Abstract
Objective
To determine the prevalence, types and correlates of intimate partner violence (IPV) in pregnant Nigerian living with HIV.
Design
Cross sectional study.
Population
HIV positive pregnant women.
Setting
A large HIV comprehensive treatment centre.
Methods
A cross sectional study of 652 HIV positive pregnant Nigerians seen at Nigerian Institute of Medical Research, Lagos, Nigeria over a 24 months period.
Main outcome measures
Prevalence of intimate partner violence after HIV diagnosis.
Results
Among the women interviewed, 423 (65.8%) reported abuse. In 74.0% of abused women, the abuse started after HIV diagnosis. Though having a HIV negative spouse and disclosure of HIV status were associated with abuse, only having a HIV negative partner retained its association with IPV (OR 3.1; CI 2.4–5.3) after controlling for confounding variables. Sixty-two (9.6%) women have not disclosed their HIV status because of fear of rejection. Verbal abuse (51.7%), threat of violence in 97 (22.9%) and sexual deprivation in 91 (21.5%) were the common forms of abuse reported.
Conclusion
IPV is common among HIV positive pregnant Nigerians; with a threefold increased risk in women in HIV serodiscordant relationship.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The World Health Organisation defined intimate partner violence (IPV) against women as “the range of sexually, psychologically and physically coercive acts used against adult and adolescent women by current or former male intimate partners” [1]. IPV is an important problem because it is global, the most common form of violence against women, violates fundamental human rights of women, and is a major public health problem [2, 3]. Abused individuals may also suffer from a sense of helplessness and fatalism that further undermines one’s interest and ability to maintain health and adopt disease coping mechanisms [4].
Between 20 and 50% of women reported experiencing violence by an intimate male partner [5, 6]. In sub-Saharan Africa, the reported prevalence of IPV ranges from 20 to 71% [5, 7, 8]. However, the prevalence of IPV is believed to be under-estimated because of under-reporting and lack of standardized methods for the estimation of IPV [9, 10].
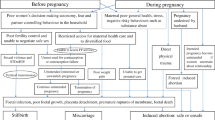
Intimate partner violence is associated with high levels of negative physical and mental health outcomes and associated with socio-demographic, cultural, lifestyle factors, and HIV status [11–13].
The links between HIV/AIDS and gender-based violence are becoming increasingly apparent. A review of some of the existing studies suggests that gender-based violence makes women vulnerable to HIV through three main mechanisms [14]. First, and most obvious, there is the possibility of direct transmission through forced or coerced sexual acts. Second, the trauma associated with violent experiences can impact later sexual behaviour. Third, violence or the threat of violence may limit women’s ability to adopt safer sex practices within on-going relationships. Also of significant importance is the emerging evidence that being HIV positive is a risk factor for violence against women. Several studies undertaken in the US and South Africa indicate a positive relationship between HIV/AIDS and domestic violence [15, 16]. Also the notification of a positive HIV test result can profoundly affect a woman’s psychological and physical well-being [17–19]. The stigma associated with HIV can cause women to experience feelings of isolation and shame. HIV-infected people often fear rejection and abandonment following disclosure of their status [17, 18]. These concerns keep some women from disclosing to others even when they would like to, and for some, disclosure has in fact led to negative consequences, including violence [17–19].
This relationship has grave consequences as its impacts affect negatively on HIV status disclosure [15, 16]; considered to be important for ensuring that HIV positive individuals are able to access a range of services including prevention of mother-to-child transmission (PMTCT), anti-retroviral treatment (ART), and psychosocial support [20].
In our settings, HIV-1 testing may place women at risk of domestic violence, and fear of domestic violence (physical, financial, or psychological abuse) may make it difficult for women to access interventions to prevent mother-to-child transmission of HIV-1 [18]. There is therefore a need to understand how domestic violence interacts with PMTCT programmes. In our PMTCT programmes, women are encouraged to disclose their status to their partners because of previously reported association between male involvement and acceptance of PMTCT intervention strategies.
