Abstract
Background
Dealing with work-related stress is highly prevalent for employees in Gynecology Medicine. Junior physicians, in particular, have to face high working demands and challenges while starting their medical career after graduation. Job resources (i.e., social support) and personal resources (coping skills) might reduce job strain. The evidence for supportive and effective mental health interventions for clinicians is limited. Offering psychosocial skill training for entrants in Gynecology Medicine is expected to be highly beneficial. Following this, the present pilot study focused on strengthening physicians’ psychosocial skills and analyzed the effects of innovative training for junior gynecologists working in German hospitals.
Methods
Coping skills training for junior gynecologists was offered as group training for 12 weekly sessions over a time period of 3 months. Physicians were randomized to either an intervention group (IG) receiving the training (n = 38) or a control group (CG; n = 40). Training content involved developing and learning coping skills as well as solution-focused and cognitive behavioral counselling for junior gynecologists. Study outcomes were (1) perceived occupational stress, (2) emotional exhaustion, (3) resilience coping behavior, (4) emotion regulation skills and (5) job satisfaction. Surveys were distributed at baseline (T0), after the training (T1), after 3 (T2) and 6 months (T3).
Results
Junior gynecologists (IG) reported a significant decrease in perceived job stress and emotional exhaustion from baseline to all follow-ups, whereas the control group did not show any comparable results. A clear positive value of the mental health promotion program was also noticeable with regard to job satisfaction and increased coping skills (i.e., emotion regulation). Overall satisfaction with the skill training was high: gynecologists reported high scores for training design, content, received outcome and overall satisfaction with the training.
Conclusions
In this pilot study, participating in a psychosocial skills training course adapted for gynecology clinicians was associated with reductions in perceived job stress, exhaustion and improvements in coping skills and satisfaction. Modified psychosocial skills training may be a time-efficient tool to support gynecologists in their performance and well-being, which may have positive implications for patient care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Starting a medical career in the field of Gynecology and Obstetrics is often mentioned as being stressful and characterized as a critical life event. Many junior gynecologists reported that they perceive high levels of job stress in combination with lots of job demands, few autonomy and control over their work as well as few relevant rewards [1, 2]. In addition, medical cases in gynecology frequently require dealing with problems that are dramatic and sometime unsolvable. In addition, there is a relatively high risk for gynecologists to be involved in problematic medical situations (bearing bad news in case of cancer, infertility, etc.) [3]. Junior physicians often complain they get only limited and unsatisfactory support from experienced colleagues of supervisors [4, 5]. Such situations are commonly accompanied by strong negative emotions and require effective coping strategies on how to regulate these emotions. However, this focus remains largely untargeted in medical school.
Consequences of these working environments are diverse. As previous research studies demonstrated gynecologists perceptions of their destructive working conditions and job satisfaction are correlated in a negative way [6]. Associations to decreased job performance and/or increased numbers of sick days have been stated [7]. In addition, symptoms of depression are common among young clinicians who report high rates of dissatisfaction [8].
High levels of working demands and efforts in the clinical setting in combination with low levels of support, feedback on their performance and autonomy make entrants in Gynecology and Obstetrics vulnerable for stress-related strain and rise concerns about their long-term mental health status and work ability [9, 10].
These issues are essential due to the fact that they may have negative consequences on quality of patient care and costly to health care organizations [11–13]. Given the effect of physician distress on quality of care and turnover, physicians and health care employers have a shared responsibility to promote junior clinicians performance and well-being [14].
As research demonstrated there is a strong relationship between physicians' job dissatisfaction and quality of patient care [15]. In addition, as reported by Hancke et al. gynecologists reported low levels of job satisfaction, dissatisfaction with their salary and quality of leadership as well as high levels of perceived work-family conflicts [16].
All in all, work flow and psychosocial work factors and relations to job satisfaction, turn over intentions and related distress are well analyzed; however, very limited research has been performed that actively address mental health promotion interventions to help and strengthen junior doctors’ performance and well-being during their first years at clinical practice in Gynecology Medicine.
