Abstract
Background
The present study aimed to compare the diagnostic value of preoperative serum levels of CA125 and vascular endothelial growth factor (VEGF), and the combination of both biomarkers for differentiating early stage epithelial ovarian cancers from ovarian cysts.
Materials and methods
In this study, preoperative and postoperative serum levels of CA125 and VEGF of 30 patients with epithelial ovarian cancers (cancer arm) compared with that of 30 patients with benign ovarian cysts (cyst arm). Initial eligibility included having an ovarian cystic or solid mass detected by transvaginal ultrasonography at the hospital clinic. Included patients had to have localized pelvic disease and no clinical or imaging evidence of extrapelvic disease, ascites and distant metastasis. Initial exclusion criteria included prior history of malignancy or any type of cancer treatment. After surgery, only patients with pathologic diagnosis of early stage epithelial ovarian cancer and ovarian cyst were included.
Results
Preoperative serum levels of CA125 (P < 0.001) and VEGF (P < 0.001) were significantly higher in the study arm compared to the control arm. In addition, postoperative serum levels of CA125 (P < 0.001) and VEGF (P < 0.001) in study arm were significantly decreased compared to preoperative serum levels. At usual clinical cut-off levels of 17.6 pg/ml for VEGF and 35 U/ml for CA125, the sensitivity and specificity for detecting early stage epithelial ovary cancer were 90 and 57 % for VEGF and 66.6 and 73 % for CA125, respectively. At 100 % specificity for each test, the addition of VEGF to CA125 increased the sensitivity of early ovarian cancer detection from 60 to 73.3 %.
Conclusion
This study indicates that the addition of VEGF serum value improves the specificity and the sensitivity of CA125 to detect early stage epithelial ovarian cancers, and to differentiate these neoplasms from ovarian cyst.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adnexal masses are frequent clinical and imaging findings in women of reproductive age as well as in postmenopausal women. These masses often arise from the ovaries. In premenopausal women, the vast majority of adnexal masses are benign, particularly simple functional ovarian cyst; however, ovarian cancers are the most important differential diagnosis, particularly in postmenopausal women [1]. Ovarian cancer accounts for approximately 4 % of all cancers and 5 % of cancer mortality in women. This cancer mainly affects older population with a mean age of 63 years old [2]. Malignant epithelial neoplasms constitute the vast majority of ovarian cancers [3]. These neoplasms tend to present at advanced stage, to have high mortality rate and to be the leading cause of gynecologic cancer-related deaths [4]. Despite advanced treatments, this neoplasm remains as a fatal disease for majority of patients. Approximately 22,280 new cases of ovarian cancer will be diagnosed in 2012, and 15,500 deaths will occur from the disease [5]. However, in cases that are diagnosed at stage I, 5 years survival is 90 % [6]. Through improvement in screening and early detection, ovarian cancer survival rates will be improved. There is an increasing interest in early ovarian cancer detection as a potential method to reduce mortality. Currently, there is no evidence to demonstrate sufficient and effective screening test for ovarian cancer in the general population. Therefore, for women with general population risk, ovarian cancer screening is not suggested. However, ovarian cancer screening is critical in high risk patients with BRCA mutation having 12 to 46 % life time risk of ovarian cancer [7]. Due to the low prevalence of ovarian cancer in the general population, a positive predictive value (PPV) of 10 % has been suggested as a clinical cut-off point for screening tests for ovarian cancer. Accordingly, to achieve a PPV of 10 %, we require tests with a sensitivity of a minimum of 75 % and a specificity of more than 99.6 %. Transvaginal ultrasound (TVUS) has been investigated as screening test in ovarian cancer in the general population and in high-risk women. The results were encouraging with a positive predictive value of 14 % and negative predictive value of 99.9 %. However, TVUS is expensive as an initial screening test [8]. Circulating biomarkers are noninvasive attractive essays and essential target for research in early detection of ovarian cancer. CA-125 has been extensively evaluated as tumor marker for early detection and screening of ovarian cancer. Despite high sensitivity of this marker in advanced stage ovarian cancer, only 50 to 60 % of patients with stage I disease show elevated levels of this marker. In addition, false elevated levels of CA125 are seen in non neoplastic conditions; as well as in other benign and malignant neoplasms [9–11]. In addition, because of approximately 20 % of ovarian cancers display unremarkable levels of CA125, further serum markers, particularly in combined panel form will be required to detect all patients in an initial phase of disease [10]. Vascular endothelial growth factor (VEGF) is a cytokine-inducing endothelial cell proliferation. It has an important role in regulating tumors angiogenesis [12]. In some neoplasms, such as ovarian cancer, VEGF has been shown to be important in tumor progression, peritoneal metastasis and ascites [12, 13]. The present study aimed to compare the diagnostic value of preoperative serum level of CA125 with vascular endothelial growth factor (VEGF) for differentiating epithelial ovarian cancers from ovarian cysts.