The recent reports of association of HIV status disclosure and violence have raised concerns. In light of these findings, some women’s advocates have questioned the rational of continued encouragement of women to disclosure their status with the possibility of a negative consequence.
Studies on domestic violence after HIV-1 testing in sub-Saharan Africa have not consistently found an association between HIV-1 test results and domestic violence. While some studies reported high rates of domestic violence, divorce, or separation [19, 21, 22], others did not found that partner notification of positive HIV-1 results increases the risk of post test domestic violence, divorce, or separation after testing [23–25]. Majority of those studies were either from east or southern Africa.
In order to contribute to the growing literature on the relationship of IPV to HIV/AIDS in pregnant women, especially in west African sub-region, where there is still paucity of data, we carried out the current study on women receiving PMTCT services in a large HIV treatment centre in Lagos Nigeria. In this study, we examined the frequency, pattern and correlates of intimate partner violence among pregnant HIV positive Nigerian women.
Methods
Study setting
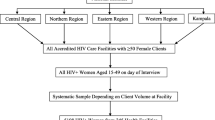
This cross sectional study was conducted at HIV treatment centre, Nigerian Institute of Medical Research (NIMR), Yaba, Lagos. NIMR is the apex medical research institute in the country. Though the mandate of the institute stipulates that it shall conduct research into diseases and problems of public health importance in the country; however, the emergence of HIV infection as a major health problem in the country and the need to provide specialized and prompt care to HIV infected Nigerians prompted the FGN to add a service component to this mandate.
The HIV treatment clinic started operations in the year 2002 with approval to provide care to only 250 adults of 10,000 planned by the FGN nationwide. NIMR was appointed to provide the research component to the FGN HIV treatment access programme. In 2004, NIMR HIV clinic became one of the six pioneer sites in Nigeria implementing The US President Emergency Programe For AIDS Relief (PEPFAR) in collaboration with Harvard School of Public Health, Boston, MA. With this support, the clinic was enlarged to provide paediatric and PMTCT services as well as TB treatment. The laboratory back ups are provided by The Human Virology Laboratory and TB Reference Laboratory of the Institute. The inpatient facilities are provided by 68 military Hospital, Yaba, Lagos, and Lagos University Teaching Hospital, Idi Araba, Lagos. Intrapartum and delivery services are provided by Ayinke House, Lagos State University Teaching Hospital, Ikeja, Lagos, Lagos University Teaching Hospital, Idi Araba, Lagos and Sacred Heart Hospital, Lantoro, Abeokuta, Havana Specialist Hospital and Rao Specialist Hospital, Lagos.
The clinic’s patients have grown from 250 in 2002 to over 10,000 by June 2008. The clinic population is heterogeneous and includes men, women (including pregnant ones), children and young people from various walks of life and from diverse ethnic, economic, religious and sociocultural backgrounds. These patients are referred from both private and public health institutions in different parts of the Lagos state and the neighbouring states of Ogun, Ondo, Oyo, Osun and Edo, with many others coming from states in other geopolitical zone and neighbouring country, Benin Republic. The clinic operates 5 days a week with 1 day (Wednesday) reserved only for PMTCT and HIV exposed babies.
Study population
The study population was HIV positive pregnant women receiving PMTCT services at the HIV treatment centre, NIMR Lagos between January 2006 and December 2007.
Pilot study
The questionnaire used for the study was a modification of the one used for a previous study in our environment [1]. It was modified to the extent to include information on HIV status. The modified questionnaire was pilot tested in 50 consecutive consenting HIV positive pregnant women before the commencement of the actual study. The test run of data collection was carried out under same conditions identical as in the main research study. This tested the ability of the participants to understand and answer the questions. It was used to correct some ambiguous and complex questions. All the necessary changes and adjustments to the questionnaire were made before the main study. The pilot study also provides the researcher and the trained interviewers with the experience required to administer the questionnaires. Essentially, this piloting ensured that the main structure is appropriate and that bias and error are limited.