The main aim of such interventions should be to improve and support individual and team skills as well as coping strategies on how to handle daily job demands, different work situations and balance between life domains. As a detailed explanation: individual coping strategies refer to the specific efforts, both behavioral and mental, that individuals can use to handle, tolerate, reduce stressful events [17].
Effectiveness of psychosocial skills trainings in different work settings have been verified in several research evaluations: improved outcome parameters include reduced stress perceptions, improved mental health (i.e., sleep quality) and higher levels of job performance [18–24].
For coping skills training the Lazarus transactional model of stress is a highly relevant and well-established theoretical model [25]. This model of stress highlights two coping strategies: problem-focused coping and emotion-focused coping. As a short definition, problem-focused coping includes to actively influence a stress situation in a positive way using cognitive or behavioral strategies. Such coping behavior has been proven to be successful in reducing mental stress and improving health related problems [26].
Emotion-focused coping primarily serves the function of handling difficult emotions such as anger, frustration, disappointment, and sadness in relation to the specific work problem [27].
Aim of this study
This pilot study focused on evaluating an innovative coping skills training for junior physicians in Gynecology and Obstetrics involving development of problem- and emotion-focused coping skills and cognitive behavioral as well as solution-focused counselling.
We hypothesized that this training would result in improved professionalism, job satisfaction and positively affect junior physician’s well-being and mental health, including reduced stress.
Study hypotheses
-
1.
Gynecologists in the intervention group score significantly lower in perceived stress and emotional exhaustion after the training compared to those in the control group.
-
2.
Gynecologists in the intervention group score significantly higher in work engagement after the training compared to those in the control group.
-
3.
Gynecologists in the intervention group score significantly higher in coping skills after the training compared to those in the control group.
Methods
Study design
In a two-arm randomized controlled trial junior physicians working in clinic departments of Gynecology and Obstetrics were divided into two groups: (1) intervention group (IG) and (2) control group (CG). The study flow is pictured in Fig. 1.
Recruitment of the study participants
Physicians working in clinic departments of Gynecology and Obstetrics Medicine were recruited from seven hospitals (five community based hospitals and two university hospitals) (see Table 1). Invitation was performed via e-mail, telephone and/or direct communication to contribute in the study. Inclusion criteria were (1) employment in Gynecology/Obstetrics, (2) being employed full time (3), a maximum of 2 years of working experience in Gynecology/Obstetrics (4) participation in the study during the next nine months (5) access to the internet and e-mail.
Randomization of the study participants
First, all included physicians answered the baseline questionnaire (t0); second the participants were randomized into two groups (intervention and control group). This procedure was supported by a computer generated list of numbers.
Coping skill training: elements and content of the intervention
The training was performed during a time span of 3 months to promote job performance and well-being in physicians and to reduce perceived distress. Each session lasted 1.5 h and was performed off duty.
This intervention involved the following methodological elements: discussion groups organized around a curriculum including elements of reflection, shared experience, and small-group learning among the physicians. Modules of the training sessions included psycho-education, theoretical input, watching videos, oral group discussions, experiential exercises, role plays. The training modules enclosed both well-established problem solving and emotion regulation strategies according to Lazarus’s transactional model of stress. The intervention design was based on this theoretical model [26]. The skills training was performed by certified occupational health psychologists; they had expertise in several stress management techniques, cognitive behavioral therapy as well as solution-focused training.
The training modules mainly focussed on situations and problems experienced at work. Practical implication including coping strategies (cognitive, emotional, external, support systems, etc.) were integrated. In detail, each training session had a special work-related topic: (1) introduction: opening and discussion on the theme "working as a gynecologist in the clinical setting", (2) and (3) experienced work-related problems (4) and (5) coping skills training (cognitive strategies, emotion regulation, and stress management techniques, self-awareness and resilience, (6) and (7) conflict management, analyzing conflict types and conflict handling in daily work routines, (8) receiving and giving feedback, asking for supervision and feedback, (9) communication training, (10) learning from mistakes, reporting, dealing with consequences, organizational hospital culture (11) handling difficult medical decisions, creating a support system, how to speak up to supervisors and senior physicians, (12) overall training evaluation. The CG received neither coping skills training nor any other comparable intervention (i.e., any other psychosocial skills training, counselling or therapy).