Materials and methods
This prospective study was performed at a tertiary academic hospital during June 2008 and November 2009. The study was approved by the local university ethics committee and all the patients provided written informed consent prior to their inclusion in the study. During this time, preoperative blood samples were collected from all women with ovarian cystic and/or solid mass and who had scheduled for surgery. Initial eligibility included patients who had to be aged more than 15 years, and had an ovarian cystic or solid mass detected by transvaginal ultrasonography at the hospital clinic. Included patients had to have localized pelvic disease and without clinical or imaging evidence of extrapelvic disease, ascites and distant metastasis. Initial exclusion criteria included prior history of malignancy or any type of cancer treatment. After surgery, only patients with pathologic diagnosis of early stage epithelial ovarian cancer and ovarian cyst were included. Other pathologic diagnosis rather than epithelial cancers or ovarian cysts such as benign and non-epithelial neoplasms were excluded. Patients with gross residual or unresectable disease were also excluded. In addition, patients who had no follow-up after 3 weeks or developed wound infection were excluded from the study. Second blood sampling was performed 3 weeks after surgery from 60 consecutive eligible patients: 30 with epithelial ovarian cancer (cancer arm) and 30 with ovarian cyst (cyst arm). Preoperative evaluation included clinical examination, transvaginal ultrasonography and abdominal and pelvic computed tomography (CT) scan. Surgical management consisted of transabdominal hysterectomy and bilateral salpingo-oophorectomy (TAH + BSO) with surgical staging for those with impression of cancer, and simple cystectomy for those in cyst arm.
All blood samples were collected in sterile tubes, centrifuged at 2,000g for 10 min, and then stored in a freezer at −20 °C until assay. The concentrations of Serum CA125 and VEGF were determined as serum immunoreactivity using a quantitative sandwich enzyme immunoassay technique. According to the manufacturers, the usual clinical cut-off levels for biomarker values were defined as 35 U/ml for CA125 and 17.6 pg/ml for VEGF; however, in this study various sensitivity and specificity for various cut-off values were calculated.
Statistics
To define a case as positive or negative, we initially determined the cut-off values of each marker for resulting in 100 % specificity in our data set. Subsequently, any case with levels higher than cut-off point values was considered as positive for each marker. All statistical analyses were performed with SPSS statistical package version 17.0 (SPSS, Chicago, IL). The Mann-Whitney test was used to compare Serum CA125 and VEGF values in different groups. Frequency tables were analyzed by the Chi squared test or Fisher’s exact test. Using receiver operating characteristics (ROC), the area under the curve (AUC), sensitivity and specificity were determined for each biomarker values. According to the published coefficients of variation for the studied parameters, a minimum of 30 patients in each arm were required for demonstrating possible statistical differences with a significance level of 5 %. All P values were 2-tailed and P values less than 0.05 were considered statistically significant.
Results
In all, 60 women were evaluated. All cancer patients were of stage I (n = 21) or stage II (n = 9) disease. The mean age of 30 patients in cancer arm was significantly higher (51.23 vs. 28 years) than that in cyst arm (P < 0.001). Accordingly, postmenopausal status was more frequent in cancer arm. In cancer arm, histological types were serous (n = 15), endometrioid (n = 11), mucinous (n = 2) and poorly differentiated (n = 2) type. The mean age, menopausal status, histological types, disease stage, area under the ROC curve, and serum CA125 and VEGF levels among cancer and cyst arms are shown in Table 1. As seen in Table 1, the areas under the ROC curves were significantly higher for both biomarkers in cancer arm compared to cyst arm. (Table 1) The mean preoperative VEGF serum level was significantly higher (47.84 vs. 20.49, P value < 0.001) in cancer arm compared to cyst arm. Similarly, the mean preoperative CA125 serum level was significantly higher (143.38 vs. 28.61, P value < 0.001) in study arm than that of control arm. The mean preoperative VEGF serum level was significantly higher (47.8 vs. 13.8, P value < 0.00) than postoperative values. Similarly, the mean preoperative CA125 serum level was significantly higher (143.4 vs. 9.2, P value < 0.001) than postoperative values. A descriptive statistics of serum CA125 and VEGF levels in ovarian cyst and cancer patients are shown in Table 2.
