Abstract
Purpose
To determine reference values for umbilical Doppler pulsatility index in fetuses with isolated two-vessel cord and to compare these values with standard umbilical Doppler pulsatility index curves from 23 to 40 gestational weeks.
Methods
A retrospective longitudinal cohort study was conducted between January 2014 and December 2017 in a tertiary referral hospital and included 62 pregnant women with isolated single umbilical artery (two-vessel cord) and 174 measurements. Only uncomplicated term pregnancies were included. A reference curve for umbilical Doppler pulsatility index was built up and compared with a standard curve commonly used for fetuses with three-vessel cord.
Results
Umbilical Doppler pulsatility index values were much lower than expected in cases with two-vessel cord compared to 3-vessel cord: mean of the regression equations was 1.02 ± 0.23 vs. 0.86 ± 0.19, respectively (p value < 0.001). This difference was quite constant across the gestational weeks considered, showing that the slopes of the two regressions were very similar.
Conclusion
Reference curves for umbilical Doppler pulsatility index in two-vessel cord pregnancies were determined. Pulsatility index values were significantly different compared with those commonly used for three-vessel cord. Using lower reference values for umbilical pulsatility index in cases with two-vessel cord may allow a better identification of fetuses affected with intrauterine growth restriction, thus improving fetal surveillance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence of pregnancies with two-vessel cord (2VC) is about 1% (0.5–2%) in the general population [1, 2] and today is a common finding at routine first trimester scan [3,4,5]. Several studies have pointed out the correlation between the presence of 2VC and an increased risk for intrauterine growth restriction (IUGR), preterm birth, fetal anomalies, and stillbirth [6,7,8,9]. However, a normal outcome can be observed in many fetuses with isolated 2VC [10,11,12].
It seems important to discuss the role of velocimetry Doppler in these fetuses that are commonly considered at increased risk for perinatal complications [13]. Previous studies have reported that umbilical artery pulsatility index (PI) values are lower in fetuses with 2VC compared with normal fetuses [14,15,16]; these results may be explained by the assumption that a single artery carries twice the blood volume of a twin artery in a three-vessel cord (3VC) [17]. This brings to the conclusion that normal value ranges for 2VC fetuses have to be considered different from those in fetuses with 3VC.
The aim of our study was to assess new reference curves for umbilical artery Doppler PI in a population of fetuses with isolated 2VC and to compare them with reference ranges used in the common practice for normal fetuses.
Materials and methods
Study design
This was a retrospective longitudinal cohort study. The database of our ultrasound Center was searched for cases with isolated 2VC referred to our tertiary hospital between January 2014 and December 2017. In this period, 62 normal pregnancies between 23 and 40 weeks of gestation and 174 measurements were retrieved. A reference curve for umbilical Doppler PI was built up and compared with a standard curve commonly used for fetuses with 3VC [18]. The study was carried out following the ethical rules of Sant’ Orsola-Malpighi General Hospital, Bologna, Italy (the local ethics committee approval code is DBPP13EPP). A written consent form was obtained in each case.
Setting
Cases with isolated 2VC were retrieved from the database of the ultrasound laboratory at the Division of Prenatal Medicine Department of Medicine and Surgery (DIMEC) in a tertiary University Hospital of Bologna, Italy. Only uncomplicated term pregnancies were included. Pregnancy management was in accordance with the standard obstetric care and the treating obstetrician. Gestational age was determined by the measurement of fetal crown–rump length (CRL) at 11–13 weeks or fetal head circumference at 19–24 weeks.
Eligibility criteria were normal single pregnancy at term without any known maternal condition and no associated fetal anomaly. Ultrasound details were stored in the electronic database Viewpoint, GE Healthcare Italy. Information about pregnancy outcome was obtained through the examination of hospital records by an operator who was blinded to the Doppler results. Patients and general practitioners were contacted in case of missing information. Participants were excluded if a complete follow-up of the pregnancy was not available or, if any of the following conditions was found: multiple pregnancy, vanishing twin, sonographic suspicion of fetal anomaly, abnormal fetal karyotype, history of maternal disease or diabetes, chronic hypertension or preeclampsia, IUGR, drug abuse or smoking, perinatal death, emergency cesarean section due to intrapartum fetal distress, admission to Neonatal Intensive Care Unit (NICU).