Assessment procedure
In the beginning, the participating gynecologists were requested to complete an online survey as a baseline assessment before the randomization. The overall outcome assessment was performed three times: (1) after the final session of the training (t1), after 3 month (t2) and after 6 month (t3). An external online survey collection service was used to get self-reports (using direct e-mail links for the access).
Outcome measures
The outcome variables included (1) perceived stress, (2) emotional exhaustion, (3) emotion regulation, (4) resilience and (5) job satisfaction.
Standardized and validated surveys were used for the outcome measurement: Perceived Stress Questionnaire (PSQ), Copenhagen Psychosocial Questionnaire (COPSOQ), Maslach Burnout Inventory (MBI) and Emotion Regulation Skills Questionnaire (ERSQ-27) and the Brief Resilient Coping Scale (BRCS).
The PSQ was used to measure perceived job related stress [28].
In total, four scales (worries, tension, demands, joy) with five items each are included in the PSQ. The included items can be answered with a four-point rating scale (1 = almost never, 2 = sometimes, 3 = often and 4 = usually).
Time of reference includes the period of the last month. Job satisfaction was measured with the job satisfaction scale in the Copenhagen Psychosocial Questionnaire (COPSOQ) [29, 30]. The scale has four items on a four-point Likert scale (very satisfied, satisfied, not satisfied and very dissatisfied). The quality criteria of the COPSOQ have been proofed and validated adequately [30].
A subscale of the Maslach Burnout Inventory (MBI-EE) with five items was used to measure emotional exhaustion (items range 1–6). The quality criteria of the MBI-EE have been validated sufficiently [31].
In addition, the validated Emotion Regulation Skills Questionnaire (ERSQ-27) was handed to evaluate emotion regulation. The included items included questions on comprehension (-C), acceptance (-A), and self-support (-SS) (nine items; range 0–4). Quality criteria were checked and fulfilled [32].
The German version of the ‘Brief Resilient Coping Scale’ (BRCS) was used to measure resilience coping behavior [33], which consists of four self-assessing items for resilient coping behavior in difficult or unpleasant situations in the past.
An additional questionnaire was developed and implemented to give grades for satisfaction with the overall course evaluation (1—very dissatisfied to 5—very satisfied).
Statistics
In the beginning, we proved whether the IG and CG differed in mean scores of the socio-demographic factors (i.e., age, etc.) or in the outcome parameters (e.g., perceived job stress) using t tests and Chi-square tests.
ANCOVA were used to analyze for differences in the outcome variables between IG and CG. Study outcome parameters were assessed before starting the training (baseline) and at three follow-up time points for both groups (IG and CG). Only gynecologists in the IG were included for the follow-up analyses who participated more than 80 % of the training sessions.
P values were adjusted with false discovery rate estimation procedure [34] to prove for an increased probability of Type I error due to multiple testing.
Moreover, we used and illustrated Cohen’s d with 95 % confidence intervals (CIs) by comparing the means and SDs of the intervention and control group. According to established statistical guide lines, the following effect sizes can be characterized: d = 0.2 as a small effect, d = 0.5 as a medium effect, and d = 0.8 as a large effect [35]. All statistical analyses were performed using the IBM SPSS Statistics Version 22.0.
A statistical power analysis was performed and showed that a sample size of 80 provides statistical power (two-tailed, alpha = 0.05) of >85 %. Therefore, size of the included study groups was considered as sufficient for this pilot study after weighing statistical considerations along with logistical and resource constraints.
Results
Participants
The demographic variables including gender, age, years of working experiences are shown in Table 1.
69 % of the physicians in the intervention group were women (n = 26) and 31 % were men (n = 12). The comparison group include 70 % female physicians (n = 28) and 30 % male physicians (n = 12). The average age in the intervention group was 27 years (SD 2.1) with an average time of working experience as a physician of 1 year (SD 1.8). All the gynecologists were employed full-time. Comparing both groups (IG and CG) baseline data on socio-demographic differences indicate insignificant differences.
Dropout attrition
Of the 80 junior physicians enrolled, all completed the baseline measures. Two physicians of the IG were excluded for the follow-up analyses because they participated in less than 80 % of the training sessions.