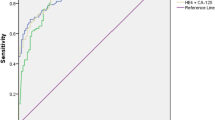
We performed ROC analysis for illustration of biomarkers discrimination in all cancer arm (Fig. 1), stage I (Fig. 2), stage II (Fig. 3), as well as in postmenopausal patients (Fig. 4). According to ROC analysis, the power to discriminate between cancer and cyst arms was higher for VEGF in all cancer stages (AUC for VEGF was 0.895 vs. 0.809 for CA125) (Fig. 3).
In addition, through linear regression analysis, we found a low determination coefficient between the VEGF and CA125 values in all the study population [r 2 = 0.2410 (r = 0.49)].
To investigate the value of preoperative CA125 and VEGF levels in detecting ovarian cancer, we calculated sensitivity and specificity of each biomarker alone and the combination of both biomarkers for various cut-off values. At cut-off levels of 17.6 pg/ml for VEGF and 35 U/ml for CA125, the sensitivity and specificity for detecting early stage epithelial ovary cancer were 90 and 57 % for VEGF and 66.6 and 73 % for CA125, respectively. At 100 % specificity for each test, the addition of VEGF to CA125 increased the sensitivity of early ovarian cancer detection from 60 to 73.3 %. In addition, by lowering the specificity of VEGF to 96.7 %, while keeping the same CA125 cut-off, the sensitivity increased to 80 % for stage I/II. Table 3 shows the sensitivities of each biomarker and their combination for the different cancer stages at 100 % specificity. In a scatterplot in Fig. 5, the 100 % specificity cut-off values for VEGF and CA125 are shown in all study population.
Discussion
Currently, early detection and screening is the most effective approach for improving survival in patients with epithelial ovarian cancer. These neoplasms mainly present as asymptomatic or symptomatic adnexal masses [6]. Ovarian cysts are among the most common benign adnexal masses mimicking the signs and the symptoms of ovarian cancer. Imaging studies were investigated as diagnostic tools for differentiating adnexal masses [1]. In a systematic review, color Doppler ultrasonography was found as a useful predicting test for preoperative diagnosis of pelvic masses, with a sensitivity of 87 % and a specificity of 92 % [14]. Transvaginal ultrasonography is another imaging modality frequently used as diagnostic method to evaluate pelvic organs including. However, this method lacks sufficient sensitivity and specificity for early detection ovarian tumors. In addition, these imaging modalities are expensive, operator dependent and mainly tend to depend on the size rather than the nature of ovarian mass [8].
Biomarkers are non-invasive potential useful diagnostic and screening tests in ovarian cancer, particularly in asymptomatic early stage lesions. To date, over 200 potential biomarkers have been identified for ovarian cancer; however, a golden standard biomarker or optimal combined screening test has not yet been established [15]. Measurement of CA125 and other serologic markers, vaginal ultrasonography, and combinations of these modalities may be useful for screening and early detection in epithelial ovarian cancer. CA125 is a glycoprotein biomarker that is usually expressed by serous ovarian tumors, some mucinous papillary tumors and less frequently in other histological types. This biomarker is well correlated with disease stage and bulk of the tumor. The CA125 alone is not sufficiently sensitive or specific to be diagnostic for epithelial ovarian cancer. This biomarker is increased in 80 % of patients with advanced disease, but many patients with epithelial ovarian cancer, particularly in 50 % of early stage disease do not show elevated levels of the marker. Therefore, it is not a cost-effective screen test for asymptomatic patients [9–11].
Despite extensive studies in the past two decades in ovarian cancer screen, recent statistics advocate that more investigations are required to the discovery of novel ovarian cancer biomarkers [15]. A variety of serum biomarkers such as Human Epididymis Protein 4 (HE4) have been investigated and combined to CA125 for providing higher sensitivity and specificity than CA 125 alone [9, 16].
Angiogenesis is an essential step for the tumor growth. Vascular endothelial growth factor (VEGF) is one of the most important angiogenesis stimulators and plays a critical role in the neovascularization of human tumors. VEGF is overexpressed in many malignant neoplasms. There is a correlation between serum VEGF level and disease stage and primary tumor size.
