Abstract
Purpose
The aim of the study was to identify risk factors associated with postoperative urinary tract infections (UTIs) following hysterectomy-based surgical staging in women with endometrial cancer.
Methods
This is a retrospective study utilizing an institutional database (2008–2016) of stage I–IV endometrial cancer cases that underwent hysterectomy-based surgery. UTIs occurring within a 30-day time period after surgery were examined and correlated to patient clinico-pathological demographics.
Results
UTIs were observed in 44 (6.4%, 95% confidence interval 4.6–8.2) out of 687 cases subsequent to the diagnosis of endometrial cancer. UTI cases were significantly associated with obesity, advanced stage, prolonged operative time, hysterectomy type, pelvic lymphadenectomy, non-β-lactam antibiotics, and intraoperative urinary tract injury (all, p < 0.05). On multivariate analysis, three independent risk factors were identified for UTIs: prolonged operative time [odds ratio (OR) 3.36, 95% CI 1.65–6.87, p = 0.001], modified-radical/radical hysterectomy (OR 5.35, 95% CI 1.56–18.4, p = 0.008), and an absence of perioperative β-lactam antibiotics use (OR 3.50, 95% CI 1.46–8.38, p = 0.005). In a predictive model of UTI, the presence of multiple risk factors was associated with significantly increased risk of UTI: 4.1% for the group with no risk factors, 7.3–12.5% (OR 1.85–3.37) for single risk factor group, and 30.0–30.8% (OR 10.1–10.5) for two risk factor group.
Conclusion
Urinary tract infections are common in women following surgical treatment for women with endometrial cancer with risk factors being a prolonged surgical time, radical hysterectomy, and non-guideline perioperative anti-microbial agent use. Consideration of prophylactic anti-microbial agent use in a high-risk group of postoperative urinary tract infection merits further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infections (UTIs) are a common reason for postoperative infectious complications in cancer patients [1, 2]. UTIs are associated with prolonged hospital stay, increased cost of care, and increased postoperative morbidity [3, 4]. The incidence of infectious complications in the perioperative period is known to be particularly elevated in cancer patients—a fourfold greater incidence than that seen in non-cancer populations [5].
Endometrial cancer is the most prevalent gynecologic malignancy in the United States, with an estimated 61,380 new cases and 10,920 deaths in 2017 [6]. The majority of patients are diagnosed with early-stage disease and undergo hysterectomy-based staging surgery with bilateral salpingo-oophorectomy and probable lymphadenectomy. Recently, there has been a paradigm shift of surgical procedures for endometrial cancer from standard laparotomy to minimally invasive surgery (MIS) [7, 8]. MIS, including robot-assisted procedures, has shown to lower complication rates and shorten hospitalizations compared to standard laparotomy, but with prolonged operative times [7]. The incidence of infectious complications after lengthy surgery is known to be elevated, and can be life-threatening in the perioperative period [9].
The factors associated with an increased risk of postoperative UTIs in women with endometrial cancer are not well described. Given that 7–13% of patients who undergo hysterectomy-based staging surgery are readmitted, and UTIs are one of the most common reasons for readmission, identification of UTI risk factors could improve postoperative management of endometrial cancer patients [10, 11]. The object of this study was to identify risk factors for postoperative UTIs in women with endometrial cancer.
Materials and methods
Study design and eligibility
After institutional review board (IRB) approval at the University of Southern California, endometrial cancer cases were identified using an institutional database. Eligibility criteria included consecutive cases of women with stage I–IV endometrial cancer who underwent hysterectomy-based surgical staging at Los Angeles County Medical Center and Keck Medical Center of the University of Southern California between January 2008 and February 2016. Exclusion criteria included women who did not undergo staging surgery, cases of uterine sarcomas, and endometrial hyperplasia. Eligible cases were divided into two groups: patients with a diagnosis of postoperative UTIs and patients without postoperative UTIs. For strengthening the reporting of observational studies in epidemiology (STROBE), guidelines were consulted for outlining the results of this retrospective cohort study [12]. Some of the patients included in prior studies [13, 14].
