Abstract
Background
The association of vitiligo with psoriasis is inconsistent in the current literature.
Objective
To assess the bidirectional association between vitiligo and psoriasis.
Methods
A population-based study was performed to compare vitiligo patients (n = 20,851) with age-, sex- and ethnicity-matched control subjects (n = 102,475) regarding the incidence of new-onset and the prevalence of preexisting psoriasis. Adjusted hazard ratios (HRs) and adjusted odds ratios (ORs) were calculated by cox regression and logistic regression, respectively.
Results
The incidence rate of new-onset psoriasis was estimated at 7.9 (95% CI 6.4–9.7) and 4.7 (95% CI 4.1–5.3) cases per 10,000 person-years among patients with vitiligo and controls, respectively. Patients with vitiligo experienced an increased risk of psoriasis (fully-adjusted HR 1.71; 95% CI 1.35–2.17; P < 0.001). On the other hand, the odds of vitiligo were only marginally elevated among patients with preexisting psoriasis (fully-adjusted OR 1.19; 95% CI 1.01–1.40; P = 0.051). Compared to other patients with vitiligo, those with vitiligo and comorbid psoriasis were older at the onset of the disease and had a greater prevalence of metabolic and cardiovascular comorbidities.
Conclusions
A diagnosis of vitiligo predisposes individuals to develop subsequent psoriasis. Clinicians managing dermatologic patients ought to be aware of this comorbidity. Further research is required to explicate the pathomechanism underlying this epidemiological observation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitiligo is a chronic inflammatory autoimmune disorder characterized by the appearance of sharply demarcated depigmented patches due to the destruction of cutaneous melanocytes [1,2,3]. About 0.5–2% of the general population worldwide suffers from vitiligo. The disease can appear at any age, although about half of cases present before the age of 20 years [1,2,3]. Both sexes can be affected, while there are several reports of higher prevalence and early onset in women [1,2,3]. The pathogenesis of vitiligo is multifactorial with the involvement of genetic predisposition and environmental triggers leading to an autoimmune process with a T cell-mediated immune response that targets melanocytes. Multiple cell types, including keratinocytes, melanocytes, fibroblasts, stem cells, and different immune cells, are involved in pathogenetic pathways, with Th17 and Th1 playing a key role [1, 2, 4]. Vitiligo has been described in association with several autoimmune diseases such as thyroid disorders, diabetes mellitus, celiac disease, alopecia areata, and rheumatoid arthritis. The prevalence of autoimmune comorbidities varies between different studies [1, 2, 5].
Psoriasis is a chronic immune-mediated inflammatory dermatosis characterized by the appearance of erythematous plaques covered by silver scales as a result of increased proliferation and abnormal differentiation of keratinocytes [6,7,8]. The prevalence of psoriasis is estimated at 3% of the general population worldwide [6]. The disease affects both sexes equally and can appear at any age [6, 8]. The pathogenesis is multifactorial and involves genetic susceptibility, possible environmental triggers, and T cell-mediated immune response [6, 7]. Similar to vitiligo, pathogenesis involves the interaction between skin stromal cells and immune cells with a crucial role of Th1 and Th17 [6, 7, 9]. In addition to metabolic and cardiovascular comorbidities, there are multiple autoimmune disorders described in association with psoriasis, including rheumatoid arthritis, inflammatory bowel disease, type-1 diabetes mellitus, celiac disease, and Grave’s disease [6, 7, 10].
Vitiligo and psoriasis share several inflammatory pathways and genetic loci, which raise the possibility that the association between diseases is not accidental [4, 9, 11]. Currently, the data on the link between vitiligo and psoriasis are limited. Several case–control and cross-sectional studies were conducted in several countries and have shown inconsistent results [12,13,14,15,16,17,18,19,20,21,22]. Apart from the high heterogeneity across their results, these studies were hampered by some major methodological flaws [12,13,14,15,16,17,18,19,20,21,22]. Our study aimed to estimate the bidirectional association between vitiligo and psoriasis. That is, to estimate (i) the risk of new-onset psoriasis in patients with vitiligo and (ii) the odds of vitiligo among patients with preexisting psoriasis. The secondary endpoint was to delineate whether the subgroup of patients with vitiligo and comorbid psoriasis are typified by clinical and demographic variables distinguishing them from other patients with vitiligo.
