Abstract
Objective
Physical activity during pregnancy is known to be beneficial, however there are controversies about the risk of preterm labor, and there is no published data to assess the association between cervical length and maternal physical activity during pregnancy. Therefore, the objective of the study was to describe the cervical length in the second and third trimesters, correlating with physical activity, anthropometric characteristics, and obstetric results.
Methods
Prospective cohort with 56 pregnant women, allocated in two groups according to the answers obtained by a validating questionnaire on physical activity. It was considered significant p < 0.05.
Results
The length of the uterine cervix was similar between active and sedentary women, from the 22nd to the 24th week of pregnancy (p = 0.58), and from the 32nd to the 34th week (p = 0.59). Gestational age at delivery was lower among active women than among sedentary ones, although without clinical repercussion, 38.2 ± 1.2 vs. 39.1 ± 1.2 weeks, respectively (p = 0.02). Among active women, 33 (89.1 %) had natural labor, while among sedentary ones, only 13 (68.4 %) (p = 0.05). The Apgar score was higher among children of active mothers (p = 0.04).
Conclusion
Despite being the data still to small to allow final conclusions, maternal physical activity, cervical length and its relation to spontaneous vaginal birth at term is a relevant topic for the information of women in early pregnancy. More investigations directly after specific activities such as riding, walking, and biking are needed to answer the questions we receive from our pregnant patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Assessing cervical length measured by transvaginal ultrasound is an effective method to predict the risk of preterm labor [1]. The relationship between shortened cervix during pregnancy and spontaneous preterm labor has been well characterized in non-selected groups and in women at high risk. The second trimester is ideal to measure cervical length, although the cut-off point is subject to debate [2].
Physical activity has obtained increased popularity among women who are searching for the possibility to keep their usual physical activities during the entire pregnancy. Guidelines from the United States, United Kingdom, and Denmark recommend a level of physical activity during pregnancy similar to the one of the non-pregnant women [3]. By demonstrating the benefits, many studies indicate decreasing backache and enhancing maternal and fetal welfare [4], even though it is not consensual among many authors if physical activity actually brings beneficial outcomes for fetal health.
There are many controversies in the literature regarding the possibility that physical activity during pregnancy increases preterm labor risk. Most studies do not associate the practice of physical exercises with preterm labor risk, low weight at birth, and neonatal complications [5, 6].
Since there are no published data evaluating the association of physical activity with cervical length during pregnancy, the objective of this study is to describe the cervical length in the second (22–24 weeks) and third trimester (32–34 weeks) of pregnancy, investigating its relation with the physical activity of the pregnant woman and its repercussion on obstetric and perinatal results.
Materials and methods
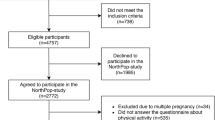
Prospective cohort study with 56 pregnant women at low risk, allocated in two groups: active (n = 37) and sedentary (n = 19) attended in a tertiary referral center in Southern Brazil from August 2009 to July 2011. Pregnant women who signed the free and informed consent form, after the approval of the study by the Research Ethics Committee of the Institution were included.
Pregnant women with risk factors known to preterm labor were excluded during the planning; strictly respecting the exclusion criteria and the contraindications to physical activities during pregnancy [7].
The International Physical Activity Questionnaire-Short Form (IPAQ-SF, version 8) validated in Brazil was applied [8]. The consensus achieved between the Center of Studies of the Physical Fitness Lab of São Caetano do Sul—SP (CELAFISCS) and the Center for Diseases Control (CDC) of Atlanta (2002) was followed, and the pregnant women were classified in active (very active, active, and irregularly active A) and sedentary (irregularly active B and sedentary).
An observer took cervical measures with the same transvaginal ultrasonography and following the protocol determined by the Fetal Medicine Foundation in both groups in the second and in the third trimester of pregnancy. The association of these measures with physical activity, the characteristics of the groups, and the obstetric outcomes obtained was verified.
To be included in this study, the gestational age (GA) of the women was observed, being established either by ultrasound performed up to the 12th week, or by the date of the last period (DLP) and confirmed by ultrasound up to the 20th week.
Data from the pregnant woman (weight, blood pressure), GA at delivery, mode of delivery, newborn (NB) weight, and Apgar score were evaluated.
