Abstract
Purpose
The aim of this study is to identify the rate of incisional hernias and associated risk factors following a vertical midline laparotomy on a gynecologic oncology service.
Methods
This is a retrospective cohort study of patients that underwent a laparotomy through a vertical midline abdominal incision between September 1998 and November 2012. Hernias and various factors were identified including demographics, disease comorbidities, intraoperative variables, and suture technique. Assessment of association with hernia formation was performed using Cox regression and log-rank test.
Results
Two hundred and fifty-two patients with follow-up of at least 30 days were identified. Mean age was 59 years (range 21–88 years) and mean BMI was 35.9 kg/m2 (range 17.2–84.4 kg/m2). Sixteen (6.3 %) developed incisional hernias with a median follow-up of 1.7 years (range 1 month to 13 years). The estimate of the 5-year probability of being hernia-free is 86 % (95 % CI 76.5–91.9). Average age of patients who developed a hernia was 66.2 years while average age of those without hernia was 58 years (p < 0.05). There was a significant association of hypertension with incisional hernia occurrence (p = 0.0035, log-rank test). Cancer was present in 100 % of patients that developed hernias and 73 % (172/236) of those that were hernia-free (p = 0.0041, log-rank test). By univariate analysis the risk of developing an incisional hernia was higher, if the abdominal fascia was closed with loop sutures (HR 4.6, 95 % CI 1.49–13.94; p = 0.008). By multivariable analysis incisions closed with loop suture had more than a fivefold increased risk of developing a hernia (HR 5.2, 95 % CI 1.65–16.39; p = 0.005). Presence of both hypertension and utilization of loop sutures had the highest risk of incisional hernia development (HR 7.1, 95 % CI 2.28–22.4; p = 0.001).
Conclusion
Wound complications including incisional hernias contribute to morbidity in gynecologic oncology patients. Older age, hypertension, utilization of loop sutures, and cancer were found to be associated with hernia formation after laparotomy through a vertical midline abdominal incision. The use of loop sutures to close the abdominal fascia should be investigated further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incisional hernias contribute significantly to patient morbidity and increased health care costs. Hernias can cause pain and have the potential to incarcerate or strangulate. The reported prevalence of incisional hernias 1 year after a midline laparotomy ranges from 5 to 15 % [1]. Following hernia repair, recurrences can occur in up to one-half of the cases [2, 3].
Incisional hernias can be caused by excessive tension on the suture line, impaired wound healing, or poor suturing technique. Various factors have been shown to contribute to the risk of incisional hernia formation [3]. Excessive suture line tension can occur in cases with large body mass index (BMI), abdominal distension, or with pulmonary comorbidities [5, 7]. Factors theorized to impair wound healing include diabetes, steroid therapy, chronic kidney disease, malnutrition, and the presence of malignancy [4, 8]. Wound closure techniques have been studied to identify the most effective method. Studies have suggested that mass closure of a midline abdominal incision in a simple running fashion with a suture to length ratio of 4:1 using a non-absorbable or slowly absorbable suture lowers the incidence of incisional hernias and fascial dehiscence [4, 9, 10].
Vertical midline abdominal incisions offer ideal exposure for certain gynecologic oncology procedures including staging and surgical cytoreduction. Following surgery many gynecologic oncology patients receive chemotherapy and/or radiation therapy, both of which have previously been identified as independent factors that impair wound healing and increase risk of hernia formation [11]. The baseline risk for post-operative hernia formation seems to be higher in oncology patients than in those undergoing surgery for benign indications [8, 11–13]. However, there is limited research on risk factors associated with hernia development in gynecologic cancer patients. Optimization of modifiable factors associated with hernia development has the potential to reduce post-operative morbidity resulting in improved quality of life. The aim of this study is to estimate the long-term risk of incisional hernia development, and identify risk factors associated with incisional hernia development in patients undergoing a midline laparotomy on a gynecologic oncology service.