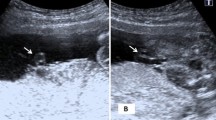
All ultrasound examinations were performed by two expert operators of our equipe (EC and IC) using a high-performance ultrasound machine equipped with color and pulsed Doppler (Voluson E8, Voluson 730 Expert, GE, Milan, Italy). According to standard technique, the umbilical artery blood velocity waveforms were sampled at the fetal end of the umbilical cord, with the vessel in longitudinal section and an angle of insonation close to zero. The same anatomical point was sampled in each case, thus reducing the variability of the repeated measurements at various gestational weeks and the interobserver variation. The first Doppler measurement was performed at 23–32 weeks (mean 27). The examination was repeated at least twice from each patient (median 3), every 2–5 weeks until delivery, for a total of 174 observations.
Statistical analysis
Sample size
Power analysis for a comparison of 2 independent means of regression was performed using Power Analysis Sample Size (PASS) software (Kaysville, UT, USA). Power analysis was conducted before the enrollment started. We estimated that a total of 58 and 174 cases (given the sample allocation ratio = 1:3), an umbilical artery PI Doppler coefficient of variation of SD/mean = 0.25 (as calculated by published data), would be needed to detect an absolute increase in the primary outcome measure (PI in 2VC) of 10% between groups, with a type I error of 5% and a power of 80%.
Statistics
The reference curve for 3VC proposed by Acharya [18] that used 513 observations in 130 lowrisk pregnancies was used as a term of comparison. We adopted the Acharya’s data [18], since the Doppler values of the fetal end, that were those used in our study, are reported. We regressed the mean values and the standard deviations (calculated by interquartile range/1.35) to obtain mean and standard deviation equations. Finally, we simulated a normal random variable for the umbilical Doppler PI values having 504 observations from 23 to 40 weeks of gestation. Umbilical Doppler PI was considered the dependent variable of the study.
Univariable analysis
The intraobserver and interobserver repeatabilities of the measurements were examined using intraclass correlation coefficients (ICCs) and their 95% confidence levels (CLs). An overlap between the 95% CIs of two ICC indicated no significant difference between them.
Simple linear regression was used to evaluate the relationship between gestational age and Doppler. Both linear and Log10 model were used. In addition, curves of the 95th centiles for both 3VS and 2VC were calculated. Student t test was used to evaluate the differences of the slopes and the intercepts of the two regression lines (3VC vs. 2VC) as reported by Glantz and Slinker [19].
Multivariable analysis
A general linear model (GLM) was used to better explore the differences between the two curves and their possible interaction.
To provide robust and unbiased estimates of means, standard errors and confidence intervals for the above mentioned performance measures, we internally validated the models using the standard SPSS bootstrap method with 1000 bootstrap samples with 95% confidence interval.
SPSS software was used for the statistical analyses (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY, USA).
Results
In 62 cases with 2VC a total of 174 observations were recorded, with a median of 3 (range 2–10) measurements per woman. Demographic details of the population are reported in Table 1. As shown, no differences were reported for maternal and neonatal characteristics.
The mean gestational weeks of the two regressions were 31.5 ± 5.1 for the 3VC and 30.8 ± 3.9 for the 2VC (p value = 0.149). At the mean gestational week, the mean PI values were 1.02 ± 0.23 and 0.86 ± 0.19, respectively (p value < 0.001). Interestingly, the quoted mean value of regression for 3VC at the mean gestational week was exactly that reported in the original paper by Acharya [18].
An overlap between the 95% CIs of the ICCs was found to be 0.93 (0.86–0.96), p value < 0.001 and 0.90 (0.80–0.95), and p value < 0.001 for interobserver and intraobserver repeatabilities, respectively.
Table 2 reports the simple linear and Log10 regressions output. No substantial fitting differences were found between linear and Log10 data transformation. Student t test [19] showed that the only difference between 3 and 2VC regression was detected for the comparison of the intercepts (p value < 0.001), being, instead, the slopes statistically equal for the two groups (p value = 1.00). Consequently, throughout the time window considered the difference in Doppler PI values was constantly of -20% about.