Ethical considerations
Ethical approval was obtained from the ethical committee of the Nigerian Institute of Medical Research, Yaba, Lagos for all components of our HIV programme. Patients enrolled into our HIV programme are counseled at entry and signed a written informed consent that data and information generated from their care to be used for research purposes. In addition, ethical approval was sought and obtained for this specific study, as the previous ethical approval did not specifically cover this aspect of research. Verbal informed consent were also sought and obtained from the patients before administering the questionnaires. However, consent was explicitly sort in the introductory section of the study questionnaire (Table 1) by statement “It is pertinent to mention that your consent is documented by your agreement to complete the questionnaire”, it was specifically stated that consent is assumed by subjects completing the questionnaires. Confidentiality was maintained by not releasing the information obtained to a third party. Anonymity was also maintained by avoidance of participant’s identifiers on the questionnaires. Only consenting patients were recruited for the study. To avoid undue influence on the women, the questionnaires were administered by training interviewers/counselors and not by their attending clinicians. The women who could not read and write were assisted by the trained interviewers/counselors to complete the questionnaires in the presence of peer volunteers (PLWHAs).
Sample size and data management
Survey items were socio-demographic characteristics, history of abuse before and after HIV diagnosis and client’s attitude and willingness to report abuse (see Table 1). Clients were enrolled consecutively until December 2007. However, it was planned that if sample size is not achieved, the study period will be extended. Sample size calculation was based on prevalence of domestic violence during pregnancy of 11.7% in our previous study [1]. The minimum sample size for statistically significant survey was obtained by using the formula:
where n, minimum sample size for statistically significant survey, z normal deviant at the position of 95% confidence level = 1.96, p, prevalence rate, d, margin of sampling error acceptance or measure of precision = 5%
Data entry and analysis were performed using the Statistical Package for Social Sciences (SPSS) for windows statistical package version 10.0 (SPSS Inc., IL, USA). Frequency tables were computed for all variables. Continuous variables such as age and parity were treated as individual elements and then as combined summary measures. The presence of an association between the hypothesized determinants and domestic violence were tested using univariate analysis. Test of statistical significance based on 95% confidence interval of Chi-square with Yates correction, Fisher’s exact test and Student’s t test as appropriate were used to determine significant determinants. The significant variables at univariate analysis were subjected to multiple logistic regressions using SPSS statistical software package, their odd ratio were calculated to determine the independent determinant factors, while controlling for confounding variables of age, parity, occupation and educational status.
Definitions
Intimate partner violence (IPV) is an abuse that occurs between two people in a close relationship. The term “intimate partner” includes current and former spouses and dating partners.
IPV for purposes of this study includes four types of behaviour:
-
Physical abuse—hurting or tries to hurt a partner by hitting, kicking, burning, or other physical force.
-
Sexual abuse—forcing a partner to take part in a sex act when the partner does not consent.
-
Threats of physical or sexual abuse include the use of words, gestures, weapons, or other means to communicate the intent to cause harm.
-
Emotional/psychological abuse—threatening a partner or his or her possessions or loved ones, or harming a partner’s sense of self-worth, e.g. stalking, name calling, intimidation, or not letting a partner to see friends and family. It also includes intentional withholding of financial support or being forbidden to earn.
Results
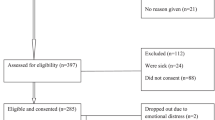
During the period of study, a total of 683 pregnant HIV positive women were approached to participate in the study. Six hundred and sixty-seven (97.1%) HIV positive women accepted to participate in the study, while 20 (2.9%) decline to participate citing various reasons. The reason for declining participation in the 20 women ranged from “need the spouse consent” in 8 (41.7%) women, no reason in 3 (25.0%), “not interested” in 2 (16.7%), “need to think about it” in 1 (8.3%) and “I have no time” in 1 (8.3%). Eleven (2.8%) HIV positive women returned questionnaire, had missing information and were thus excluded from the analysis. Thus only 652 (97.8%) questionnaire with complete information were used for analysis; 95.5% of the original sample population.