Materials and methods
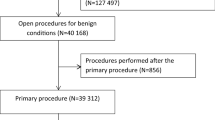
A retrospective chart review of patients that underwent a vertical midline abdominal incision on one surgeon’s gynecologic oncology service between September 1998 and November 2012 was performed. The information from the medical records was initially collected by one of the investigators (S. W.) and entered into an electronic spreadsheet. The data were verified for accuracy by two other investigators (J. G., E. H.). Patients with available medical records and follow-up of at least 30 days were included. Hernias were identified by physical examination (i.e., palpable defect in the fascia along the surgical scar). A standard post-surgical evaluation form that specifically asked for the presence or absence of hernia, and its location if present, was used. The estimate of the cumulative probability of developing an incisional hernia was calculated using the Kaplan–Meier method. Possible risk factors were identified including age, race, BMI, smoking history, presence of cancer, histology and its stage, disease comorbidities such as hypertension, diabetes, and chronic obstructive pulmonary disease (COPD), radiation or chemotherapy treatment, albumin levels pre-operatively, intraoperative factors including extent of incision (above or below the umbilicus), blood transfusion, estimated blood loss (EBL), and abdominal wall closure technique. Comparison was made between using #1-0 vs. #1 suture, continuous vs. interrupted closure, and use of loop suture vs. non-loop suture. Descriptive analysis between groups was made using two-sample student t-test for continuous variables and Chi-square test for categorical variables. The association between possible risk factors and incisional hernia development was analyzed using Cox regression and log-rank test.
Type of surgical procedures included simple hysterectomy, trachelectomy, radical hysterectomy, radical vaginectomy, radical trachelectomy, myomectomy, salpingo-oophorectomy, ovarian cystectomy, resection of ovarian malignancy and staging, intestinal resection, colostomy, pelvic and/or para-aortic lymphadenectomy, retroperitoneal exploration, lysis of adhesions, and urinary diversion.
The standard surgical approach consisted of performing a vertical midline incision on the skin using a scalpel. Prophylactic antibiotics were given before incising the skin. The subcutaneous fat was separated with electrocautery. The rectus fascia was incised with a scalpel. The peritoneal cavity was entered sharply. The peritoneal and fascial incisions were extended using scissors or electrocautery. The duration of the majority of the procedures was between 120 and 240 min. The wound was periodically irrigated with normal saline when the procedure lasted for more than 4 h. At the completion of the procedure the fascia was closed with interrupted stitches or a continuous running stitch in two lengths. The peritoneum was not closed. The subcutaneous fat was not approximated and a supra-fascial drain was not used. The skin was approximated with stainless steel surgical staples. A pressure dressing was applied and removed on the first post-operative day. No prophylactic heparin was used before surgery, but all patients had pneumatic sequential compression stockings on their legs during the procedure. Prophylactic heparin was started the morning of the first post-operative day, as was ambulation.
This study underwent expedited review by Temple University Institutional Review Board (protocol #13393). It was determined that the study qualified for exemption and that informed consent from the study subjects was not necessary.
Results
A total of 781 patients underwent a laparotomy through a vertical midline abdominal incision between September 1998 and November 2012. Two hundred and fifty-two (32 %) patients had medical records available for review with follow-up of at least 30 days. Follow-up range was 30 days–13 years with a median follow-up of 1.7 years. Average age of patients was 59 years (range 21–88 years). One hundred and fifty (59 %) patients were Caucasians, 55 (22 %) African-American, 22 (9 %) Hispanics, 10 (4 %) Asians and 15 (6 %) other or not recorded. Among the 16 patients who developed a hernia 9 (56 %) were Caucasian and 5 (31 %) were African-American. The average weight was 186.7 lbs (range 88.5–367 lbs). BMI ranged from 17.2 to 84.4 kg/m2 with an average of 35.9 kg/m2. A final diagnosis of cancer was rendered in 188 (75 %) patients. Twenty-five (13 %) patients had cervical cancer, 90 (48 %) endometrial cancer, 53 (28 %) ovarian cancer, 12 (6 %) uterine carcinosarcoma, 3 (1.6 %) fallopian tube cancer, and 5 (2.6 %) a non-gynecologic cancer. Of patients with a gynecologic cancer 109 (59.5 %) had stage I, 13 (7.1 %) stage II, 43 (23.5 %) stage III, 10 (5.5 %) stage IV, and 8 (4.4 %) were unstaged or the stage was not available (Table 1).
Among the 252 patients, 16 (6.3 %) hernias were identified from 135 days to 5 years after surgery. Median time to identification of hernias was 3.26 years. The estimate of the 5-year probability of being hernia-free is 86 % (95 % CI 76.5–91.9) (Fig. 1). None of the patients had significant symptoms related to the hernia at the time the diagnosis was clinically made. Some patients noticed a bulge and a few patients complained of intermittent abdominal discomfort. None needed immediate surgical intervention for the hernia. Average age of those with hernias was 66.2 years while the average age of those without hernia was 58 years (p < 0.05) (Table 2). Body mass index was slightly higher in those that developed hernia with an average of 38.04 kg/m2 (range 23.93–53.96 kg/m2) and 35.76 kg/m2 (range 17.2–84.4 kg/m2) in those without hernias. However, the difference was not statistically significant.