As illustrated in Fig. 1, during follow-up 1, 37 of the participants in the IG (98 %) gave responses, and 33 (n = 87 %) gave responses for follow-up 2. Finally, 31 physicians of the IG (82 %) answered the last survey (follow-up 3). Participants who failed to complete the follow-up surveys did not differ in their baseline responses from those who complied with the study protocol.
Outcome analyses
Table 2 illustrates the main outcome parameters: occupational stress, emotional exhaustion, job satisfaction and changes in emotion regulation, resilience as a coping behavior in intervention and control group at baseline (T0) and follow-up (1), follow-up (2) and follow-up (3).
Significant group effects have been found: the intervention group showed improved scores on occupational stress in contrast to the control group. Middle to large between-group effect sizes were observed at t1 (Cohen’s d = 0.52; 95 % CI 0.38–0.74; P < 0.001), t2 (Cohen’s d = 0.46; 95 % CI 0.27–0.61; P < 0.01) and t3 (d = 0.38; 95 % CI 0.21–0.58). The control group showed no significant within-group effect sizes (P > 0.05) from pre-test to all follow-ups.
The scale for emotional exhaustion also showed improvements, with medium effect sizes (t1: d = 0.59; 95 % CI 0.41–0.80).
At the second follow-up, the effect sizes ranges between small and moderate sizes (d = 0.23 for job satisfaction, d = 0.41 for resilience and d = 0.49 for emotion regulation skills). Moderate or small effect sizes were found at the third follow-up for emotional exhaustion (d = 0.43), emotion regulation skills (d = 0.41) and resilience (d = 0.39). Job satisfaction showed a small, but significant improvement (P < 0.05).
No significant group differences have been found comparing gynecologists and obstetricians (P > 0.05).
Correlations between changes in coping behavior (resilience and emotion regulation skills) and changes in other outcome measurements were also analyzed.
Improvements in emotion regulation skills and resilience were moderately correlated with decreases in total stress perceptions (1. emotion regulation r = −0.35, P < 0.01; resilience r = −0.39, P < 0.01). They were also moderately correlated with decreases in the emotional exhaustion subscale (emotion regulation r = −0.32, P < 0.01; resilience r = −37; P < 0.01).
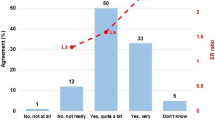
Evaluation of Kirkpatrick’s training criteria and satisfaction with the intervention
The evaluation results show an overall training satisfaction score of M = 4.58. Satisfaction with the training design was scored with M = 4.34. In addition, the atmosphere during the intervention was also rated with high scores (M = 4.21). All in all, gynecologists would recommend this skills training program M = 4.58. All scores of the skill training evaluation are illustrated in Table 3.
In addition, we proved the four levels of Kirkpatrick’s training criteria and demonstrated that they were fulfilled. For the learning criterion gynecologists identified that they learned to understand the values and principles of the diverse coping strategies, conflict management, etc. and how to exercise and repeat in every day work. The gynecologists indicated that the usage of the practical everyday instructions of the training was relevant and appropriate in their clinical work. The participating gynecologists reported that they feel more at comfort, experience the feeling of more control and autonomy during work.
89 % of the gynecologists gave best grades for satisfaction with the training (“being satisfied in an overall, general sense; very satisfied or satisfied. 85 % of the gynecologists stated that they got the kind of training they anticipated before starting the training. 87 % reported that the training met their individual needs. In addition, 80 % described that the skill training was supportive in dealing more effectively with clinical work problems and daily working demands.
Discussion
The main focus of this pilot study was to evaluate the outcomes of a coping skills training for junior physicians working in Gynecology and Obstetrics Medicine. Evaluation results can be interpreted in a way that the training was effective in improving residents stress and exhaustion levels as well as their individual coping skills (such as emotion regulation). Our findings suggest that a psychosocial skills training may support young health professionals in Gynecology and Obstetrics.
To our knowledge, this is the first scientific evaluation on mental health prevention with focus on strengthen gynecologists’ coping skills. Other evaluation studies investigated on mental health promotion programs implemented in other working settings [36–39].