Among the 652 women with complete questionnaire, 65.7% (428) reported a life time history of abuse. The socio-demographic characteristics of the women and the HIV status of their spouse are shown in Table 2. Of the socio-demographic characteristics studied, it was only in the women’s social economic class and spouse’ HIV status that was shown to be associated with increased risk of violence. Low socioeconomic class was shown to be associated with increased prevalence of IPV (P = 0.000). Also unknown and negative HIV status of women’s spouse was associated with IPV (P < 0.005). However, after controlling for possible confounding factors of age, occupation, parity and educational status, it was only HIV status of the spouse that retained its association with IPV (OR 2.01; CI 1.45–5.67).
Further segregation of the women that reported history of abuse showed that, while the abused pre-dated HIV diagnosis in 111 (25.9%) cases, in the majority of the women (74.1%) abuse started after diagnosis of HIV. In the 111 women, that history of abuse predated HIV diagnosis, 59 (53.2%) reported that abuse has increased since they were diagnosis HIV positive, 33 (29.7%) reported no change and 19 (17.1%) reported no abuse since diagnosis. Thus 409 (62.7%) of the 652 respondents had been abused since HIV diagnosis compared to 111(17.0%) before diagnosis.
Table 3 showed the relationship between selected socio-biological characteristics and abuse history before and after HIV diagnosis. Having a HIV negative spouse and disclosure of HIV positive status to the spouse were associated with abuse after HIV diagnosis in women that had never been abused before the diagnosis. However after controlling for confounding factors of age, parity, educational status, tribe, socioeconomic class, spouse with HIV negative status only retained its association with intimate partner abuse (OR 3.1; CI 2.4–5.3).
Sixty-three (9.6%) of the women studied have not disclosed their status because of fear of stigma, rejection and possible abuse by their spouse.
Verbal abuse was the commonest (221; 51.7%) form of abuse reported by the women. Other forms of abuse reported includes economic deprivation in 67 (15.7%), physical abuse in 35 (8.1%), sexual deprivation in 92 (21.6%), threat of violence in 89 (20.8%), husband parking out of the house/eloping with their kids in 13 (3.0%), informing relations of her HIV serostatus in 9 (2.1%), forced to leave her home in 7 (1.7%) and forced sex in 6 (1.3%).
In none of the patients were the abuse severe enough to warrant hospital visit/treatment or pose a threat to the fetomaternal well being. All, but one woman engaged the services of a lawyer to prevent being thrown out of her house by her HIV negative spouse. The rest were afraid to report because of fear of making her status public.
The spouse was the perpetrators of the violence in the majority of cases (89.4%). The finance/boy friend and spouse’s relations were the perpetrators in 38 (8.9%) and 4 (7.3%), respectively.
Discussion
The purpose of this study was to better understand the relationship between HIV status and pattern and frequency of domestic violence against pregnant women in environment. Also investigated are the correlates of the association if any. The findings from this study not only confirmed a high rate of domestic violence, especially after HIV diagnosis, it also revealed that a number of women are not willing to disclose or report abuse. Thirty-one (4.5%) respondents declined to participate in the study either out rightly or by returning uncompleted questionnaires citing “need husband consent”, “no reason”, “not interested” and “have no time” as reason for not participating. Our previous study on domestic violence among pregnant of unknown status and those of Stewart, Multhal-Rathore et al. reported similar findings [5, 26, 27]. This reluctance have been attributed to the women’s fear of reappraisal attack/further abuse following such reported [5, 26]. In the context of HIV/AIDS, the situation may even be worse because of the associated stigma and discrimination.