Overall, 26 % (65/252) of the patients had diabetes and 58 % (145/252) had hypertension. Information on the severity of these conditions was not available. Hernias were observed to occur more frequently in patients with comorbidities. Of the 16 patients with hernias, 38 % (6/16) were diabetic and 94 % (15/16) were hypertensive. There was a significant association of hypertension with incisional hernias (p = 0.0035). Cancer was present in 100 % of patients that developed hernias and 73 % (172/236) of those that were hernia-free (p = 0.0041). Of the 16 patients with hernias, 12 had endometrial cancer and their average BMI was 36 kg/m2. One patient with hernia had ovarian cancer and one had fallopian tube cancer. Neither of these patients had ascites. The remaining two hernia patients had cervical cancer. Radiation and chemotherapy treatment independently were not associated with the occurrence of an incisional hernia. However, the details of these treatments were not available.
By univariate analysis the risk of developing an incisional hernia was higher if the abdominal fascia was closed with loop sutures (HR 4.6, 95 % CI 1.49–13.94, p = 0.008). By multivariable analysis incisions closed with loop suture had more than a fivefold increased risk of hernia occurrence than those closed with non-loop suture (HR 5.2, 95 % CI 1.65–16.39; p = 0.005). Patients whose abdomen was closed with a loop suture were similar to those whose closure was done with a single strand suture except that more women in the former group had diabetes mellitus (Table 3). The risk of hernia formation was highest among patients who had history of hypertension and whose abdominal fascia was closed with loop suture (HR 7.1, 95 % CI 2.28–22.4; p = 0.001). The extent of the abdominal incision (above or below the umbilicus), type of suture used (polyglactin vs. polydioxanone), suture size (#1 vs. #0) or the type of stitch (continuous vs. interrupted) were not associated with the occurrence of incisional hernias.
Smoking history was not statistically significantly associated with hernia development. Neither was patients' race or cancer stage. Preoperative albumin level was not statistically significantly associated with hernias. The probability of developing an incisional hernia was not associated with EBL, or need for intraoperative blood transfusion.
Discussion
Using the Kaplan–Meier method we estimated that the probability of developing an incisional hernia 5 years after a midline laparotomy is 14 % (95 % CI 7.9–22.5). This is within the range reported by others with shorter patient follow-up [1]. There are a few reports on the development of incisional hernias following surgery for gynecologic malignancies. Gynecologic oncology patients represent an unique population with regards to incisional hernia risk. Aside from the presence of malignancy and possibly impaired immune system, these patients frequently undergo long vertical incisions to obtain adequate visualization required for optimization of staging and tumor debulking. Franchi et al. [12] reported a 16.9 % incisional hernia rate among patients who had a laparotomy for uterine or cervical cancer. Long et al. [13] reported on 167 women who underwent primary laparotomy for ovarian, fallopian tube or primary peritoneal carcinoma and who were followed for 2 years. The 2-year hernia rate was 23.4 % (39/167). Spencer et al. [8] reported a 9.8 % 1-year hernia rate among 265 women who underwent primary laparotomy for ovarian cancer. Of the 189 patients who were followed for 2 years, an additional 7.9 % developed a hernia. A meta-analysis of 14,618 patients identified a mean incisional hernia rate of 12.8 % (95 % CI 11.4–14.2) at a weighted mean follow-up time of 2 years [14]. Others using the Kaplan–Meier method have estimated that the 10-year probability of incisional hernia formation is 18.7 % [6]. More than one-half of incisional hernias are recognized 12 months after surgery and 75 % are diagnosed 2 years after surgery [6]. In our patients the median time for the identification of a hernia was 3.26 years. Our estimate of the probability of incisional hernia formation at 5 years is within the range reported by others. It can be argued that if a hernia develops many years after surgery it may be due to other patient intrinsic factors and not due to the previous surgery. However, the impact surgical wound healing may have on delayed hernia formation cannot be discounted.