Methods
Study design and dataset
Aiming at investigating the bidirectional association between vitiligo and psoriasis, the current population-based study encompassed two study designs. First, a retrospective cohort study design was applied to longitudinally follow patients with vitiligo and estimate the incidence of new-onset psoriasis. Second, a case–control study design was implemented to estimate the prevalence of preexisting psoriasis (exposure) in patients with subsequent vitiligo (outcome). Given the rare disease assumption, the latter design is likely to delineate the odds of vitiligo after psoriasis [23].
The computerized dataset of Clalit Health Services (CHS) is the source of the current study. Based on the National Health Insurance Law, all residents in Israel must subscribe to one of the four healthcare maintenance organizations, of whom CHS is the largest, covering 4,540,768 enrollees (~ 50.0% of the general Israeli population). CHS supplies a wide range of healthcare services that covers all tiers of the healthcare system (both outpatient and inpatient settings). Each contact with the health system is systematically documented in the medical files of patients. As this database continuously retrieves data from the medical files, it provides a comprehensive overview of CHS enrollees across time and serves as a reliable source for epidemiological data [24, 25].
Study population and definition of covariates
The CHS database was screened for incident cases with a diagnostic code of vitiligo between the years 2002 and 2019. Patients were considered eligible for inclusion if one of the following criteria was fulfilled: (i) a documented diagnosis of vitiligo as registered by a board-certified dermatologist, or (ii) a diagnosis of vitiligo in discharge letters from dermatological wards.
We enrolled a control group including up to five individuals without vitiligo per each case. Controls were matched based on age, sex, and ethnicity and were recruited on the day on which the corresponding case was diagnosed. The diagnosis of psoriasis was based on its documentation by a board-certified dermatologist or in discharge letters released from dermatological wards.
Outcome measures were adjusted for demographic variables and putative confounding comorbidities, including smoking, diabetes mellitus, hypertension, hyperlipidemia, and obesity. These comorbidities were found to predispose individuals to psoriasis [26] and were controlled to avoid confounding.
Statistical analysis
The comparison of variables between different comparator groups was performed using the chi-square test and t test for categorical and continuous variables, respectively. In the cohort study design, incidence rates of psoriasis were calculated for both vitiligo patients and controls and expressed as the number of events per 10,000 person-years. Hazard ratios (HR)s and 95% confidence intervals (CI)s for the risk of incident psoriasis were found by the use of the Cox regression model. Differences in the all-cause mortality of vitiligo patients with and without psoriasis were estimated using a stratified log-rank test.
In the case–control study design, logistic regression analysis was utilized to calculate odds ratios (ORs) and 95% CIs to compare cases and controls with regard to the presence of preexisting psoriasis. Based on the temporal relationship between exposure and outcome in case–control studies, only individuals who developed vitiligo after the diagnosis of psoriasis were included. Two-tailed P-values less than 0.05 were considered statistically significant. All statistical analyses were performed using SPSS software, version 25 (SPSS, Armonk, NY IBM Corp).
Results
Characteristics of the study population
A total of 123,326 participants were subject to inclusion in the current study. Of whom, 20,851 were patients with vitiligo and 102,475 were age-, sex, and ethnicity-matched controls. The mean (SD) age at the diagnosis of vitiligo was 34.7 (22.4) years, 10,570 (50.7%) were females, and 15,311 (73.4%) were Jews (Table 1). The baseline characteristics of the study population are outlined in Table 1.
The risk of psoriasis in patients with vitiligo
The findings of the retrospective cohort study design, estimating the risk of psoriasis among patients with vitiligo, are detailed in Table 2. The incidence rates of psoriasis were estimated at 7.9 (95% CI 6.4–9.7) and 4.7 (95% CI 4.1–5.3) cases per 10,000 person years among patients with vitiligo and controls, respectively.
Compared to their control subjects, the risk of psoriasis was significantly elevated in patients with vitiligo (HR 1.70; 95% CI 1.34–2.15; P < 0.001). In sex- and age-stratified analyses, the risk of psoriasis was more prominent among females (HR, 1.81; 95% CI 1.28–2.56; P = 0.001) and younger individuals (age < 32.4; HR, 1.93; 95% CI 1.28–2.91; P = 0.002). Vitiligo conferred a significantly increased risk of psoriasis in a multivariate analysis adjusting for demographics and comorbidities (fully-adjusted HR, 1.71; 95% CI 1.35–2.17; P < 0.001).
