited number of groups; hence, they are not adequately depicted, and the results are possibly not representative of the most commonly used SLNB strategies in ESCC worldwide.
Furthermore, there may have been a selection bias. Participants of centers performing SLNB were more likely to have higher surgical expertise and to complete the survey. Additionally, the predominance of academic institutions, gynecologic oncologists, and also members of the GCIG community, whose physicians are generally highly motivated in clinical trials and innovations, would once more mean that the outcomes may not correctly illustrate the view of the entire gynecological community.
The strengths of our study are the heterogeneity of participants both in regional terms, having received answers from four continents, as well as their different working environments, from low- to middle- and high-volume centers, university and general hospitals, and personal background, i.e. subspecialty.
The overall number of answers is sufficient to reliably highlight both common procedures used, as well as differences regarding SLNB in CC, whereas the matched comparison of different groups of respondents (B–D) is fully representative of the current state of this procedure in the gynecological universe.
Moreover, responders predominantly expressed their availability and inclination to take part in multicenter prospective studies about SLNB in CC. Thus, this survey clearly shows the willingness, desire and need of participants to establish this technique, to define its indications by selecting a target population, and to standardize this procedure.
Conclusion
The current questionnaire demonstrates encouraging levels of adoption of SLNB in CC across the globe; there is, however, a lack of international consensus and considerable differences mostly regarding SLNB strategy in CC worldwide. This is not a complete surprise and may reflect the relatively limited efforts to surgically train gynecologic oncologists in SLNB technique, and to complete international trials, resulting in conflicting evidence in the literature.
There is a high need for educational and training programs, harmonization of guidelines and conduct for prospective trials to evaluate the role of SLNB in ESCC as well as in LACC.
The hope is to maximize the surgical information about LN status while limiting the unnecessary human cost associated with it, and eventually coming up with more definitive answers as to the optimal treatment of ESCC.
References
Delgado G, Bundy BN, Fowler WC Jr, Stehman FB, Sevin B, Creasman WT, Major F, DiSaia P, Zaino R (1989) A prospective surgical pathological study of stage I squamous carcinoma of the cervix: a Gynecologic Oncology Group Study. Gynecol Oncol 35(3):314–320
Driscoll DO, Halpenny D, Johnston C, Sheehy N, Keogan M (2015) 18F-FDG-PET/CT is of limited value in primary staging of early stage cervical cancer. Abdom Imaging 40(1):127–133
Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R (2018) Cancer of the cervix uteri. Int J Gynaecol Obstet 143(Suppl 2):22–36. https://doi.org/10.1002/ijgo.12611
Beesley V, Janda M, Eakin E, Obermair A, Battistutta D (2007) Lymphedema after gynecological cancer treatment: prevalence, correlates, and supportive care needs. Cancer 109(12):2607–2614
Magrina JF, Goodrich MA, Lidner TK, Weaver AL, Cornella JL, Podratz KC (1999) Modified radical hysterectomy in the treatment of early squamous cervical cancer. Gynecol Oncol 72(2):183–186
Aldredge LM (2007) The role of sentinel node biopsy in patients with cutaneous melanoma. Nurs Clin North Am 42(3):379–392 (v–vi)
Veronesi U, Paganelli G, Viale G, Galimberti V, Luini A, Zurrida S, Robertson C, Sacchini V, Veronesi P, Orvieto E, De Cicco C, Intra M, Tosi G, Scarpa D (1999) Sentinel lymph node biopsy and axillary dissection in breast cancer: results in a large series. J Natl Cancer Inst 91(4):368–373