Bootstrap analysis on 1000 samples confirmed the results. The GLM did not detect any interaction effect between gestational age and 2VC vs. 3VC curves, maybe because all the pregnancies here considered were normal without any clinical complication including preeclampsia and/or IUGR. Since the GLM yielded redundant results, its output has been omitted, but is available from the authors. Figure 1 reports the umbilical-PI Doppler values plotted against the weeks of gestation at the time of measurements and stratified according to the group of interest (3VC and 2VC). As shown at peer gestational ages, the mean estimated umbilical-PI Doppler values are lower than expected for the 2VC group (solid lines). Finally, the 95th centiles of the two curves (dotted lines) are also reported. Interestedly, at 40 gestational weeks, the 95th centile for 2VC curve is quite similar to the mean quoted value for 3VC curve.
Discussion
Umbilical artery Doppler is nowadays commonly used in fetal well-being monitoring, especially in small for gestational age (SGA) fetuses. In this study, we have built new references ranges valid for fetuses with umbilical two-vessel cord, comparing them with the normal curves used in three-vessel cord. For comparison purposes, we preferred to use data from the medical literature instead from our own cohort of three-vessel cord cases, so to obtain more generalized results with a possible better impact for a routinely use of our curves.
We found that, as demonstrated in the previous studies [14, 15], umbilical Doppler PI values in cases with isolated 2VC were about 20% lower than those expected for normal fetuses with 3VC. This difference was quite constant across the gestational weeks considered, showing that the slopes of the two regressions were very similar.
The assumption at the basis of our study is that in cases with 2VC, a single umbilical artery (instead of two) carries the fetal blood flow, with a larger diameter and a lower impedance to flow.
The logical consequence of this finding is that using normal PI reference range for fetal with single umbilical artery may not be appropriate, hiding cases with increased impedance to flow with potential worse outcome.
Other papers, as previously said, have reported the result of a lower value of umbilical Doppler PI values in comparison with normal fetuses [14, 15], with smaller sample size. Our results seem, however, different from the other studies in the literature for various reasons: first of all, we took the umbilical PI value at the fetal end of the umbilical cord and not in a free loop, also standardizing the sonographic technique (longitudinal section of the vessel sampled) and thus vanishing the differences in resistance existing along the cord. Moreover, we did not match our cases with controls, but with a validated standard curve commonly used for fetuses with 3VC, thus reducing the selection bias. The two series of values are different at each gestational age (from 23 to 40), confirming the original hypothesis.
Strength of the study
This was a precise picture of all umbilical Doppler PI measurements in cases with isolated 2VC with uncomplicated pregnancy in a large tertiary center over a 4-year period. We chose a low-risk maternal population to exclude possible confounders. We measured the PI using the same strict technique to standardize the method between different operators and to have a better reliability in the repeated measurements.
Limit of the study
We acknowledge some limitations of our study. We used simulated, but robust, data from the literature to compare our results. Using fitted data usually smaller standard deviations are estimated, yielding more optimistic results. Again, no covariates can be added and not random effect can be estimated. It is, therefore, possible that our results are overestimated. We, however, detected a very substantial difference that surely would justify the use of custom curves to estimate 2VC fetuses.
Conclusions
In conclusion, normal PI values in cases with 2VC are 20% lower than those expected for normal fetuses with 3VC, with a parallel trajectory in the time window here considered. Further studies would evaluate if the customized curves could improve our recognition of fetuses at risk, mainly among those with normal weight but with Doppler PI values outside the 95th centile obtained in our study.
References
Parilla BV, Tamura RK, MacGregor SN, Geibel LJ, Sabbagha RE (1995) The clinical significance of a single umbilical artery as an isolated finding on prenatal ultrasound. Obstet Gynecol. 85:570–572
Hua M, Odibo AO, Macones GA, Roehl KA, Crane JP, Cahill AG, et al (2010) Single umbilical artery and its associated findings. Obstet Gynecol 115:930–934.