In comparison to other coping skill trainings in the medical setting mixed between-group effects for reduced stress perceptions after the intervention have been demonstrated, ranging from non-significant to moderate effect sizes [40–42]. Studies on mindfulness training for physicians, in particular, also showed significant improvements in stress perceptions [22, 43].
Long-term improvement of work-related strain after taking part in such training may be achieved by active and ongoing practice of learned and experienced psychosocial skills, an improved regulation of conflicts and emotions, as well as better communication skills [44]. In addition, psychosocial competencies may support gynecologists’ resilience via self-awareness development. These insights may lead to long lasting behavior changes that may also have positive effects on quality of patient care in health services [45].
Moreover, significant medium to large between-group effects were also found for emotional exhaustion, anxiety and emotion regulation competencies. Previous studies that focused on these parameters showed comparable results: Goodman et al. as well as Pflugeisen et al. developed a mindfulness training intervention for health professionals and reported significant improvements in emotional exhaustion and perceived stress at work [46, 47].
A similar integrative self-care program for healthcare professionals was implemented and evaluated by Huang et al. [48] also presenting significant effects on perceived job stress, emotional exhaustion and prolonged fatigue.
The current study finding showed only small improvements on gynecologists’ job satisfaction after training. This result was expected, former studies verified this result also demonstrating small effects of stress management interventions on perceptions of employees’ job satisfaction [49–51]. It is reasonable to assume that the training content did not directly focus on improving gynecologists’ job satisfaction. Additional interventions designed to more specifically address other elements of job satisfaction may be necessary to affect those domains, including organizational interventions.
All participants reported a positive evaluation with high scores for training design, training outcomes and overall satisfaction with the psychosocial skill training.
The positive evaluation was also confirmed by proving the levels of Kirkpatrick’s training criteria [52]. The participating physicians reported an improvement in the awareness for relations between work-related demands, their work ability and mental health. A repetitive use of the learned skills in coping with stressful work situations and daily challenges and an improvement in their professional and social competencies were declared.
Our study results are also comparable to findings of studies evaluating Balint interventions [53, 54]. Both forms of intervention are useful and necessary; Balint groups focus mostly on case presentation followed by general discussion with the focus and emphasis on the emotional content of the doctor–patient relationships [55, 56]. The psychosocial training, we presented here, focused mostly on first work experiences, individual coping skill training and conflict management training aiming to strengthen coping behavior (i.e., resilience and self-efficacy). In our opinion, both interventions complement each other in a very good way; therefore, we would combine them. At first, we would implement our training just after medical graduation while starting work in the clinic. After the first year, we would integrate Balint groups with a stronger focus on supervision and concrete medical cases.
In general, we think, increasing gynecologists’ skills and confidence in dealing with psychosocial aspects of medicine is an implied goal and outcome of long-term education in Gynecology Medicine. Our preliminary research into the effectiveness of a psychosocial training supports the conclusion that training enhances the levels of residents’ behavioral skills.
Strength and limitations
Mental health support programs are rare in general: so this study is the first to implement and evaluate a mental health promotion program for gynecologists. The main strength of this study is the controlled study design. The number of follow-ups can be considered as very satisfying for worksite health promotion research.
Limitation of this pilot study is its small sample size. So, the external validity of the study findings is restricted. Statistical significance should be interpreted cautiously due to the exploratory nature of the pilot study. The time period of 6 months is quite short for the follow-up measurements, so long-term effects of the pilot intervention cannot be concluded.
Generalizability is limited as gynecologists were self-selected. They may have enrolled because of special curiosity or awareness and may be those who find psychosocial skill training more interesting than do their colleagues. As a further limitation: only self-report measures were included due to feasibility reasons. A mixture of self-report questionnaires and physiological (objective) performance evaluation measures could add further important indications and suggestions.
Practical implications and future directions
Further research in the future should repeat this pilot intervention in larger study trails and for longer time periods as such trainings may have the potential to improve the work ability, performance and mental health of employees with a lasting effect.