The odds of vitiligo among patients with a preexisting diagnosis of psoriasis
To investigate the odds of vitiligo following a history of psoriasis, a case–control study design was carried out (Table 3). The development of subsequent vitiligo was not significantly associated with a history of psoriasis (OR 1.15; 95% CI 0.97–1.36; P = 0.107). In an age- and sex-stratified analysis, psoriasis was found to predict vitiligo only among younger individuals (age < 32.4; OR 1.89; 95% CI 1.32–2.69; P < 0.001), whereas the association was insignificant among older individuals and both sexes (Table 3). In a multivariate logistic regression analysis adjusting demographic variables and comorbidities, the odds of vitiligo fell shortly out of significance after psoriasis (fully-adjusted OR 1.19; 95% CI 1.01–1.40; P = 0.051; Table 3).
Factors associated with comorbid psoriasis among patients with vitiligo
The last endpoint of the current study was to characterize vitiligo patients with comorbid psoriasis relative to the remaining patients with vitiligo (Table 4). The presence of psoriasis in patients with vitiligo was significantly associated with older age, Jewish ethnicity, obesity, ischemic heart disease, diabetes mellitus, hyperlipidemia, smoking, and hypertension (Table 4).
Survival analysis was then conducted to evaluate the risk of all-cause mortality in patients with vitiligo and comorbid psoriasis compared to the remaining patients with vitiligo. While comorbid psoriasis was associated with increased all-cause mortality in univariate analysis (HR 1.87; 95% CI 1.08–3.25; P = 0.026), this figure lost its statistical significance after adjusting for demographic variables and the following comorbidities: smoking, diabetes mellitus, hypertension, hyperlipidemia, and obesity (adjusted HR 1.28; 95% CI 0.74–2.23; P = 0.383; Supplementary Fig. 1).
Discussion
According to the current large-scale population-based study, patients with vitiligo are at a 1.7-fold increased risk of subsequent psoriasis. A history of preexisting psoriasis confers an elevated probability of developing vitiligo only among young individuals. Compared to patients with vitiligo alone, those with vitiligo and comorbid psoriasis were older, had a higher prevalence of cardiovascular comorbidities and comparable all-cause mortality rates.
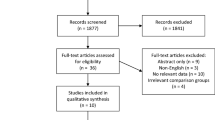
The coexistence of vitiligo and psoriasis in an individual patient was first reported by Seleyni in 1955 [27]. Subsequently, numerous case reports and a few cross-sectional and case–control studies were published. This epidemiological connection was studied bilaterally, with some studies investigating the risk of vitiligo among psoriatic patients and others evaluating the risk of psoriasis in patients with vitiligo [12]. This association was recently explored by a meta-analysis pooling data from seven study populations of psoriasis (n = 120,866) and four study populations of vitiligo (n = 79,907) [12]. This quantitative synthesis revealed elevated odds of comorbid psoriasis in vitiligo (OR 2.29; 95% CI 1.56–3.37) as well as of vitiligo in psoriasis (OR 3.43; 95% CI 1.86–6.33) [12]. While our findings accord with the latter in the increased risk of psoriasis in vitiligo, the inverse association fell shortly out of statistical significance. It is noteworthy that our study represents the first retrospective cohort study shedding light on this association. Owing to the longitudinal follow-up and maintaining the temporal sequence between exposure and outcome, this study design is superior to the previously utilized cross-sectional and case–control study designs with regard to identifying causality [28].
The mechanism underlying the association of vitiligo with psoriasis is yet to be precisely delineated. However, several hypotheses have been postulated. One of the putative explanations relates to the epitope spreading phenomenon, in which the primary immune-inflammatory process against vitiligo-related epitopes causes exposure to nearby hidden epidermal epitopes, leading to the production of an immune response against these antigens [29]. Second, a mechanistic role exerted by genetic predisposition cannot be excluded. A shred of evidence has accumulated to suggest that these conditions share common genetic loci such as HLA-C/HLA-B rs9468925 and AIS1 interval within PSOR7 on chromosome 1p31.3–p32.2 [11, 30]. A recent genome-wide association study identified several shared susceptibility genes, including (i) IFIH1 that participates in the innate immune response, (ii) BTNL2 that contributes to T-cell activation, and iii the risk locus on 6p21.3 [31].