Clinical information
Archived medical records were reviewed to extract clinical information for eligible cases: (1) patient demographics at the time of surgery, including age, ethnicity, body mass index (BMI, kg/m2), American Society of Anesthesiologists Physical Status (ASA-PS), presence of medical comorbidities (diabetes mellitus, hypertension, and hypercholesterolemia), and cigarette smoking; (2) tumor characteristics, including uterine weight (grams), tumor size (cm), cancer stage, histologic subtype, tumor grade, depth of myometrial invasion (%), and lymph-vascular space invasion (LVSI); (3) treatment pattern, including operating time (min), estimated blood loss (EBL, mL), surgical staging details (minimally invasive surgery, type of hysterectomy, and lymphadenectomy), intraoperative cystoscopy, and ureteral stent insertion; (4) complications in perioperative period, including blood transfusion (≥5 units), urinary injury, vascular injury, bowel injury, hospital stay (day), wound infection including surgical site fascial deficiency or evisceration, readmission, sepsis, venous thromboembolism, and death; (5) characteristics relating to UTIs, including symptoms, type of prophylactic antibiotics before and during surgery, urine pathogens, and sensitivity for prophylactic antibiotics; and (6) survival outcomes, including disease-free survival (DFS) and overall survival (OS).
Study definitions
A UTI was defined as a patient with UTI symptoms and (1) a culture with >103 colonies/mL of uropathogens with urinary catheters, (2) a culture with >105 colonies/mL of uropathogens regardless of using urinary catheters, (3) a positive gram stain, or (4) a clinical diagnosis. These were based on prior manners [15, 16]. All cases of UTIs diagnosed within 30 days of the primary staging surgery were included in this study [17]. Prophylactic antibiotics were categorized based on American College of Obstetrics and Gynecology (ACOG) guidelines: β-lactam antibiotics (cephalosporin 1–2 generation), β-lactam alternatives (clindamycin and gentamicin), and non-standard antibiotics (clindamycin alone, ciprofloxacin alone, and other regimens) [18]. Stage for endometrial cancer was reclassified based on the 2009 International Federation of Gynecology and Obstetrics (FIGO) system. Histologic subtypes were divided into endometrioid and non-endometrioid. Minimally invasive surgery included robotic-assisted hysterectomy. Hysterectomy types were grouped into total simple hysterectomy and modified-radical hysterectomy/radical hysterectomy. Urinary stents were inserted before and during surgery. Postoperative complications were defined as occurring within 30 days from the hysterectomy-based surgical staging.
Statistical analysis
The primary interest of this analysis was to examine the prevalence of UTIs after hysterectomy-based surgical staging and the independent risk factors for UTIs in women with endometrial cancer. The secondary interest of analysis was to design a predictive model for UTIs in this population.
Continuous variables were examined for normality by Kolmogorov–Smirnov test and expressed with mean [±standard deviation (SD)] or median (range) as appropriate. Student’s t test or Mann–Whitney U test was used to assess statistical significance for continuous variables. Clinically relevant age cut-off (<60 vs. ≥60 years), the World Health Organization definition for BMI (<30, 30–39.9 ≥40 kg/m2), surgical operating time (<300 vs. ≥300 min), estimated blood loss (<2000 vs. ≥2000 mL), and median time for hospital stay (0–3 vs. <3 days) were used for the cut-off values and selected in an priori manner [9, 19, 20]. Pearson’s correlation coefficient value was determined among the continuous variables. Categorical variables were evaluated using Fisher’s exact test or the Chi-squared test as appropriate.
A binary logistic regression model was used to identify independent contributing factors for postoperative UTIs. Significant covariates with p < 0.10 in univariate analysis were initially entered into the multivariate model; then, the least significant covariate was removed from the model until the final model retained significant covariates (conditional backward method). Magnitudes of statistical significance were expressed with adjusted odds ratio (OR) and 95% confidence interval (CI). Statistical significance of survival analysis was performed using the Log-rank test. The Kaplan–Meier method was used to construct survival curves. A p value of less than 0.05 was considered statistically significant (all, two-tailed hypothesis). The Statistical Package for Social Science software (version 24.0, Chicago, IL, USA) was used for all analyses.