Implementation of this work-related psychosocial training during work-time was not possible due to bureaucratic and organizational requirements and the perceived need for financial investments. Therefore, this training was performed off duty. However, participation rate was high, so we conclude motivation and acceptance of the training were also high. Nevertheless, it is recommended, if possible, to integrate such work-related training during work-time. To our opinion, often overlooked is the potential of such an intervention to increase employees’ motivation and commitment. This, in turn, is likely to have a direct impact on performance and productivity. In addition, the implementation of such training can demonstrate that the employer cares about the well-being and work ability of their employees, and leads to an enhanced organizational culture and an improvement in staff retention [57, 58]. We hope integration of such a supportive intervention during work-time is an option in the future.
Given the shared responsibility of health professionals and health care organizations to support and promote clinicians performance, mental health and well-being, a good prognosis is likely to involve institutionally individual strategies and efforts in combination with institutional approaches (i.e., restructuring of the institutional environment) [50, 59].
We think such wide-ranging and comprehensive approach has the potential to change the actual situation of work-related distress among physicians into a situation of successful working environments [60].
As illustrated, such an intervention is flexible and adaptable; therefore, it could be integrated easily in various hospital departments and/or medical specialties.
However, further studies are needed to verify this pilot study and to prove the usefulness of mental health support interventions for clinicians.
Conclusion
This study provides first indications that mental health promotion skills training for junior gynecologists might be a promising approach to improve and support junior physicians.
Our results suggest this training is a relatively low cost, time-efficient way to improve physicians’ well-being and coping skills. The intervention is practicable and the results specify that this intervention could be helpful and beneficial in the health care sector, not only for physicians in Gynecology and Obstetrics Medicine.
This pilot study is not an overall solution for physician work-related stress but symbolizes an important value to promote gynecologists performance and well-being. Additional research is needed to confirm these and previous findings. Understanding the complex interactions among physicians’ health, performance in patient care will help health care organizations develop programs that support physicians and improve job performance, satisfaction, and patient care within this demanding profession.
Abbreviations
- ANCOVA:
-
Analysis of covariance
- b :
-
Beta weight
- BRCS:
-
Brief Resilient Coping Scale
- CI:
-
Confidence interval
- COPSOQ:
-
Copenhagen Psychosocial Questionnaire
- d :
-
Effect size
- ERSQ:
-
Emotion Regulation Skills Questionnaire
- N:
-
Numbers
- M:
-
Mean
- MBI:
-
Maslach Burnout Inventory
- MD:
-
Median
- PSQ:
-
Perceived Stress Questionnaire
- SD:
-
Standard deviation
References
Emmons SL, Nichols M, Schulkin J, James KE, Cain JM (2006) The influence of physician gender on practice satisfaction among obstetrician gynecologists. Am J Obstet Gynecol 194:1728–1738
Bauer J, Groneberg DA, Brueggmann D (2016) Gender-based workplace assessment in gynecology and obstetrics in Germany: results from the iCEPT Study. Arch Gynecol Obstet 294:317–326
Esteves SC, Hamada A, Kondray V, Pitchika A, Agarwal A (2012) What every gynecologist should know about male infertility: an update. Arch Gynecol Obstet 286:217–229
Graham J, Ramirez A (2002) Improving the working lives of cancer clinicians. Eur J Cancer Care 11:188–192
Rasmussen V, Turnell A, Butow P, Juraskova I, Kirsten L, Wiener L, Patenaude A, Hoekstra-Weebers J, Grassi L (2016) Burnout among psychosocial oncologists: an application and extension of the effort-reward imbalance model. Psychooncology 25:194–202
Keeton K, Fenner DE, Johnson TRB, Hayward RA (2007) Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol 109:949–955
Becker JL, Milad MP, Klock SC (2006) Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol 195:1444–1449
Shanafelt TD, Boone S, Tan L (2012) Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 172:1377–1385
Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM (1996) Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 347:724–728
Brooks SK, Chalder T, Gerada C (2011) Doctors vulnerable to psychological distress and addictions: treatment from the Practitioner Health Programme. J Ment Health 20:157–164
Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, Edwards S, Wiedermann BL, Landrigan CP (2008) Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ Clin Res Ed 336:488–491
West CP, Shanafelt TD (2007) Physician well-being and professionalism. Minn Med 90:44–46
Ruitenburg MM, Frings-Dresen MHW, Sluiter JK (2012) The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: a cross-sectional study. BMC Health Serv Res 12:292
Shanafelt TD (2009) Enhancing meaning in work: a prescription for preventing physician burnout and promoting patient-centered care. JAMA 302:1338–1340
Williams ES, Manwell LB, Konrad TR, Linzer M (2007) The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manag Rev 32:203–212
Hancke K, Igl W, Toth B (2014) Work—life balance of German gynecologists: a web-based survey on satisfaction with work and private life. Arch Gynecol Obstet 289:123–129
Carver CS, Scheier MF, Weintraub JK (1989) Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 56:267–283
Macedo T, Wilheim L, Gonçalves R, Coutinho ES, Vilete L, Figueira I, Ventura P (2014) Building resilience for future adversity: a systematic review of interventions in non-clinical samples of adults. BMC Psychiatry 14:227–241
Ramaswamy R, Williams A, Clark EM, Kelley AS (2014) Communication skills curriculum for foreign medical graduates in an internal medicine residency program. J Am Geriatr Soc 62:2153–2158
Puskar KR, Sereika S, Tusaie-Mumford K (2003) Effect of the teaching kids to cope (TKC) program on outcomes of depression and coping among rural adolescents. J Child Adolesc Psychiatr Nurs 16:71–80
Tan L, Wang MJ, Modini M, Joyce S, Mykletun A, Christensen H, Harvey SB (2014) Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med 12:74
Krasner MS, Epstein RM, Beckman H (2009) Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physician. JAMA 302:1284–1293
Czabała C, Charzyńska K, Mroziak B (2011) Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int 26(Suppl 1):i70–i84. doi:10.1093/heapro/dar1050
Lagerveld SE, Blonk RW, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB (2012) Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J Occup Health Psychol 17:220–234
Lazarus R, Folkman S (1984) Stress, appraisal, and coping. Springer Publishing Co, New York
Malouff JM, Thorsteinsson EB, Schutte NS (2007) The efficacy of problem solving therapy in reducing mental and physical health problems: a meta-analysis. Clin Psychol Rev 27:46–57
D’Zurilla T, Nezu A, Dobson KS (2010) Problem-solving therapy. Handbook of cognitive-behavioral therapies. Guilford Press, New York
Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C (1993) Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. J Psychsom Res 37:19–32
Kristensen T, Hannerz H, Høgh A, Borg V (2005) The Copenhagen Psychosocial Questionnaire (COPSOQ). A tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health 31:438–449
Nuebling M, Hasselhorn HM (2010) The Copenhagen Psychosocial Questionnaire in Germany: from the validation of the instrument to the formation of a job-specific database of psychosocial factors at work. Scand J Public Health 38:120–124
Schaufeli W, Leiter M, Maslach C, Jackson S (1996) Maslach Burnout Inventory—General Survey (MBI-GS). In: Maslach C, Jackson SE, Leiter MP (eds) Maslach Burnout Inventory Manual. Consulting Psychologists Press, Palo Alto
Berking M, Znoj H (2008) Development and validation of a self-report instrument for the assessment of emotion-specific regulation skills (ERSQ-27). Z Psychiatrie Psychol Psychother 56:141–153
Sinclair VG, Wallston KA (2004) The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 11:94–101
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. Stat Soc Ser 57
Cohen J, Hillsdale NJ (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, New York
Buchberger B, Heymann R, Huppertz H, Friepörtner K, Pomorin N, Wasem J (2011) The effectiveness of interventions in workplace health promotion as to maintain the working capacity of health care personal. GMS Health Technol Assess 1
Zimber A, Gregersen S, Kuhnert S, Nienhaus A (2010) Workplace health promotion through human resources development part I: development and evaluation of qualification programme for prevention of psychic stresses. Gesundheitswesen 72:209–215