Vitiligo and psoriasis share a common Th-1/Th-17 immune response pathway. The increase in the main pro-inflammatory cytokines produced by Th-1 cells (IFN-gamma, TNF-α, and IL-2) as well as cytokines secreted by Th-17 cells (IL-17 and IL-23) were observed in both conditions [32, 33]. In some patients, the psoriatic and vitiliginous lesions are localized in the same area concomitantly. In these cases, a Koebner phenomenon (isomorphic reaction) was suggested as a mechanism for the coexistence, when an injury to vitiliginous skin may induce an appearance of psoriatic lesions and vice versa [34].
The large sample size and the population-based nature of the study argue against the existence of selection bias. The reliance on a large-scale database that retrieves clinical data from all tiers of the healthcare system provides an insightful view of the epidemiological question of interest. The dependence on diagnostic codes registered merely by dermatologists substantiates the external validity of our study. Given that a computerized database was the origin of our findings, the clinical and morphological variables of the investigated dermatoses (like disease severity and clinical variants), were missing.
In conclusion, this large-scale population-based study revealed that patients with vitiligo are at a 1.7-fold increased chance of acquiring psoriasis. Relative to patients with vitiligo only, those with vitiligo and comorbid psoriasis are older, have a higher prevalence of smoking, metabolic and cardiovascular comorbidities, and a comparable risk of all-cause mortality. Our findings add to the understanding of the relationship between vitiligo and psoriasis. Further research is needed to expand our comprehension of the link between these disorders to reduce the impact of comorbidities, improve treatment efficacy, and, ultimately, improve patients’ quality of life.
References
Speeckaert R, van Geel N (2017) Vitiligo: an update on pathophysiology and treatment options. Am J Clin Dermatol 18:733–744
Rodrigues M, Ezzedine K, Hamzavi I, Pandya AG, Harris JE (2017) New discoveries in the pathogenesis and classification of vitiligo. J Am Acad Dermatol 77(1):1–13
Ezzedine K, Eleftheriadou V, Whitton M, Van Geel N (2015) Vitiligo. Lancet 386:74–84
Bassiouny DA, Shaker O (2011) Role of interleukin-17 in the pathogenesis of vitiligo. Clin Exp Dermatol 36:292–297
Dahir AM, Thomsen SF (2018) Comorbidities in vitiligo: comprehensive review. Int J Dermatol 57:1157–1164
Armstrong AW, Read C (2020) Pathophysiology, clinical presentation, and treatment of psoriasis: a review. J Am Med Assoc 323:1945–1960
Boehncke WH, Schön MP (2015) Psoriasis. Lancet 386:983–994
Michalek IM, Loring B, John SM (2017) A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol 31:205–212
Di Cesare A, Di Meglio P, Nestle FO (2009) The IL-23Th17 axis in the immunopathogenesis of psoriasis. J Invest Dermatol 129:1339–1350
Wu JJ, Nguyen TU, Poon KYT, Herrinton LJ (2012) The association of psoriasis with autoimmune diseases. J Am Acad Dermatol 67:924–930
Zhu KJ, Lv YM, Yin XY, Wang ZX, Sun LD, He SM et al (2011) Psoriasis regression analysis of MHC loci identifies shared genetic variants with vitiligo. PLoS ONE 6:e23089
Yen H, Chi CC (2019) Association between psoriasis and vitiligo: a systematic review and meta-analysis. Am J Clin Dermatol 20:31–40
Sharquie KE, Salman HA, Yaseen AK (2017) Psoriasis and vitiligo are close relatives. Clin Cosmet Investig Dermatol 10:341–345
Teulings HE, Ceylan E, Overkamp M, Vrijman C, Bos JD, Nijsten TE et al (2016) Nonsegmental vitiligo disease duration and female sex are associated with comorbidity and disease extent: a retrospective analysis in 1307 patients aged ≥ 50 years. Br J Dermatol 175:821–824
Arunachalam M, Dragoni F, Colucci R, Berti S, Crocetti E, Galeone M et al (2014) Non-segmental vitiligo and psoriasis comorbidity—a case–control study in italian patients. J Eur Acad Dermatol Venereol 28:433–437