The sample size estimated of sampling size to respond to the objectives of this study was determined by the following criteria: comparison of two averages with non-paired Student’s t test, 5 % alpha error, and 80 % statistical power. Considering that the average cervical length from 22 to 24 weeks is 30 mm and the standard deviation is 6 mm, the minimum value of 18 patients obtained for each group was enough to show the difference between groups, since cervical length differences considered clinically significant for this study was of at least 5.8 mm. This result was obtained using a 0.05 two-tailed alpha, and a test power of 80 % on GraphPad StatMate program version 1.01i. The sample size was later increased by 35 % due to possible segment losses predicted in a prospective longitudinal study.
The statistics was performed by descriptive analysis, expressing categorical variables in absolute and relative frequencies, as well as the analysis of numerical variables (sorted according to physical activity in active and sedentary women), through average, median and standard deviation or interquartile range. The analytical statistic was assessed by Chi-square and Fisher tests for categorical variables and by the Student t or Mann–Whitney tests for independent samples for numerical variables. Correlations among numerical variables were tested with the use of Pearson’s test. To evaluate the effect of physical activity on newborn weight adjusted to GA at delivery, a variance analysis was performed, considering the physical activity as a fixed effect, GA as co-variable, and weight at birth, independent variable. It was considered significant if p < 0.05.
Results
From the 56 patients included in the study, 54 (96.4 %) were white, one (1.8 %) brown and one (1.8 %) black. The average age was 29.6 ± 4.2 years. According to IPAQ-SF, 37 (66.1 %) were active and 19 (33.9 %), sedentary. Table 1 describes characteristics of the studied population. Its values were expressed by average ± standard deviation or absolute and relative frequency. Age, racial group proportion, and anthropometric variables were similar between active and sedentary women (p = 0.90). Weight gain was also similar between both groups, 12.9 ± 4.4 vs. 14.7 ± 4.1 kg (p = 0.150), respectively.
Systolic blood pressure (SBD), diastolic blood pressure (DBP), and variations between them from the first appointment to the 32nd week of pregnancy were similar in both groups (p = 0.63).
Among active women, 17 (45.9 %) were primigravidas, while 11 (57.9 %) sedentary women were first time mothers (p = 0.13).
There were similarities in GA in the inclusion of the study between active and sedentary women, established either by DLP (10.0 ± 3.8 vs. 10.5 ± 3.6, p = 0.678), or by ultrasound (10.1 ± 3.5 vs. 10.8 ± 3.9 weeks, p = 0.593).
Cervical length was similar between active and sedentary women on both assessments, from the 22nd to the 24th week, 39.9 ± 7.4 vs. 38.4 ± 8.0 mm, p = 0.583; from 32nd to 34th week, 29.5 ± 6.6 vs. 28.5 ± 5.8, p = 0.593. Variation in cervical length from the 22nd to the 24th and from the 32nd to the 34th week was similar between active and sedentary women, 10.4 ± 5.4 vs. 9.9 ± 5.2, p = 0.875, respectively (Table 1).
GA at delivery was lower among active women compared to sedentary women, although this finding was not clinical relevant, 38.2 ± 1.2 vs. 39.1 ± 1.2 weeks, respectively (p = 0.02).
Among active women, 33 (89.1 %) had natural labor while 13 (68.4 %) sedentary women had this birth mode of delivery with a tendency to the significance from the statistical point of view (p = 0.05).
Cervical dilation stage and expulsion period were similar between active and sedentary women, 7.1 ± 1.4 vs. 7.0 ± 1.3 h (p = 0.206) and 15.8 ± 5.8 vs. 15.2 ± 5.8 min (p = 0.762), respectively.
The Apgar score, disposed in medians and interquartile ranges, at the first minute after delivery was 8 (7–9) for children of active women and 7 (7–8) for children of sedentary ones (p = 0.046). At the fifth minute, the score of children of active women was 9 (9–10) and for children of sedentary women 8 (8–9) (p = 0.043).
The children of sedentary women weighed 3.1 ± 0.2 kg, the ones of active women weighed 3.0 ± 0.3 kg (p = 0.017). This difference was of small magnitude, although statistically significant, without clinical relevance. Since sedentary women had higher GA at the time of delivery, multivariable analysis was performed to examine the effect of physical activity on weight at birth, adjusted to GA at delivery. Thus, the association between newborn weight and maternal physical activity was not statistically significant anymore (F = 1.7, df = 1, p = 0.199), being the higher newborn weight of children of sedentary women, at the moment of delivery, explained by the GA (F = 16.3, df = 1, p < 0.001).