De Cicco C, Sideri M, Bartolomei M, Grana C, Cremonesi M, Fiorenza M, Maggioni A, Bocciolone L, Mangioni C, Colombo N, Paganelli G (2000) Sentinel node biopsy in early vulvar cancer. Br J Cancer 82(2):295–299
Plante M, Renaud MC, Têtu B, Harel F, Roy M (2003) Laparoscopic sentinel node mapping in early-stage cervical cancer. Gynecol Oncol 91(3):494–503
Lécuru F, Mathevet P, Querleu D, Leblanc E, Morice P, Daraï E, Marret H, Magaud L, Gillaizeau F, Chatellier G, Dargent D (2011) Bilateral negative sentinel nodes accurately predict absence of lymph node metastasis in early cervical cancer: results of the SENTICOL study. J Clin Oncol 29(13):1686–1691. https://doi.org/10.1200/JCO.2010.32.0432 (Epub 2011 Mar 28)
Stegeman M, Louwen M, van der Velden J, ten Kate FJ, den Bakker MA, Burger CW, Ansink AC (2007) The incidence of parametrial tumor involvement in select patients with early cervix cancer is too low to justify parametrectomy. Gynecol Oncol 105(2):475–480 (Epub 2007 Feb 9)
Vercellino GF, Koehler C, Erdemoglu E, Mangler M, Lanowska M, Malak AH, Schneider A, Chiantera V (2014) Laparoscopic pelvic lymphadenectomy in 32 pregnant patients with cervical cancer: rationale, description of the technique, and outcome. Int J Gynecol Cancer 24(2):364–371. https://doi.org/10.1097/igc.0000000000000064
Marnitz S, Köhler C, Roth C, Füller J, Hinkelbein W, Schneider A (2005) Is there a benefit of pretreatment laparoscopic transperitoneal surgical staging in patients with advanced cervical cancer? Gynecol Oncol 99(3):536–544 (Epub 2005 Aug 29)
Zaal A, Zweemer RP, Zikán M, Dusek L, Querleu D, Lécuru F, Bats AS, Jach R, Sevcik L, Graf P, Klát J, Dyduch G, von Mensdorff-Pouilly S, Kenter GG, Verheijen RH, Cibula D (2014) Pelvic lymphadenectomy improves survival in patients with cervical cancer with low-volume disease in the sentinel node: a retrospective multicenter cohort study. Int J Gynecol Cancer 24(2):303–311. https://doi.org/10.1097/igc.0000000000000043
Holman LL, Levenback CF, Frumovitz M (2014) Sentinel lymph node evaluation in women with cervical cancer. J Minim Invasive Gynecol 21(4):540–545. https://doi.org/10.1016/j.jmig.2013.12.095 (Epub 2014 Jan 7)
Bats AS, Frati A, Mathevet P, Orliaguet I, Querleu D, Zerdoud S, Leblanc E, Gauthier H, Uzan C, Deandreis D, Darai E, Kerrou K, Marret H, Lenain E, Froissart M, Lecuru F (2015) Contribution of lymphoscintigraphy to intraoperative sentinel lymph node detection in early cervical cancer: analysis of the prospective multicenter SENTICOL cohort. Gynecol Oncol 137(2):264–269. https://doi.org/10.1016/j.ygyno.2015.02.018 (Epub 2015 Feb 26)
Rob L, Robova H, Halaska MJ, Hruda M, Skapa P (2013) Current status of sentinel lymph node mapping in the management of cervical cancer. Expert Rev Anticancer Ther 13(7):861–870. https://doi.org/10.1586/14737140.2013.811147
Cibula D, Abu-Rustum NR, Dusek L, Slama J, Zikán M, Zaal A, Sevcik L, Kenter G, Querleu D, Jach R, Bats AS, Dyduch G, Graf P, Klat J, Meijer CJ, Mery E, Verheijen R, Zweemer RP (2012) Bilateral ultrastaging of sentinel lymph node in cervical cancer: Lowering the false-negative rate and improving the detection of micrometastasis. Gynecol Oncol 127(3):462–466. https://doi.org/10.1016/j.ygyno.2012.08.035 (Epub 2012 Aug 31)
Salvo G, Ramirez PT, Levenback CF, Munsell MF, Euscher ED, Soliman PT, Frumovitz M (2017) Sensitivity and negative predictive value for sentinel lymph node biopsy in women with early-stage cervical cancer. Gynecol Oncol 145(1):96–101. https://doi.org/10.1016/j.ygyno.2017.02.005 (Epub 2017 Feb 8)