Results
There were 687 cases of endometrial cancer that underwent hysterectomy-based surgical staging during the study period. Postoperative UTIs were observed in 44 (6.4%, 95% CI 4.6–8.2) cases. Patient demographics comparing postoperative UTI cases (n = 44) and non-UTI cases (n = 643) are shown in Table 1. Across the two groups, the majority of women with endometrial cancer were less than 60 years old (62.3%), Hispanic ethnicity (59.0%), and obese (BMI ≥ 30 kg/m2, 63.2%). Approximately, half of the patients had severe systemic diseases (ASA score 3–4, 43.2%) and hypertension (53.7%). One-third of the patients had comorbidities: diabetes mellitus (32.0%) and hypercholesterolemia (30.4%). Patient’s age, ethnicity, BMI, ASA score, comorbidity rates, and cigarette smoking rates were similar between the groups with and without postoperative UTIs (all, p > 0.05).
Tumor characteristics were compared between the two groups (Table 2). The majority consisted of stage I (78.5%), endometrioid histology (83.2%), and low-grade tumor (76.3%). Tumor size, uterus size, histologic subtypes, tumor grade, deep myometrial invasion rates, and lymphovascular space invasion rates were similar between the two groups (all, p > 0.05). Advanced stage cases were significantly associated with postoperative UTIs compared to early-stage cases (10.8 vs. 5.2%, OR 2.21, 95% CI 1.16–4.21, p = 0.02).
Treatment patterns for endometrial cancer and perioperative complications were also compared between the two groups (Table 3). The majority underwent minimally invasive surgery (61.1%), simple hysterectomy (97.4%), intraoperative cystoscopy (64.9%), and received β-lactam antibiotics (88.9%). Readmissions were observed in 25 (3.6%) cases. Postoperative UTIs were associated with prolonged operative time (≥300 min, 10.7%), modified-radical/radical hysterectomy (22.2%), β-lactam alternatives (15.2%), and intraoperative urinary injury (38.5%) in univariate analysis (p < 0.05). Minimally invasive surgery and cystoscopy use during surgery were not associated with increased risk of postoperative UTIs (p > 0.10). Postoperative UTIs significantly correlated with longer hospital stay (OR 2.43, 95% CI 1.31–4.50, p = 0.005) and other postoperative complications, including readmission (OR 3.99, 95% CI 1.42–11.2, p = 0.009) and sepsis (OR 11.7, 95% CI 2.53–54.0, p = 0.002).
Prophylactic antibiotics given at the time of surgery and urine pathogens collected at the time of UTI diagnosis are shown in Table 4. The most common prophylactic antibiotics were cefoxitin (50.0%) followed by cefazolin (27.3%) and clindamycin and gentamycin (11.4%). Among the detected cases, more than a half of microorganisms showed a resistance to prophylactic antibiotics (60.6%). The median onset of UTIs was on postoperative day 7 (range 1–26). The most frequently isolated uropathogens were Escherichia Coli (36.4%) followed by Enterococcus species (16.3%), Klebsiella pneumonia (9.1%), and Pseudomonas aeruginosa (9.1%). The common symptoms of UTIs were dysuria (36.4%), high fever (27.3%), abdominal or back pain (18.2%), and urinary frequency (11.4%).
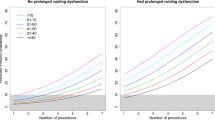
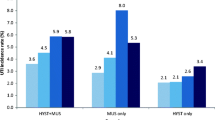
Multivariate analysis was performed to determine independent risk factors associated with postoperative UTIs (Table 5). There were three independent risk factors identified in the analysis. These included non-β-lactam antibiotics (adjusted OR 3.50 95% CI 1.46–8.38, p = 0.005), prolonged operative time (≥300 min, adjusted OR 3.36 95% CI 1.65–6.87, p = 0.001), and modified-radical/radical hysterectomy (adjusted OR 5.35 95% CI 1.56–18.4, p = 0.008). The relative contribution of these three independent risk factors was examined to predict the risk of postoperative UTIs (Fig. 1). The risk of postoperative UTIs rose dramatically with an increasing number of risk factors (none 4.1%, one risk factor 8.1%, and two risk factors 30.4%, p < 0.05). The combination of risk factors associated with the highest prevalence of postoperative UTIs was operating time ≥300 min and non-β-lactam prophylactic antibiotics (50.0%).