Burton NW, Pakenham KI, Brown WJ (2008) Feasibility and effectiveness of psychosocial resilience training: a pilot study of the READY program. Psychol Health Med 15:266–277
Leppin AL, Gionfriddo MR, Sood A, Montori VM, Erwin PJ, Zeballos-Palacios C, Bora PR, Dulohery MM, Brito JP, Boehmer KR, Tilburt JC (2014) The efficacy of resilience training programs: a systematic review protocol. Syst Rev. doi:10.1186/2046-4053-3-20
Goldhagen BE, Kingsolver K, Stinnett SS, Rosdahl JA (2015) Stress and burnout in residents: impact of mindfulness-based resilience training. Adv Med Educ Pract 25:525–532
McCue JD, Sachs CL (1991) A stress management workshop improves residents’ coping skills. Arch Intern Med 151:2273–2277
Ospina-Kammerer V, Figley CR (2003) An evaluation of the respiratory one method (ROM) in reducing emotional exhaustion among family physician residents. Int J Emerg Ment Health 5:29–32
Shapiro SL, Astin JA, Bishop SR (2005) Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag 12:164–176
Holton MK, Barry AE, Chaney JD (2015) Employee stress management: An examination of adaptive and maladaptive coping strategies on employee health. Work
Schneider S, Kingsolver K, Rosdahl J (2014) Physician coaching to enhance well-being: a qualitative analysis of a pilot intervention. Explore 10:372–379
Goodman MJ, Schorling JB (2012) A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med 43:119–128
Pflugeisen BM, Drummond D, Ebersole D, Mundell K, Chen D (2016) Brief video-module administered mindfulness program for physicians: a pilot study. Explore 12:50–54
Huang SL, Li RH, Huang FY, Tang FC (2015) The potential for mindfulness-based intervention in workplace mental health promotion: results of a randomized controlled trial. PLoS One 10
West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, Romanski SA, Hellyer JMH, Sloan JA, Shanafelt TF (2014) Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med 174:527–533
Sood A, Prasad K, Schroeder D, Varkey P (2011) Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. J Gen Intern Med 26:858–861
Ayres J, Malouff JM (2007) Problem-solving training to help workers increase positive affect, job satisfaction, and life satisfaction. Eur J Work Organ Psychol 16:279–294
Kirkpatrick DL, Kirkpatrick DJ (2006) Evaluating training programs: the four levels. Berrett-Koehler Publishers, Oakland
McKensey A, Sullivan L (2016) Balint groups—helping trainee psychiatrists make even better use of themselves. Australas Psychiatry 24:84–87
Parker SD, Leggett A (2014) Reflecting on our practice: an evaluation of Balint groups for medical students in psychiatry. Australas Psychiatry 22:190–194
Van Roy K, Vanheule S, Inslegers R (2015) Research on Balint groups: a literature review. Patient Educ Couns 98:685–694
Lee E, Kealy D (2014) Revisiting Balint’s innovation: enhancing capacity in collaborative mental health care. J Interprof Care 28:466–470
Aust B, Ducki A (2004) Comprehensive Health promotion interventions at the workplace: experiences with health circles in Germany. J Occup Health Psychol 9:258–270
Köhler T, Janssen C, Platz SC, Reese JP, Lay J, Steinhausen S, Gloede T, Kowalski C, Schulz-Nieswandt F, Pfaff H (2010) Communication, social capital and workplace health management as determinants of the innovative climate in German banks. Int J Public Health 55:561–570
Warnecke E, Quinn S, Ogden K, Towle N, Nelson MR (2011) A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Med Educ 45:381–388
Shanafelt TD, Balch CM, Bechamps GJ (2009) Burnout and career satisfaction among American surgeons. Ann Surg 250:463–471
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare, they have no conflict of interest.
Ethical considerations
Ethical approval was granted by the Institutional Review Board of the Free University Berlin. The study is in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964.
Informed consent
Informed consent was obtained from all participating physicians included in this study.
Rights and permissions
About this article
Cite this article
Mache, S., Baresi, L., Bernburg, M. et al. Being prepared to work in Gynecology Medicine: evaluation of an intervention to promote junior gynecologists professionalism, mental health and job satisfaction. Arch Gynecol Obstet 295, 153–162 (2017). https://doi.org/10.1007/s00404-016-4223-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4223-6