VEGF consists of five subtypes and they promote tumor growth and angiogenesis via receptors on endothelial cells [13]. VEGF is excreted via kidney and urinary levels have been shown to be more in cancerous patients than in healthy people. This cytokine is found in effusion fluids in malignant diseases and also in benign situations such as wound healing fluids. VEGF increases in serum and plasma in cancer patients [17]. There are very limited studies investigating the diagnostic impact of VEGF serum level in screening and early detection of ovarian cancer. The results of these studies are uniformly consistent with our study results and show a significant higher concentration of VEGF serum levels in ovarian cancer patients compared to benign ovarian and healthy control cases [2, 18–21]. Demirkiran et al. in a study measured VEGF in benign ovary cysts and malignant ovary tumors. VEGF was significantly higher in malignant lesions. The serum level was also higher in cancer group (0.72 ± 0.17 ng/ml) in malignant lesions compared with benign cysts (0.33 ± 0.11 ng/ml, P < 0.001). In their study, tumor grade had no relation with VEGF levels [2]. In another study, VEGF level correlated with operation success. After operation the decrease in VEGF level was in relation with the presence of residual disease [19]. Candido Dos Reis et al. in a similar study investigated the value of VEGF serum and cyst level concentrations in differentiation of benign and malignant ovarian tumors. They found significantly higher levels of VEGF in serum and cyst fluid for malignant and borderline tumors compared with benign cysts [20]. Likewise, Cooper et al. assessed the clinical significance of VEGF serum levels in differentiation of patients with benign adnexal masses from those with ovarian cancer. They found a significant higher mean preoperative VEGF serum level in cancer patients compared to patients with benign adnexal masses [21].
In the present study, we investigated the potential use of VEGF serum values as a diagnostic test for early stage ovarian cancer and its combination with CA125 serum values as a screening approach with higher sensitivity to differentiate ovarian cancer from ovarian cyst. We found VEGF serum levels were significantly higher in patients with early stage ovarian cancer compared to those with ovarian cyst; as well as to postoperative cancer patients. In this study, by considering a 100 % specificity for each test, we eliminated any false positive results among women with ovarian cyst to achieve a combined screening test for detecting about third-fourth of patients with early epithelial ovarian cancer.
These results confirm our hypothesis that VEGF serum value is a useful diagnostic test for detection of early stage ovarian cancer. This test enhances the sensitivity and specificity of CA125 for screening early stage epithelial ovarian cancer and differentiating these neoplasms with ovarian cyst. However, the small sample size of 30 patients in each arm and the lack of healthy aged-matched control arm limit the power of our study.
Further large-scale studies are warranted to further examine the accuracy of VEGF alone and in combination with CA125 or others biomarker for early detection and screening of ovarian cancer.
Conclusion
This study indicates that VEGF serum value is a potential useful biomarker in epithelial ovarian cancer. It has a higher sensitivity compared to CA125 in early stage ovarian cancer. The addition of VEGF serum value improves the specificity and the sensitivity of CA125 to detect early stage epithelial ovarian cancers, and to differentiate these neoplasms from ovarian cyst.
References
Perez-Lopez FR, Chedraui P, Troyano-Luque JM (2010) Peri- and post-menopausal incidental adnexal masses and the risk of sporadic ovarian malignancy: new insights and clinical management. Gynecol Endocrinol 26(9):631–643. doi:10.3109/09513590.2010.487611
Demirkiran F, Kumbak B, Bese T, Arvas M, Benian A, Aydin S, Uzun H, Sanioglu C, Aydinli K, Kosebay D (2003) Vascular endothelial growth factor in adnexal masses. Int J Gynaecol Obstet 83(1):53–58
Kaku T, Ogawa S, Kawano Y, Ohishi Y, Kobayashi H, Hirakawa T, Nakano H (2003) Histological classification of ovarian cancer. Med Electron Microsc 36(1):9–17. doi:10.1007/s007950300002