Perioperative mortality rate (death occurring within 30 days of surgery) was observed in one case (0.2%, 95% CI 0–0.4) and was similar between the patients who developed postoperative UTIs and patients without postoperative UTIs (p = 0.99). Venous thromboembolism was the immediate cause of death. In survival analysis, postoperative UTIs were not associated with decreased disease-free survival (median time, 17.0 vs. 20.4 months; p = 0.37) or overall survival (median time, 18.8 vs. 22.1 months; p = 0.55) compared to without postoperative UTI group.
Predictive model of UTI in endometrial cancer. Risk of postoperative urinary tract infection based on individual number of risk factors. Prevalence and odds ratio for UTI are shown based on the number of independent risk factors (operating time ≥300 min, non-β-lactam prophylaxis antibiotics use, modified-radical/radical hysterectomy type, p < 0.01)
Discussion
The key findings of our study are that non-β-lactam antibiotic prophylaxis, prolonged operative time, and performance of modified-radical/radical hysterectomy are independent risk factors for postoperative UTIs in women with endometrial cancer. Multiple risk factors are associated with a markedly elevated risk of UTIs, suggesting a consideration of appropriate antibiotics prophylaxis in this cohort.
Perioperative complications and readmission costs are two important concerns for management of endometrial cancer. The rate of UTIs after conventional hysterectomies is reported to be approximately 0.5–4.2% in benign gynecological disease [9, 21, 22]. In our study, the rate of UTIs after hysterectomy-based staging surgery in women with endometrial cancer was 7.1%, which is relatively higher than the rates of prior studies in benign disease. Moreover, this risk correlated with other postoperative complications, including sepsis and readmission in the perioperative period. Readmission after surgery has been shown to increase the cost after surgery. Previous studies showed patients with complications in perioperative period had higher total charges than patients with no complications ($64,792 vs. $39,064), and the median cost for readmission was $9774 in women with endometrial cancer [11, 23]. Several studies have demonstrated that hospital readmissions affect not only the cost of care, but also the quality of care delivered to patients [24, 25]. Reducing the incidence of postoperative UTIs can improve the quality of care for women with endometrial cancer and reduce the secondary complications and readmission costs.
Our study identified several independent prognostic factors for postoperative UTIs after hysterectomy-based surgical staging of endometrial cancer. First, non-β-lactam agents for anti-microbial prophylaxis were associated with increased risk of postoperative UTIs. A previous study shows that β-lactam antibiotics are associated with decreased rates of postoperative surgical site infections (SSIs) after conventional hysterectomy. In this study, patients receiving β-lactam alternatives and non-standard regimens had a significantly higher risk of SSIs [26]. Similarly, our study showed that non-β-lactam antibiotics are inferior in preventing postoperative UTIs compared to a standard β-lactam regimen. A possible explanation is that β-lactam antibiotics first generations, commonly used for surgical prophylaxis, are highly effective against Escherichia coli, Klebsiella pneumonia, and Proteus mirabilis, which are the predominant pathogens that cause UTIs [16, 27]. Given the risk of postoperative infections, steps should be taken to determine the veracity of any patient-reported penicillin allergies, and β-lactam antibiotics should be considered in appropriate cases. In cases of self-reported penicillin allergy, skin testing shows cross-reactivity with cephalosporins in only 10% of patients with a true penicillin allergy [28]. Additionally, cross-allergy is negligible with second- and third-generation cephalosporins [29]. Patients with negative results on penicillin skin testing and those without a history of anaphylactic reaction might be allowed to receive cephalosporins.