Prignano F, Pescitelli L, Ricceri F, Lotti T (2008) The importance of genetical link in immuno-mediated dermatoses: psoriasis and vitiligo. Int J Dermatol 47:1060–1062
Sandhu K, Kaur I, Kumar B (2004) Psoriasis and vitiligo. J Am Acad Dermatol 51:149–150
Lee H, Lee MH, Lee DY, Kang HY, Kim KH, Choi GS et al (2015) Prevalence of vitiligo and associated comorbidities in korea. Yonsei Med J 56:719–725
Chen YT, Chen YJ, Hwang CY, Lin MW, Chen TJ, Chen CC et al (2015) Comorbidity profiles in association with vitiligo: a nationwide population-based study in taiwan. J Eur Acad Dermatol Venereol 29:1362–1369
Park JM, Kim HJ, Bae BG, Park YK (2009) A case of concurrent vitiligo and psoriasis. Ann Dermatol 21:330–333
Sawchuk M, Spano F, Loo WJ, Guenther L (2012) The coexistence of psoriasis and vitiligo: a review. J Cutan Med Surg 16:300–305
Canu D, Shourick J, Andreu N, Gey A, Ballanger-Désolneux F, Barailler H et al (2021) Demographic and clinical characteristics of patients with both psoriasis and vitiligo in a cohort of vitiligo patients: a cross-sectional study. J Eur Acad Dermatol Venereol. https://doi.org/10.1111/jdv.17383
Greenland S, Thomas DC (1982) On the need for the rare disease assumption in case-control studies. Am J Epidemiol 116:547–553
Kridin K, Ludwig RJ, Schonmann Y, Damiani G, Cohen AD (2020) The bidirectional association between bullous pemphigoid and psoriasis: a population-based cohort study. Front Med 7:511
Cohen AD, Dreiher J, Regev-Rosenberg S, Yakovson O, Lieberman N, Goldfracht M et al (2010) The quality indigators program in clalit health services: the first decade. Harefuah 149:204–209
Singh S, Young P, Armstrong AW (2017) An update on psoriasis and metabolic syndrome: a meta-analysis of observational studies. PLoS ONE 12:e0181039
Selenyi A (1955) Vitiligo and psoriasis on the same side with syringomyelia. Borgyogy Venerol Sz Hungr 9:94–96
Soh SE, Saw SM (2010) Cohort studies: design and pitfalls. Am J Ophthalmol 150:3–5
Chan LS, Vanderlugt CJ, Hashimoto T, Nishikawa T, Zone JJ, Black MM et al (1998) Epitope spreading: lessons from autoimmune skin diseases. J Invest Dermatol 110:103–109
Fain PR, Gowan K, LaBerge GS, Alkhateeb A, Stetler GL, Talbert J et al (2003) A genomewide screen for generalized vitiligo: confirmation of AIS1 on chromosome 1p31 and evidence for additional susceptibility loci. Am J Hum Genet 72:1560–1564
Shen C, Gao J, Sheng Y, Dou J, Zhou F, Zheng X et al (2016) Genetic susceptibility to vitiligo: GWAS approaches for identifying vitiligo susceptibility genes and loci. Front Genet. https://doi.org/10.3389/fgene.2016.00003
Das D, Akhtar S, Kurra S, Gupta S, Sharma A (2019) Emerging role of immune cell network in autoimmune skin disorders: an update on pemphigus, vitiligo and psoriasis. Cytokine Growth Factor Rev 45:35–44
Seneschal J, Boniface K, D’Arino A, Picardo M (2021) An update on vitiligo pathogenesis. Pigment Cell Melanoma Res 34:236–243
Ji Y-Z, Liu S-R (2019) Koebner phenomenon leading to the formation of new psoriatic lesions: evidences and mechanisms. Biosci Rep. https://doi.org/10.1042/BSR20193266
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ADC served as an advisor, investigator, or speaker for Abbvie, BI, Dexcel Pharma, Janssen, Novartis, Perrigo, Pfizer, and Rafa. None of the other authors have any conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

403_2022_2358_MOESM1_ESM.jpg
Supplementary Figure 1. Kaplan–Meier curves demonstrating all-cause mortality of vitiligo patients with psoriasis as compared to vitiligo patients without psoriasis.
Rights and permissions
About this article
Cite this article
Kridin, K., Lyakhovitsky, K., Onn, E. et al. Investigating the epidemiological relationship between vitiligo and psoriasis: a population-based study. Arch Dermatol Res 315, 395–400 (2023). https://doi.org/10.1007/s00403-022-02358-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-022-02358-8