Narayan K, Lin MY (2015) Staging for cervix cancer: role of radiology, surgery and clinical assessment. Best Pract Res Clin Obstet Gynaecol 29(6):833–844. https://doi.org/10.1016/j.bpobgyn.2015.01.005 (Epub 2015 Mar 4)
Van Oostrum NH, Makar AP, Van Den Broecke R (2012) Sentinel node procedures in gynecologic cancers: an overview. Acta Obstet Gynecol Scand 91(2):174–181. https://doi.org/10.1111/j.1600-0412.2011.01302.x (Epub 2011 Dec 20)
Diaz JP, Gemignani ML, Pandit-Taskar N, Park KJ, Murray MP, Chi DS, Sonoda Y, Barakat RR, Abu-Rustum NR (2011) Sentinel lymph node biopsy in the management of early-stage cervical carcinoma. Gynecol Oncol 120(3):347–352. https://doi.org/10.1016/j.ygyno.2010.12.334 (Epub 2011 Jan 8)
Puente R, Guzman S, Israel E, Poblete MT (2004) Do the pelvic lymph nodes predict the parametrial status in cervical cancer stages IB-IIA? Int J Gynecol Cancer 14(5):832–840
Slama J, Dundr P, Dusek L, Fischerova D, Pinkavova I, Zikan M, Vrzackova P, Kojanova M, Cibula D (2012) Sentinel lymph node status in patients with locally advanced cervical cancers and impact of neoadjuvant chemotherapy. Gynecol Oncol 125(2):303–306. https://doi.org/10.1016/j.ygyno.2012.02.010 (Epub 2012 Feb 14)
Covens A, Rosen B, Murphy J, Laframboise S, DePetrillo AD, Lickrish G, Colgan T, Chapman W, Shaw P (2002) How important is removal of the parametrium at surgery for carcinoma of the cervix? Gynecol Oncol 84(1):145–149
Smith B, Backes F (2015) The role of sentinel lymph nodes in endometrial and cervical cancer. J Surg Oncol 112(7):753–760. https://doi.org/10.1002/jso.24022 (Epub 2015 Sep 9)
Roy M, Bouchard-Fortier G, Popa I, Grégoire J, Renaud MC, Têtu B, Plante M (2011) Value of sentinel node mapping in cancer of the cervix. Gynecol Oncol 122(2):269–274. https://doi.org/10.1016/j.ygyno.2011.04.002 (Epub 2011 Apr 29)
Sagae S, Monk BJ, Pujade-Lauraine E, Gaffney DK, Narayan K, Ryu SY, McCormack M, Plante M, Casado A, Reuss A, Chávez-Blanco A, Kitchener H, Nam BH, Jhingran A, Temkin S, Mileshkin L, Berns E, Scholl S, Doll C, Abu-Rustum NR, Lecuru F, Small W Jr, Gynecologic Cancer InterGroup Cervix Cancer brainstorming day (2016) Advances and concepts in cervical cancer trials: a road map for the future. Int J Gynecol Cancer. 26(1):199–207. https://doi.org/10.1097/igc.0000000000000587
Marchiolé P, Buénerd A, Benchaib M, Nezhat K, Dargent D, Mathevet P (2005) Clinical significance of lympho vascular space involvement and lymph node micrometastases in early-stage cervical cancer: a retrospective case-control surgico-pathological study. Gynecol Oncol 97(3):727–732
Cibula D, Abu-Rustum NR, Dusek L, Zikán M, Zaal A, Sevcik L, Kenter GG, Querleu D, Jach R, Bats AS, Dyduch G, Graf P, Klat J, Lacheta J, Meijer CJ, Mery E, Verheijen R, Zweemer RP (2012) Prognostic significance of low volume sentinel lymph node disease in early-stage cervical cancer. Gynecol Oncol 124(3):496–501. https://doi.org/10.1016/j.ygyno.2011.11.037 (Epub 2011 Nov 25)
Cormier B, Diaz JP, Shih K, Sampson RM, Sonoda Y, Park KJ, Alektiar K, Chi DS, Barakat RR, Abu-Rustum NR (2011) Establishing a sentinel lymph node mapping algorithm for the treatment of early cervical cancer. Gynecol Oncol 122(2):275–280. https://doi.org/10.1016/j.ygyno.2011.04.023 (Epub 2011 May 13)
Lee YS, Rhim CC, Lee HN, Lee KH, Park JS, Namkoong SE (2007) HPV status in sentinel nodes might be a prognostic factor in cervical cancer. Gynecol Oncol 105(2):351–357 (Epub 2007 Feb 2)
Slama J, Dundr P, Dusek L, Cibula D (2013) High false negative rate of frozen section examination of sentinel lymph nodes in patients with cervical cancer. Gynecol Oncol 129(2):384–388. https://doi.org/10.1016/j.ygyno.2013.02.001 (Epub 2013 Feb 8)
Altgassen C, Hertel H, Brandstädt A, Köhler C, Dürst M, Schneider A, AGO Study Group (2008) Multicenter validation study of the sentinel lymph node concept in cervical cancer: AGO Study Group. J Clin Oncol 26(18):2943–2951. https://doi.org/10.1200/jco.2007.13.8933