Four hundred and twenty-eight (65.7 %) of 652 women that returned their questionnaire completed reported history of intimate partner violence. Detailed analysis also showed that while the abused pre-dated HIV diagnosis in 111 (25.9%) cases, in the majority of the women (74.1%) abuse started after diagnosis of HIV. In the 111 women that history of abuse predated HIV diagnosis, 59 (53.2%) reported that abuse has increased since they were diagnosis HIV positive, 33 (29.7%) reported no change and 19 (17.1%) reported no abuse since diagnosis. Thus 409 (62.7%) of the 652 respondents had been abused since HIV diagnosis compared to 111(17.0%) before diagnosis. These findings confirm those of previous studies that domestic violence is associated with HIV infection [28–30]. This relationship may either be casual or effect of the HIV diagnosis. Abused women are not only unable to negotiate sex, but their male partners’ behaviour of infidelity and having multiple sexual partners also places them at a risk of HIV infection [28]. Thus domestic violence interventions that target reasons for conflicts may have additional benefit of preventing HIV infection. Past research also reports women’s concern about stigma, rejection and violence related to disclosing their HIV seropositive status. In this study, the prevalence of violence increased from 17.0% pre-HIV diagnosis to 62.7% post-HIV diagnosis. Defeu et al. [31] also documented that negative reactions to disclosure are common; including making the information available to other people, negative reactions from partners including physical abuse and abandonment. In another study, 45% of the adults who have experienced relationship violence reported that it was the result of their HIV infection [32].
The results from this study have important implications for the prevention of HIV and violence against women. Women in settings like ours are at a risk for both HIV infection and violence largely because of the behaviour of partners, especially so when some level of violence is seen as normal by the larger society [5, 29]. Therefore, the foundation of any violence prevention and control programme must include efforts to raise community awareness and to develop critical attitudes towards domestic violence. Promoting an ethic of responsibility among men for the health and well being of their intimate partner is needed. Efforts to change norms surrounding conflict resolution and sexual behaviour are necessary and important parts of any global women’s health promotion strategy [5, 29].
Another important finding in this study is that though the overall prevalence of domestic violence is higher than that reported in women of unknown HIV status from similar environment, the pattern of violence remained the same [5].
Violence after HIV diagnosis was associated with having a HIV negative spouse and disclosure of HIV positive status to the spouse. However after controlling for confounding variables, only HIV negative partner remain strongly associated with intimate partner abuse (OR 3.1; CI 2.4–5.3). In our community, being HIV positive is synonymous with being promiscuous. It is therefore not surprising that prevalence of domestic violence increased, as the HIV negative spouse will see the woman as promiscuous and not faithfully him.
Despite the important findings from this study, it should be viewed in the light of some limitations. First is the study population size. Though the number studied is smaller than in some previous studies [7, 8, 28–30], the number of women studied in this study being twice the sample size calculated, based on a previous study in our environment ensures the adequacy of the sample to detect association between IPV and independent factors. The study population is much larger than any other study on same subject from our environment [1]. Second is asking women to recall violent events present some of these limitations, including female minimalization of experiences of violence [29], and inaccurate recall of past events. However to minimize recall bias, we only asked about violent events before and after HIV diagnosis. Also no use of HIV negative control makes it rather difficult to make some definite conclusion. We only made comparison between findings in this study and other studies that studied HIV negative women. It is also important to note that our clinic being a specialized public clinic, the population studied might not be a true representative of the catchment population. Some privileged and very poor women may have been excluded because of the nature of the clinic.
Therefore, our findings should be interpreted with these limitations in mind and only be generalized to women who are HIV positive. However, it has potentially important implications for programmes aimed at preventing violence and HIV.
Conclusion
This study shows that the diagnosis of HIV infection is associated with increased violence, and especially so in women with HIV positive spouses. All effort geared towards HIV prevention and control should also address the issue of domestic violence.