Among active women, 32 (86.5 %) had babies with adequate weight for the GA, while this number among sedentary women was 19 (100 %). However, the difference among proportions of appropriate and small newborns for GA was not statistically different between groups (p = 0.093).
During the day, active women stood upright for 5.5 ± 2.2 h while sedentary women spent 4.1 ± 2.2 h (p = 0.020) standing upright.
There was no significant correlation between the GA at delivery and the cervical length from the 22nd to the 24th week or from the 32nd to the 34th weeks, r = 0.04, p = 0.792 and r = −0.02, p = 0.915, respectively.
Subjects who had vaginal delivery presented cervical length from the 22nd to the 24th week and from the 32nd to the 34th week significantly shorter than subjects who underwent a C-section, 38.1 ± 7.3 vs. 44.4 ± 6.7, p = 0.015 and 27.9 ± 5.8 vs. 34.8 ± 5.2, p = 0.001, respectively.
Discussion
This study stands out for being prospective and longitudinal, adhering to the inclusion criteria and thorough sampling selection. Analyzing the possible confusion factors for differences or reduction of cervical length, it is known that younger and thinner women are more likely to deliver before time. In the most significant parts of the research, homogeneity is verified regarding age, weight, GA, and number of pregnancies at study enrollment, selection of patients for both groups, active and sedentary women, in addition to the use of specific validated questionnaire (IPAQ-SF).
Significant difference in cervical length between active and sedentary pregnant women, from the 22nd to the 24th weeks and from the 32nd to the 34th weeks was not observed.
Cervical length measured from the 22nd to the 24th week in both groups was similar, analogous to Heath et al. [9], 38 mm; Palma-Dias et al. [10], 37 mm, in Porto Alegre/RS, and Fonseca et al. [11], 34 mm.
Cervical length from the 32nd to the 34th week was similar in both groups, confirming the findings of Freitas Jr. et al. [12]. Rovas et al. [13] presented different results describing values of 23 mm in nulliparous and 30 mm in primiparous for this same GA. Therefore, the importance of strict sampling selection can be emphasized, being distributed equally to both nulliparous and primiparous groups.
In the third trimester, cervical length varied significantly in relation to the values found in the second trimester, 10.4 ± 5.4 mm (active) and 9.9 ± 5.2 mm (sedentary). This variation is expected and similar to the results of Freitas Jr. et al. [12], which demonstrated expressive cervical length reduction from the 28th week onwards.
GA at delivery was statistically lower among active women than among sedentary ones (38.2 vs. 39.1 weeks), although without clinical significance. Current evidences have been demonstrating that physical exercises do not increase prematurity rates [4, 6] agreeing with our findings, which showed no increase of deliveries before 37 weeks.
Among active women, 89.1 % had natural labor. This rate was 68.4 % among sedentary ones, an important difference with strong tendency to statistical significance. The literature is not consistent regarding higher rates of C-sections in sedentary pregnant women. Bungum et al. [14] and Lewis et al. [15] evidenced that sedentary women were twice as likely to undergo C-sections than active ones.
Our study provides an additional information for it has considered the cervical length according to the status of maternal physical activity. The fact that no difference in cervical length was found between active and sedentary women strengthens incentive prenatal attitudes regarding the adherence of a fitness program throughout pregnancy. It is known that only 15 % of pregnant women perform physical activities at levels suggested by guidelines, despite recommendations for low-risk pregnant women to perform physical activity of moderate intensity [7]. Preliminary evidences, from a Cochrane’s review, suggested that combining diet and exercise seems to be more effective than the isolated diet for maternal weight loss after delivery [16], corroborating to stimulate pregnant women to exercise.
There was no difference in weight gain during pregnancy between the groups, similar to the findings of Magann et al. [17] which did not find an association between the level of exercise during pregnancy and significant differences in maternal weight gain. Clapp et al. [18] and Olson and Strawderman [19], on the other hand, showed that decreasing exercise intensity during pregnancy leads to higher tendency of increasing weight gain.
We did not find differences in SBP, DBP, in their variation, from the first prenatal appointment to the one occurred in the 32nd week, in both groups. Saftlas et al. [20] demonstrated that women who engaged in some physical activity during pregnancy present lower rates of preeclampsia than sedentary ones. In the Cochrane Library review, the randomized work of Yeo et al. [21], despite the limited number of 16 participants, found a tendency for the reduction of DBP in active women when compared to controls (p = 0.052).