Bats AS, Buénerd A, Querleu D, Leblanc E, Daraï E, Morice P, Marret H, Gillaizeau F, Mathevet P, Lécuru F, SENTICOL collaborative group (2011) Diagnostic value of intraoperative examination of sentinel lymph node in early cervical cancer: a prospective, multicenter study. Gynecol Oncol. 123(2):230–235. https://doi.org/10.1016/j.ygyno.2011.08.010 (Epub 2011 Sep 3)
Bats AS, Mathevet P, Buenerd A, Orliaguet I, Mery E, Zerdoud S, Le Frère-Belda MA, Froissart M, Querleu D, Martinez A, Leblanc E, Morice P, Daraï E, Marret H, Gillaizeau F, Lécuru F (2013) The sentinel node technique detects unexpected drainage pathways and allows nodal ultrastaging in early cervical cancer: insights from the multicenter prospective SENTICOL study. Ann Surg Oncol 20(2):413–422. https://doi.org/10.1245/s10434-012-2597-7 (Epub 2012 Aug 22)
Jewell EL, Huang JJ, Abu-Rustum NR, Gardner GJ, Brown CL, Sonoda Y, Barakat RR, Levine DA, Leitao MM Jr (2014) Detection of sentinel lymph nodes in minimally invasive surgery using indocyanine green and near-infrared fluorescence imaging for uterine and cervical malignancies. Gynecol Oncol 133(2):274–277. https://doi.org/10.1016/j.ygyno.2014.02.028 (Epub 2014 Feb 28)
Plante M, Touhami O, Trinh XB, Renaud MC, Sebastianelli A, Grondin K, Gregoire J (2015) Sentinel node mapping with indocyanine green and endoscopic near-infrared fluorescence imaging in endometrial cancer. A pilot study and review of the literature. GynecolOncol 137(3):443–447. https://doi.org/10.1016/j.ygyno.2015.03.004 (Epub 2015 Mar 11)
Andikyan V, Khoury-Collado F, Denesopolis J, Park KJ, Hussein YR, Brown CL, Sonoda Y, Chi DS, Barakat RR, Abu-Rustum NR (2014) Cervical conization and sentinel lymph node mapping in the treatment of stage I cervical cancer: is less enough? Int J Gynecol Cancer 24(1):113–117. https://doi.org/10.1097/IGC.0000000000000034
Garg G, Shah JP, Toy EP, Field JB, Bryant CS, Liu JR, Morris RT (2011) Intra-operative detection of nodal metastasis in early stage cervical cancer: a survey of the practice patterns of SGO members. Gynecol Oncol 121(1):143–147. https://doi.org/10.1016/j.ygyno.2010.12.337 (Epub 2011 Jan 26)
Author information
Authors and Affiliations
Contributions
GFV: idea, questionnaire editing, questionnaire editing revision, data collection, manuscript editing, table editing, manuscript revision; EE: data collection, manuscript revision; PL: data collection; MZM: data collection; RR: data collection; NAR: data collection, manuscript revision; MP: data collection, manuscript revision; FL: data collection, manuscript revision; SG: data collection; BJM: data collection, manuscript revision; SS: data collection, manuscript revision; MA: data collection; CD: data collection; MK: questionnaire and reminder posting, contact with centers, manuscript revision; MH: data collection; AMD: data collection; VC: data collection, manuscript revision; JS: questionnaire editing revision, data collection, manuscript revision.
Corresponding authors
Ethics declarations
Conflict of interest
No actual or potential conflict of interest in relation to this article exists. Specifically, Bradley Monk has consulted for Roche Inc, Genmab and Advaxis; other authors declare no conflicts of interest. Thanks to: Ione und Costas Tziouvas for their very precious help editing the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vercellino, G.F., Erdemoglu, E., Lichtenberg, P. et al. A GCIG international survey: clinical practice patterns of sentinel lymph node biopsies in cervical cancer. Arch Gynecol Obstet 300, 191–199 (2019). https://doi.org/10.1007/s00404-019-05164-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05164-2