References
WHO/WHD world report on violence (1997) Geneva, World Health Organisation
WHO/WHD world report on violence (1997) Geneva, World Health Organisation
Kaye DK, Mirembe FM, Bantebya G, Johansson A, Ekstrom AM (2006) Domestic violence as a risk factor for unwanted pregnancy and induced abortion in Mulago Hospital, Kampala, Uganda. Trop Med Int Health 11:90–101. doi:10.1111/j.1365-3156.2005.01531.x
Leung SJ, Tesoriero JM, Klein SJ, Heavner KK, Battles HB, Nemeth C, Birkhead GS (2005) Intimate partner violence and HIV testing history among high risk individuals (abstract no. Wo-A1602). National HIV prevention conference Atlanta, Georgia, June 12–15
Ezechi OC, Kalu BKE, Ezechi LO, Nwokoro CA, Ndububa VI, Okeke GCE (2004) Prevalence and pattern of domestic violence against pregnant Nigerian women. J Obstet Gynaecol 24(6):652–656. doi:10.1080/01443610400007901
Heise L, Ellsberg M, Gottmoeller M (1999) Ending violence against women. Population report, series L, No. 11. Population Information Program, Center for Communication Programs, Johns Hopkins University School of Public Health, 111 Market Place, Suite 310, Baltimore, Maryland 21202–4012, USA
Koenig MA, Lutalo T, Zhao F, Nalugoda F, Wabire-Mangen F, Kiwanuka N, Wagman J, Serwadda D, Wawer M, Gray R (2003) Domestic violence in rural Uganda: evidence from a community based study. Bull World Health Organ 81:53–60
WHO: WHO multi-country study on women’s health and domestic violence (WHO/FCH/GWH/02.01)
Heise L, Ellsberg M, Gottmoeller M (1999) Ending violence against women. Population report series L No. 11. Population Information Program, Center for Communication Programs, Johns Hopkins School of Public Health, 111 Market Place, Suite 310, Baltimore, Maryland 21202–4012, USA
Karamagi CAS, Tumwine JK, Tylleskar T, Heggenhougen K (2006) Intimate Partner Violence against women in eastern Uganda: Implications for HIV Prevention. BMC Public Health 6:284–288. doi:10.1186/1471-2458-6-284
Ellsberg MC, Rena R, Herrera A, Liljestrand J, Winkvist A (1999) Wife abuse among women of childbearing age in Nicaragua. Am J Public Health 89:241–244. doi:10.2105/AJPH.89.2.241
Suzanne M, Mbwambo JK, Hogan NM, Kilonzo GP, Campbell JC, Weiss E, Sweat MD (2002) HIV positive women report more life time partner violence: findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. Am J Public Health 92:1331–1337. doi:10.2105/AJPH.92.8.1331
Rao V (1997) Wife beating in rural South India: a qualitative and econometric analysis. Soc Sci Med 44:1169–1180. doi:10.1016/S0277-9536(96)00252-3
Maman S, Campbell J et al (2000) The intersections of HIV and violence: directions for future research and investigations. Soc Sci Med 50:459–478
Ward J (2002) If not now? Addressing gender-based violence in refugee, internally displaced and post-conflict settings, Reproductive Health for Refugees consortium, Washington DC, http://www.rhrc.org/resources/gbv/ifnotnow.html
Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD (2004) Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet 363:1415–1421. doi:10.1016/S0140-6736(04)16098-4
Gielen AC, McDonnell KA, Burke JG, O’Campo P (2000) Women’s lives after an HIV-positive diagnosis: disclosure and violence. Matern Child Health J 4(2):111–120. doi:10.1023/A:1009522321240
Kiarie JN, Farquhar C, Richardson BA, Kabura BN, John FN, Nduati RW, John-Stewart GC (2006) Domestic violence and prevention of mother-to-child transmission of HIV-1. AIDS 20:1763–1769. doi:10.1097/01.aids.0000242823.51754.0c