Second, prolonged operative time was associated with an increased incidence of postoperative UTIs. Prolonged operative time is known to increase postoperative infectious complications, especially surgical site infections. One study reported that postoperative UTIs correlate with operating time in gynecological surgery [9]. This association reflected to increased complexity of procedures that may result from increased uterine size, hysterectomy type, lymphadenectomy, lysis of adhesions, and conversion to laparotomy [24, 30, 31].
Third, modified-radical/radical hysterectomy had the greatest impact on the incidence for postoperative UTIs. These procedures seem to be associated with longer urinary catheterization and urinary stent placement. The protocols at our institution are to remove catheters on postoperative day 1 after a simple hysterectomy, postoperative days 5–7 after a modified-radical hysterectomy, and postoperative days 7–14 after a radical hysterectomy. The majority of patients without perioperative complications followed the protocol in this study. Several studies have shown that early removal of urinary catheters reduces UTI rates. For instance, enhanced recovery after surgery programs often included early catheter removal and reported a significantly reduced rate of postoperative UTIs [32]. In addition, the procedure of radical hysterectomy involves the potential for nerve injury and local inflammation, which may increase urinary retention after catheter removal.
Strengths of our study include the fact that we comprehensively evaluated the significance of postoperative urinary tract infections in a relatively large number of women with endometrial cancer. One of the limitations is the retrospective nature of this study that may miss potential confounding factors. For example, our patients may have visited or been readmitted at other local hospitals; thus, some data regarding symptoms or uropathogens would not be captured. Second, the antibiotic prophylaxis for hysterectomy procedures is commonly aimed at prevention of surgical site infections, not postoperative UTIs. In addition, a possible limitation in this study is that the majority of our cohort had stage I and low-grade endometrioid cancer, which is reflective of the relatively low incidence of disease mortality. Therefore, a type II error may occur when examining the relation between postoperative UTIs and survival outcomes.
Despite the limitations, our study identified several risk factors for UTIs after hysterectomy-based staging surgery in endometrial cancer. Accounting for these risk factors by adopting our predictive model of postoperative UTIs when determining whether to utilize longer-term antibiotic prophylaxis as well as proper selection of β-lactam candidates may improve patient outcomes and reduce the risk of readmission due to postoperative UTIs. Due to the costs associated with readmission resulting from postoperative UTIs, further studies regarding strategies to reduce postoperative UTIs with women in endometrial cancer may be warranted.
References
Matsuo K, Prather CP, Ahn EH et al (2012) Significance of perioperative infection in survival of patients with ovarian cancer. Int J Gynecol Cancer. 22:245–253
Horan TC, Culver DH, Gaynes RP et al (1993) Nosocomial infections in surgical patients in the United States, January 1986–June 1992. National Nosocomial Infections Surveillance (NNIS) System. Infect Control Hosp Epidemiol 14:73–80
Foxman B (2002) Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med 113(Suppl 1A):5s–13s
Wakeam E, Hyder JA, Lipsitz SR et al (2016) Hospital-level variation in secondary complications after surgery. Ann Surg 263:493–501
Williams MD, Braun LA, Cooper LM et al (2004) Hospitalized cancer patients with severe sepsis: analysis of incidence, mortality, and associated costs of care. Crit Care 8:R291–R298
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics. CA Cancer J Clin 67:7–30
Wright JD, Burke WM, Tergas AI et al (2016) Comparative effectiveness of minimally invasive hysterectomy for endometrial cancer. J Clin Oncol 34:1087–1096
Barnett JC, Judd JP, Wu JM et al (2010) Cost comparison among robotic, laparoscopic, and open hysterectomy for endometrial cancer. Obstet Gynecol 116:685–693
Catanzarite T, Saha S, Pilecki MA et al (2015) Longer operative time during benign laparoscopic and robotic hysterectomy is associated with increased 30-day perioperative complications. J Minim Invasive Gynecol 22:1049–1058