By univariate analysis closure with a loop suture was associated with a statistically significantly higher rate of incisional hernias than closure with single strand suture. By multivariable analysis our patients whose incisions were closed with loop suture had a fivefold increased risk of hernia formation when compared to those closed with single strand suture. A theoretical explanation of this finding may involve an exaggerated inflammatory response due to the amount of suture material left in the wound and/or the placement and spacing of the stitches. Milbourn et al. [15] performed a pseudorandomized controlled trial that compared the outcomes of patients undergoing their first laparotomy through a midline incision. The 737 patients had their abdominal wall closed with a “small or long stitch” (small or large bites of tissue). Patients in the “long stitch” group had the stitches placed more than 10 mm from the fascial edge using #1-0 polydioxanone (PDS) suture. The comparison group (short stitch) had the stitches placed 5–8 mm from the fascial edge using #2-0 PDS suture. At a 12-month post-surgery assessment incisional hernias were identified more frequently in patients assigned to the “long stitch” group (18 vs. 5.6 %, p < 0.001). The authors suggest that with smaller amounts of tissue in the closure there is less trauma and less ischemia resulting in decreased number of hernias. This finding was confirmed by a more recent study that randomly assigned 560 patients scheduled to undergo an elective midline vertical laparotomy to closure of the fascia with small tissue bites (5 mm every 5 mm) or large bites (10 mm every 10 mm) [16].They used #2-0 PDS on a 31 mm needle for the short bites and #1 PDS for the large bites. They identified incisional hernias by physical examination, diagnostic imaging or both. At 1 year follow-up 21 % of patients in the large bites group developed hernias compared to 13 % in the small bites group. The proportion of fascial dehiscence was 0.7 % in the large bites group and 1.4 % in the small bites group (p = 0.44). The loop sutures utilize double the amount of suture material than the single strand suture. The #1 and the #1-0 PDS loop sutures we use are mounted on a 65 mm half circle needle (TP-1, Ethicon, Inc.), while the #1-0 PDS or polyglactin single strand sutures are mounted on a 36 mm half circle needle (CT-1, Ethicon, Inc.). Placement of sutures further away from the wound edge with larger bites, which is the tendency with loop sutures on larger sized needles, increases compressive forces on the tissue contained between the stitches. This could result in impairment of the wound microvasculature resulting in suboptimal wound healing. Closure with a loop suture may in theory reduce the rate of early post-operative fascial dehiscence due to suture breakage, which outweighs the risk of long-term incisional hernia development. However, the only patient who had a fascial dehiscence in Milbourn et al.’s [15] study was in the group closed with large bites and thicker suture. In the study by Deerenberg et al. [16], even though the rate of fascial dehiscence was 0.7 % in the small bites group using #2-0 PDS suture compared to 1.4 % in the large bite group using #1 PDS suture, the difference was not statistically significant. None of the patients in our study suffered a fascial dehiscence. Most fascial disruptions are caused by fascial tears and not due to a broken suture [5, 17].
We also found that hypertension is associated with a statistically significant higher incisional hernia rate. Arterial hypertension may affect the microvasculature and negatively impact wound healing. By multivariable analysis, patients with hypertension whose abdomen was closed with a loop suture had the highest risk of developing an incisional hernia (HR 7.1, 95 % CI 2.28–22.4; p = 0.001). This suggests that the compromise of the microvascular environment due to hypertension combined with the trauma and relative ischemia caused by large stitch bites results in impaired wound healing and subsequent hernia formation.
Another factor associated with a higher incisional hernia rate in our patients is cancer. This may be due to the higher BMI typical of patients with endometrial cancer who comprised the majority of our patients who developed a hernia. However, in our study BMI was not independently associated with incisional hernias. The average BMI of our patents is 35.9 kg/m2. Therefore, we may not have identified BMI as a risk factor because the majority of our patients are obese.
The association of patient age and hernia risk almost reached statistical significance (p = 0.056). The patients who developed hernias were on average 8 years older than those who did not. Bosanquet et al. [14] reported that increasing age was associated with a higher rate of incisional hernias. This association was also found by Spencer et al. [8] who pointed out that older patients may have hematologic issues and vascular deficiencies that could predispose to deficits of fascial strength.