Temmerman M, Ndinya-Achola J, Ambani J, Piot P (1995) The right not to know HIV-test results. Lancet 345:969–970. doi:10.1016/S0140-6736(95)90707-6
World Health Organization (WHO) (2003) Gender dimensions of HIV status disclosure to sexual partners: rates, barriers and outcomes: a review paper. World Health Organization, Geneva, Switzerland
Gaillard P, Melis R, Mwanyumba F, Claeys P, Muigai E, Mandaliya K et al (2002) Vulnerability of women in an African setting: lessons for mother-to-child HIV transmission prevention programmes. AIDS 16:937–939. doi:10.1097/00002030-200204120-00019
Yacouba N, Nicolas M, Valeraine L, Laurent M, Seydou Y, Issiaka S et al (2001) Sexual and reproductive life of women informed of their HIV seropositivity: a prospective cohort study in Burkina Faso. J Acquir Immune Defic Syndr 28:367–372
Kissinger PJ, Niccolai LM, Magnus M, Farley TA, Maher JE, Richardson-Alston G et al (2003) Partner notification for HIV and syphilis: effects on sexual behaviors and relationship stability. Sex Transm Dis 30:75–82. doi:10.1097/00007435-200301000-00015
Antelman G, Fawzi MCS, Kaaya S, Mbwambo J, Msamanga GI, Hunter DJ, Fawzi WW (2001) Predictors of HIV–1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS 15:1865–1874. doi:10.1097/00002030-200109280-00017
Maman S, Mbwambo JK, Hogan NM, Kilonzo GP, Campbell JC, Weiss E, Sweat MD (2002) HIV-positive women report more lifetime partner violence: findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. Am J Public Health 92:1331–1337. doi:10.2105/AJPH.92.8.1331
Multhal-Rathore A, Tripathi R, Arora R (2002) Domestic violence against pregnant women interviewed at a hospital in New Delhi. IJGO 76(1):83–85
Stewart DE, Cecutti A (1993) Physical abuse in pregnancy. Can Med Assoc J 149:1257–1263
Kiarie JN, Farquhur C, Richardson BA, Kabura MN, John FN, Nduati RW, John-Stewart GC (2006) Domestic violence and prevention of mother to child transmission of HIV-1. AIDS 20:1763–1769. doi:10.1097/01.aids.0000242823.51754.0c
Maman S, Mbwambo JK, Hogan NM, Kilonzo GP, Campbell JC, Weiss E, Sweat MD (2002) HIV positive women report more lifetime partner violence: findings from VCT clinic in Dar es Salaam, Tanzania. Am J Public Health 92:1331–1337. doi:10.2105/AJPH.92.8.1331
Dunkie KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD (2004) Gender based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet 363:1415–1421. doi:10.1016/S0140-6736(04)16098-4
Defeu I, Van Renterghem H, De Vuyst H, Fleerackers Y, Peters R, Colebunders R (1994) Consequences of telling one’s seropositivity to others. Abstract PD 224. Presented at International Conference on AIDS, Yokohama, Japan
Zierler S, Cunningham WE, Anderson R, Shapiro MF, Nakazono T, Morton S, Crystal S, Stein M, Turner B, St Clair P (2000) Bozzette. Violence victimization after HIV infection in a US probability sample of adult patients in primary care. Am J Public Health 90:208–215. doi:10.2105/AJPH.90.2.208
Olusanya O, Okpere E, Ezimokhai M (1985) The importance of social class in voluntary fertility control in a developing country. West Afr J Med 4:205–215
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ezechi, O.C., Gab-Okafor, C., Onwujekwe, D.I. et al. Intimate partner violence and correlates in pregnant HIV positive Nigerians. Arch Gynecol Obstet 280, 745–752 (2009). https://doi.org/10.1007/s00404-009-0956-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-0956-9