Liang MI, Rosen MA, Rath KS et al (2013) Reducing readmissions after robotic surgical management of endometrial cancer: a potential for improved quality care. Gynecol Oncol 131:508–511
Henretta MS, Scalici JM, Engelhard CL et al (2011) The revolving door: hospital readmissions of gynecologic oncology patients. Gynecol Oncol 122:479–483
von Elm E, Altman DG, Egger M et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335:806–808
Matsuo K, Moeini A, Cahoon SS et al (2016) Weight change pattern and survival outcome of women with endometrial cancer. Ann Surg Oncol 23:2988–2997
Matsuo K, Hom MS, Machida H et al (2017) Incidence of urinary tract injury and utility of routine cystoscopy during total laparoscopic hysterectomy for endometrial cancer. Eur J Obstet Gynecol Reprod Biol 213:141–142
Hooton TM, Bradley SF, Cardenas DD et al (2010) Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 50:625
Czaja CA, Scholes D, Hooton TM et al (2007) Population-based epidemiologic analysis of acute pyelonephritis. Clin Infect Dis 45:273–280
Bratzler DW, Dellinger EP, Olsen KM et al (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect 14:73–156
ACOG practice bulletin No. 104 (2009) Antibiotic prophylaxis for gynecologic procedures. Obstet Gynecol 113:1180–1189
Deurenberg P, Yap M, van Staveren WA (1998) Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord 22:1164–1171
Ramzan AA, Garcia-Sayre J, Hom MS et al (2015) Relative morbidity and mortality of panniculectomy-combined surgical staging in endometrial cancer. Int J Gynecol Cancer 25:1503–1512
Brummer TH, Jalkanen J, Fraser J et al (2011) FINHYST, a prospective study of 5279 hysterectomies: complications and their risk factors. Hum Reprod 26:1741–1751
Makinen J, Johansson J, Tomas C et al (2001) Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod 16:1473–1478
Chan JK, Gardner AB, Taylor K et al (2015) Robotic versus laparoscopic versus open surgery in morbidly obese endometrial cancer patients—a comparative analysis of total charges and complication rates. Gynecol Oncol 139:300–305
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 360:1418–1428
Lawson EH, Hall BL, Louie R et al (2013) Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg 258:10–18
Uppal S, Harris J, Al-Niaimi A et al (2016) Prophylactic antibiotic choice and risk of surgical site infection after hysterectomy. Obstet Gynecol 127:321–329
Echols RM, Tosiello RL, Haverstock DC et al (1999) Demographic, clinical, and treatment parameters influencing the outcome of acute cystitis. Clin Infect Dis 29:113–119
Anne S, Reisman RE (1995) Risk of administering cephalosporin antibiotics to patients with histories of penicillin allergy. Ann Allergy Asthma Immunol 74:167–170
Pichichero ME, Casey JR (2007) Safe use of selected cephalosporins in penicillin-allergic patients: a meta-analysis. Otolaryngol Head Neck Surg 136:340–347
Walker JL, Piedmonte MR, Spirtos NM et al (2009) Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol 27:5331–5336
O’Hanlan KA, McCutcheon SP, McCutcheon JG (2011) Laparoscopic hysterectomy: impact of uterine size. J Minim Invasive Gynecol. 18:85–91
Grant MC, Yang D, Wu CL et al (2017) Impact of enhanced recovery after surgery and fast track surgery pathways on healthcare-associated infections: results from a systematic review and meta-analysis. Ann Surg 265:68–79
Acknowledgements
The study was supported by the Ensign Endowment for Gynecologic Cancer Research (K.M.).
Author information
Authors and Affiliations
Contributions
KM: protocol/project development, data collection and data management, data analysis, manuscript writing and editing. HM: project development, data collection and data management, data analysis, manuscript writing and editing. MH, AS, and BG: protocol/project development, data collection and data management, manuscript writing and editing.
Corresponding author
Ethics declarations
Financial support
Ensign Endowment for Gynecologic Cancer Research (K.M.)
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All information in studies involving human participants was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Machida, H., Hom, M.S., Shabalova, A. et al. Predictive model of urinary tract infection after surgical treatment for women with endometrial cancer. Arch Gynecol Obstet 296, 335–343 (2017). https://doi.org/10.1007/s00404-017-4434-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4434-5