Patients who had natural labor presented cervical length, from the 22nd to the 24th weeks and from the 32nd to the 34th weeks, significantly shorter than patients who underwent a C-section. Our results were similar to the ones found by Smith et al. [22], which reported a higher incidence of C-sections among pregnant women with cervical length of 40–67 mm in the 23rd week, when compared to the ones presenting from 16 to 30 mm, confirming that cervical length in the middle of pregnancy is an independent predictor for C-section risk at term in primiparous.
Among active women, there were 32 (86.5 %) newborns appropriate for GA and 5 (13.5 %) newborns were small for the GA, while the sedentary pregnant women had 19 (100 %) newborns considered appropriate for the GA. The difference between the proportions of appropriate and small infants for the GA was not statistically different between groups (p = 0.093), which is similar to the findings of Lewis [15], indicating that the weight of the infants did not differ significantly among women who exercised and those who did not exercise during pregnancy.
Among active pregnant women enrolled in the study, time spent standing upright during the day was longer than among the sedentary ones. Despite that, there was no increased incidence of preterm labor in active women. Our results go toward current evidences that have been demonstrating that physical exercises are beneficial and that advising relative rest, since absolute rest is completely unacceptable nowadays, does not bring benefits in reducing preterm labor rates [23, 24].
Some limitations of our study must be considered. The measure of physical activity was assessed by questionnaire application (IPAQ-SF), not offering an accurate evaluation of energy expenditure precise as objective methods: pedometers and accelerometers. Despite this fact, this study is the first to assess the effects of physical activity on cervical length in two periods of pregnancy, highlighting its outline with appropriate methodological control to minimize possible confusion factors and the adherence of researchers to the inclusion and exclusion criteria adapted, strengths of this kind of investigation.
Apgar score, even though it is a subjective measure of neonate well-being at birth [25], demonstrated that children of active mothers presented outstanding scores. It is reasonable to assume, facing the results, that active mothers possibly show a better oxygenated cellular unit, which may, by cascade effect, improve fetus oxygen saturation. Here, a perspective is opened to prove at biochemical level, if these results are confirmed by gas analysis of the blood from the umbilical cord at birth.
In view of the above, our study demonstrates that among active women, there is a strong tendency favoring vaginal delivery and vigorous children in perfect conditions. This data are of expressive importance, especially when identifying that applying strategies to facilitate population access to moderate physical activities may contribute to the reduction of C-section rates, mostly in countries where, unfortunately, this mode of delivery is no exception.
Nevertheless, the sample size is still limited as well as the method to evaluate physical activity, by the use of a questionnaire. Thus, the timing of cervical changes according to the activity level remains unclear. Whether with these small numbers, the differences in Apgar score and mode of delivery are significant remains doubtful.
We conclude, based on our study, that moderate physical activity during pregnancy is not associated to cervical length reduction or preterm labor. There is still a tendency for vaginal delivery of vigorous children, being, therefore, advisable. Despite the data are still too small to allow final conclusions, maternal physical activity, cervical length and its relation to spontaneous vaginal birth at term is a relevant topic for the information of pregnant mothers already at the start of pregnancy. In the light of current evidences, the benefits attributed to physical exercise seem to justify the recommendation for moderate physical activity throughout pregnancy. More investigations directly after specific activities such as riding, walking, biking are needed to answer additional questions we receive from our patients.