Martínez-Payo C, Cabezas E, Nieto Y, Azúa MRd, García-Benasach F, Iglesias E (v) Detection of single umbilical artery in the first trimester ultrasound: its value as a marker of fetal malformation. Biomed Res Int
ISUOG Practice Guidelines: performance of first-trimester fetal ultrasound scan UOG, vol 41 n, pp 102–113, 2013.
Lamberty CO, de Carvalho MHB, Miguelez J, Liao AW, Zugaib M (2011) Ultrasound detection rate of single umbilical artery in the first trimester of pregnancy. Prenat Diagn 31(9):865–868.
Jacques SA, Steven LW, David MS, Levy DL, Woods JR (1991) Value of a random single Doppler study of the umbilical artery for predicting perinatal outcome. J Ultrasound Med 10(6):337-339.
Pierce BT, Dance V, Wagner RK, Apodaca CC, Nielsen PE, Calhoun BC (2001) Perinatal outcome following fetal single umbilical artery diagnosis. J Matern Fetal Med 10:59–63
Murphy-Kaulbeck L, Doods L, Joseph KS, van den Hof M (2010) Single umbilical artery risk factors and pregnancy outcomes.Obstetr Gynecol 116(4):843–850.
Catanzarite VA, Hendricks S, Maida C, Westbrook C, Cousins L, Schrimmer D (1995) Prenatal diagnosis of the two-vessel cord: implications for patient counselling and obstetric management. Ultrasound Obstet Gynecol 5:98–105
Voskamp BJ, Fleurke-Rozema H, Oude-Rengerink K et al (2013) Relationship of isolated single umbilical artery to fetal growth, aneuploidy and perinatal mortality: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 42(6):622–628
Sterne GSL, Dubinsky TJ (2001) Abnormal fetal cerebral andumbilical Doppler measurements in fetuses with intrauterine growth restriction predicts the severity of perinatal morbidity.J Clin Ultrasound 29:146–151.
Chang CH, Chang F, Yu CH, Liang RI, Ko HC, Chen HY (2000) Systemic assessment of fetal hemodynamics by Doppler ultrasound. Ultrasound Med Biol 26:777–785
Gornall AS, Kurinczuk JJ, Konje JC (2003) Antenatal detection of a single umbilical artery: does it matter? Prenat Diagn 23:117–123.
Joel B, Adi YW, Yael S, Salvatore AM, Speigel E, Hershkovitz R (2015) Umbilical artery blood flows among pregnancies with single umbilical artery: a prospective casecontrol study. J Matern Fetal Neonatal Med 28(15):1803–1805.
Goldkrand JW, Pettigrew C, Lentz SU et al (2001) Volumetric umbilical artery blood flow: comparison of the normal versus the single umbilical artery cord. J Matern Fetal Med 10:116–121.
Hershkovitz R, Sheiner E, Mazor M (2006) Middle cerebral artery blood flow velocimetry among healthy fetuses with a single umbilical artery. J Ultrasound Med 25:1405–1408.
Sepulveda W, Peek MJ, Hassan J et al (1996) Umbilical vein to artery ratio in fetuses with single umbilical artery. Ultrasound Obstet Gynecol 8:23–26.
Acharya G, Wilsgaard T, Berntsen GK, Maltau JM, Kiserud T(2005) Reference ranges for serial measurements of blood velocity and pulsatility index at the intra-abdominal portion, and fetal and placental ends of the umbilical artery. Ultrasound Obstet Gynecol 26(2):162–169.
Glantz SA, Slinker BK (1990) Primer of applied regression and analysis of variance 1st edition
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
EC: protocol/project development, data collection, and manuscript writing. IC: data collection. DM: protocol/project development, data collection, and manuscript writing. AF: protocol/project development, data collection, manuscript writing, and data analysis.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Sant’Orsola Malpighi Hospital Bologna, Italy and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Contro, E., Cataneo, I., Morano, D. et al. Reference charts for umbilical Doppler pulsatility index in fetuses with isolated two-vessel cord. Arch Gynecol Obstet 299, 947–951 (2019). https://doi.org/10.1007/s00404-019-05086-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05086-z