Fotopoulou C, Richter R, Braicu IE, Schmidt SC, Neuhaus P, Lichtenegger W, Sehouli J (2011) Clinical outcome of tertiary surgical cytoreduction in patients with recurrent epithelial ovarian cancer. Ann Surg Oncol 18(1):49–57. doi:10.1245/s10434-010-1245-3
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62(1):10–29. doi:10.3322/caac.20138
Barnholtz-Sloan JS, Schwartz AG, Qureshi F, Jacques S, Malone J, Munkarah AR (2003) Ovarian cancer: changes in patterns at diagnosis and relative survival over the last three decades. Am J Obstet Gynecol 189(4):1120–1127
King MC, Marks JH, Mandell JB, New York Breast Cancer Study G (2003) Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302(5645):643–646. doi:10.1126/science.1088759
van Nagell JR Jr, DePriest PD, Ueland FR, DeSimone CP, Cooper AL, McDonald JM, Pavlik EJ, Kryscio RJ (2007) Ovarian cancer screening with annual transvaginal sonography: findings of 25,000 women screened. Cancer 109(9):1887–1896. doi:10.1002/cncr.22594
Moore RG, MacLaughlan S, Bast RC Jr (2010) Current state of biomarker development for clinical application in epithelial ovarian cancer. Gynecol Oncol 116(2):240–245. doi:10.1016/j.ygyno.2009.09.041
Bast RC Jr, Badgwell D, Lu Z, Marquez R, Rosen D, Liu J, Baggerly KA, Atkinson EN, Skates S, Zhang Z, Lokshin A, Menon U, Jacobs I, Lu K (2005) New tumor markers: CA125 and beyond. Int J Gynecol Cancer 15(Suppl 3):274–281. doi:10.1111/j.1525-1438.2005.00441.x
Einhorn N, Sjovall K, Knapp RC, Hall P, Scully RE, Bast RC Jr, Zurawski VR Jr (1992) Prospective evaluation of serum CA 125 levels for early detection of ovarian cancer. Obstet Gynecol 80(1):14–18
Orre M, Rogers PA (1999) VEGF, VEGFR-1, VEGFR-2, microvessel density and endothelial cell proliferation in tumours of the ovary. Int J Cancer 84(2):101–108
Su JL, Yen CJ, Chen PS, Chuang SE, Hong CC, Kuo IH, Chen HY, Hung MC, Kuo ML (2007) The role of the VEGF-C/VEGFR-3 axis in cancer progression. Br J Cancer 96(4):541–545. doi:10.1038/sj.bjc.6603487
Medeiros LR, Rosa DD, da Rosa MI, Bozzetti MC (2009) Accuracy of ultrasonography with color Doppler in ovarian tumor: a systematic quantitative review. Int J Gynecol Cancer 19(7):1214–1220. doi:10.1111/IGC.0b013e3181a386e5
Suh KS, Park SW, Castro A, Patel H, Blake P, Liang M, Goy A (2010) Ovarian cancer biomarkers for molecular biosensors and translational medicine. Expert Rev Mol Diagn 10(8):1069–1083. doi:10.1586/erm.10.87
Moore RG, McMeekin DS, Brown AK, DiSilvestro P, Miller MC, Allard WJ, Gajewski W, Kurman R, Bast RC Jr, Skates SJ (2009) A novel multiple marker bioassay utilizing HE4 and CA125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol 112(1):40–46. doi:10.1016/j.ygyno.2008.08.031
Kut C, Mac Gabhann F, Popel AS (2007) Where is VEGF in the body? A meta-analysis of VEGF distribution in cancer. Br J Cancer 97(7):978–985. doi:10.1038/sj.bjc.6603923
Tan X, Shen K, Liu D, Xu X, Lang J (2000) The diagnostic and prognostic values of assay of serum vascular endothelial growth factor in epithelial ovarian cancer. Zhongguo yi xue ke xue yuan xue bao Acta Academiae Medicinae Sinicae 22(4):352–355
Oehler MK, Caffier H (2000) Prognostic relevance of serum vascular endothelial growth factor in ovarian cancer. Anticancer Res 20(6D):5109–5112
Candido Dos Reis FJ, Moreira de Andrade J, Bighetti S (2002) CA 125 and vascular endothelial growth factor in the differential diagnosis of epithelial ovarian tumors. Gynecol Obstet Invest 54(3):132–136. doi:67877
Cooper BC, Ritchie JM, Broghammer CL, Coffin J, Sorosky JI, Buller RE, Hendrix MJ, Sood AK (2002) Preoperative serum vascular endothelial growth factor levels: significance in ovarian cancer. Clin Cancer Res 8(10):3193–3197
Acknowledgments
This study was supported by Shiraz University of Medical Sciences. The authors would like to thank the clinical research development of Namazi Hospital for statistical consulting; and Research Improvement Center of Shiraz University of Medical Sciences, Shiraz, Iran and Ms. A. Keivanshekouh for improving the use of English in the manuscript.
Conflict of interest
None of the authors has any conflict of interest, financial or otherwise.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Robati, M., Ghaderi, A., Mehraban, M. et al. Vascular endothelial growth factor (VEGF) improves the sensitivity of CA125 for differentiation of epithelial ovarian cancers from ovarian cysts. Arch Gynecol Obstet 288, 859–865 (2013). https://doi.org/10.1007/s00404-013-2819-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-2819-7