References
Berghella V, Baxter JK, Hendrix NW (2009) Cervical assessment by ultrasound for preventing preterm delivery. Cochrane Database Syst Rev (3):CD007235. doi:10.1002/14651858.CD007235.pub2
Carvalho MHB, Bittar RE, Brizot ML, Bicudo C, Zugaib M (2005) Prediction of preterm delivery in the second trimester. Obstet Gynecol 105(3):532–536
Madsen M, Jorgensen T, Jensen ML, Juhl M, Olsen J, Andersen PK et al (2007) Leisure-time physical exercise during pregnancy and the risk of miscarriage: a study within the Danish National Birth Cohort. BJOG 114(11):1419–1426
Domingues MR, Barros AJ, Matijasevich A (2008) Leisure-time physical activity during pregnancy and preterm birth in Brazil. Int J Gynaecol Obstet 41(2):173–180
Morris SN, Johnson NR (2005) Exercise during pregnancy: a critical appraisal of the literature. J Reprod Med 50(3):181–188
Juhl M, Andersen PK, Olsen J, Madsen M, Jorgensen T, Nohr EA et al (2008) Physical exercise during pregnancy and the risk of preterm birth: a study within the Danish National Birth Cohort. Am J Epidemiol 167(7):859–866
ACOG Committee Obstetric Practice (2002) Committee opinion #267: exercise during pregnancy and the postpartum period. Obstet Gynecol 99(1):171–173
Matsudo SM, Araújo TL, Matsudo VKR, Andrade DR, Andrade EL, Oliveira LC et al (2001) Questionário Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Saude 10:5–18
Heath VCF, Southall TR, Souka AP, Novakov A, Nicolaides KH (1998) Cervical length at 23 weeks of gestation: relation to demographic characteristics and previous obstetric history. Ultrasound Obstet Gynecol 12:304–311
Palma-Dias RS, Fonseca MM, Stein NR, Schmidt AP, Magalhães JA (2004) Relation of cervical length at 22–24 weeks of gestation to demographic characteristics and obstetric history. Braz J Med Biol Res 37(5):737–744
Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH (2007) Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med 357(5):462–469
Freitas Jr RAO, Mauad Filho F, Duarte G, Ferreira AC, Freitas AKMSO, Azevedo GD (2003) Changes in cervical length during pregnancy measured by transvaginal ultrasound. Rev Bras Gynecol Obstet 25(2):115–121
Rovas L, Sladkevicius P, Strobel E, Valentin L (2006) Reference data representative of normal findings at two-dimensional and three-dimensional gray-scale ultrasound examination of the cervix from 17 to 41 weeks’ gestation. Ultrasound Obstet Gynecol 27(4):392–402
Bungum TJ, Peaslee DL, Jackson AW, Perez MA (2000) Exercise during pregnancy and type of delivery in nulliparae. J Obstet Gynecol Neonatal Nurs 29:258–264
Lewis B, Avery M, Jennings E, Sherwood N, Martinson B, Crain LA (2008) The effect of exercise during pregnancy on maternal outcomes: practical implications for practice. Am J Lifestyle Med 2(5):441–455
Amorim AR, Linne YM (2013) Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev (7):CD005627. doi:10.1002/14651858.CD005627.pub3
Magann EF, Evans SF, Weitz B, Newnham J (2002) Antepartum, intrapartum, and neonatal significance of exercise on healthy low-risk pregnant working women. Obstet Gynecol 99(3):466–472
Clapp JF, Kim H, Burciu B, Schmidt S, Petry K, Lopez B (2002) Continuing regular exercise during pregnancy: effect of exercise volume on fetoplacental growth. Am J Obstet Gynecol 186(1):142–147
Olson CM, Strawderman MS, Hinton PS, Pearson TA (2003) Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum. Int J Obes Relat Metab Disord 27(1):117–121
Saftlas AF, Logsden-Sackett N, Wang W, Woolson R, Bracken MB (2004) Work, leisure-time physical activity, and risk of preeclampsia and gestational hypertension. Am J Epidemiol 160:758–765
Yeo S, Steele NM, Chang MC, Leclaire Sm, Ronis DL, Hayashi R (2000) Effect of exercise on blood pressure in pregnant women with a hight risk of gestacional hypertensive disorders. J Reprod Med 45:293–298
Smith GC, Celik E, To M, Khouri O, Nicolaides KH (2008) Cervical length at mid-pregnancy and the risk of primary cesarean delivery. N Engl J Med 27(13):1346–1353
Hegaard HK (2008) Leisure-time physical activity is associated with a reduced risk of preterm delivery. Am J Obstet Gynecol 198(2):180.e1–180.e5
Matijasevich A, Domingues MR (2010) Physical exercise and preterm birth. Rev Bras Ginecol Obstet 32(9):415–419
El Beitune P, Duarte G, Campbell O, Quintana SM, Rodrigues LC (2007) Effects of antiretroviral agents during pregnancy on liver enzymes and amylase in HIV-exposed, uninfected newborn infants. Braz J Infect Dis 11(3):314–317
Acknowledgments
Dr. P. El Beitune is recipient of CNPq (National Council for Research and Technology, Brazil), fellowship number 302183/2012-4.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Portela, S.N., Rocha-de-Souza, R., Oppermann-Lisboa, K. et al. Maternal physical activity, cervical length and its relation to spontaneous vaginal birth at term. Arch Gynecol Obstet 290, 257–262 (2014). https://doi.org/10.1007/s00404-014-3198-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3198-4