This study suffers from many of the limitations of retrospective studies to include selection bias. As a teaching institution we aim at exposing our trainees to various surgical techniques and allow the senior residents to make independent decisions. The decision as to what type of suture to use for abdominal closure, as well as the technique (continuous vs. interrupted) was often left to the discretion of the chief resident assisting with the surgery. This obviously introduces selection bias since the choice of closure technique can be influenced by perceived patient risk factors. However, as shown in Table 3 patients whose abdomen was closed with a loop suture were similar to those whose abdomen was closed with a single strand suture except that a higher proportion of them had history of diabetes mellitus (38 vs. 22 %). Due to the referral nature of our practice many of our patients returned to the referring hospital for post-surgical follow-up. Thereafter, those from our own clinic were seen for follow-up visit 4–6 weeks after surgery. Those with benign gynecologic pathology were examined annually, while those with cancer were seen more frequently (typically every 3 months for 2 years, then every 6 months for another 3 years and after that annually). Follow-up was available in only 32 % of 781 patients who underwent midline laparotomy on our service during the study period. Nonetheless, our estimate of incisional hernia rate at 5 years is similar to that reported by others. We included patients whose incisional hernias were identified by physical examination only. Others have included patients whose incisional hernias were identified by physical examination and/or imaging studies, which resulted in a slightly higher incisional hernia rate than ours. In the meta-analysis by Bosanquet et al. [14] the incisional hernia rate detected clinically was similar to that diagnosed clinically and radiologically (12.6 vs. 14.6 %, p = 0.22). We did not record for all our patients whether or not there were surgical site infections (SSI), which could predispose to hernia formation. However, of the 16 patients who developed a hernia none had a documented SSI (two had small seromas). All our patients receive prophylactic antibiotics before the skin incision. Studies that included previous laparotomies in their analysis show that the incisional hernia rate is higher among patients with previous laparotomies, but we did not abstract that information for this study.
Our study is exploratory in nature and suggests that wound closure with a loop suture on a large needle increases the risk of hernia formation. This needs to be confirmed with prospective studies.
References
O’Dwyer PJ, Courtney CA (2003) Factors involved in abdominal wall closure and subsequent incisional hernia. Surg J R Coll Surg Edinb Irel 1:17–22
Burger JW, Luikendijk RW, Hop WC, Halm JS, Verdaasdonk GG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
Hodgson NC, Malthaner RA, Østbye T (2000) The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg 231:436–442
Israellsson LA, Millbourn D (2013) Prevention of incisional hernias. How to close a midline incision. Surg Clin N Am 93:1027–1040
Poole GV (1985) Mechanical factors in abdominal wound closure: the prevention of fascial dehiscence. Surgery 97:631–640
Höer J, Lawong G, Klinge U, Schumpelick V (2002) Factors influencing the development of incisional hernia: a retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg 73:474–480
Goodenough CJ, Ko TC, Kao LS et al (2015) Development and validation of a risk stratification score for ventral incisional hernia after abdominal surgery: hernia expectation rates in intra-abdominal surgery (the hernia project). J Am Coll Surg 220:405–415
Spencer RJ, Hayes KD, Rose S et al (2015) Risk factors for early-occurring and late-occurring incisional hernias after primary laparotomy for ovarian cancer. Obstet Gynecol 125:407–413
Israelsson LA, Jonsson T (1996) Incisional hernia after midline laparotomy: a prospective study. Eur J Surg 162:125–129
Israelsson LA, Jinsson T (1993) Suture length to wound length ratio and healing of midline laparotomy incisions. Br J Surg 80:1284–1286
Rettenmaier MA, Abaid LN, Brown JV, Micha JP, Goldstein BH (2009) Chemotherapy and patient co-morbidity in ventral site hernia development. Gynecol Oncol 20:246–250
Franchi M, Ghezzi F, Buttarelli M, Tateo S, Balestreri D, Bolis P (2001) Incisional hernia in gynecologic oncology patients: 10-year study. Obstet Gynecol 97:696–700
Long KC, Levinson KL, Diaz JP, Gardner GJ, Chi DS, Barakat RR, Leitao MM Jr (2011) Ventral hernia following primary laparotomy for ovarian, fallopian tube, and primary peritoneal cancers. Gynecol Oncol 120:33–37
Milbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144:1056–1059
Bosanquet DC, Ansel J, Abdelrahman T et al (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14618 patients. PLoS One 10:e0138745
Deerenberg EB, Harlaar JJ, Steyerberg EW et al (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet 386:1254–1260
Osther PJ, Gjøde P, Mortensen BB, Mortenese PB, Bartholin J, Gottrup F (1995) Randomized comparison of polyglycolic acid and polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. Br J Surg 82:1080–1082
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
S. Wang was a visiting scholar at Temple University School of Medicine now back at The First Municipal Hospital of Shijazhuang City, Hebei, China.
Rights and permissions
About this article
Cite this article
Guitarte, C., Grant, J., Zhao, H. et al. Incisional hernia formation and associated risk factors on a gynecologic oncology service: an exploratory analysis. Arch Gynecol Obstet 294, 805–811 (2016). https://doi.org/10.1007/s00404-016-4100-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4100-3