Abstract
Toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS) are considered to be drug-induced diseases, and are characterized by extensive mucocutaneous disorder and epidermal necrosis which result in the detachment of the epidermis. Inactive and active forms of metalloproteinases (MMP2 and MMP9) secreted by skin explants maintained in organ culture for 72 h and in blister fluid from two TEN and three SJS patients were investigated. Interestingly, lesional skin from both the TEN and the SJS patients cultured for 3 days in conditioned medium showed high levels of both 72 kDa progelatinase A and 66 kDa activated gelatinase A, and the 66 kDa activated form was not observed in cultures of skin from control individuals. Furthermore, indirect immunodetection showed the presence of MMP2 and MMP9 in TEN and SJS patients’ skin. Increased gelatinase activity in the culture medium of TEN and SJS skin maintained in organ culture and in blister fluid indicates that these gelatinases may be responsible for the detachment of the epidermis in these drug-induced necrolyses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Toxic epidermal necrolysis (TEN) was first described by Lyell in 1956 who reported four patients with a “scalded skin” appearance. TEN, also known as Lyell’s syndrome, is characterized by extensive mucocutaneous disorder, particularly epidermal necrosis, which results in the detachment of the epidermis. This severe drug-induced disease, despite progress in intensive care, remains severe with a non-negligible mortality and constitutes a dermatological emergency. Stevens-Johnson syndrome (SJS) is also considered a drug-induced disease. It has been put forward that SJS and TEN are related mucocutaneous disorders, which can overlap [18]. There is no clear distinction between TEN and SJS because these two pathological states include a wide range of clinical presentations [1].
The term “acute disseminated epidermal necrosis” (ADEN) was presented during the International Symposium on Drug-Related Skin Reactions, which was held in Créteil in 1994. ADEN was defined as follows:
-
Group I (60% of patients). Includes those with SJS. Cutaneous detachment affects less than 10% of the body area.
-
Group II (30% of patients). Includes syndromes between TEN and SJS. Cutaneous detachment affects between 10% and 30% of the body area.
-
Group III (10% of patients). Includes those with TEN. Cutaneous detachment affects more than 30% of the body area.
Because histological investigations conducted on skin from patients suffering from TEN have revealed detachment of the entire epidermis, Paquet et al. [15] have suggested that the detachment of epidermal basal cells is caused by proteolytic processes mainly involving metalloproteinases. Keratinocytes which synthesize the macromolecular components of the dermoepidermal basement membrane have also been shown to express metalloproteinases such as gelatinase A (MMP2) and gelatinase B (MMP9) which are able to degrade macromolecular components of the basement membrane.
These enzymes are secreted in the form of latent zymogens that need to be activated in the extracellular compartment or in the vicinity of the cell membrane by other MMPs or serine proteinases [11]. So we decided to investigate inactive and active forms of metalloproteinases (MMP2 and MMP9) secreted by skin explants maintained in organ culture for 72 h and in blister fluid from two TEN and three SJS patients, to ascertain whether we could draw a parallel between MMPs (active and inactive forms) secreted in organ culture medium and blister fluid. We also compared the results obtained with skin explants from TEN and SJS patients with those obtained from two healthy control volunteers. Furthermore, by indirect immunodetection we sought evidence for the presence of MMP2 and MMP9 in skin from TEN and SJS patients and the results were compared with those obtained from the skin of two healthy subjects.
Materials and methods
Blister fluid collection
The fluid from intact blisters was collected and kept frozen at –80°C until used.
Skin biopsies
Skin biopsies were taken from the edge of blisters of two patients suffering from TEN (one male and one female aged 57 and 76 years, respectively), from three patients suffering from SJS (two males and one female aged 33, 39 and 55 years, respectively), and from two healthy control volunteers (one male and one female aged 25 and 26 years, respectively). After obtaining the subjects’ consent, the biopsies were obtained under local lidocaine anaesthesia. The biopsies were cut into two parts, one for organ culture and the other for histology and immunostaining.
Biochemical studies
Organ culture
Skin biopsies cut into small pieces were maintained for up to 3 days in Dulbecco’s modified Eagle’s medium (DMEM) containing 1.5 mmol/l Ca2+, supplemented with 0.2% lactate hydrolysate (Sigma, St Louis, Mo.), 2 mmol/l l-glutamine,100 U/ml penicillin and 100 μg/ml streptomycin (Boehringer, Mannheim, Germany) at 37°C in an atmosphere of 95% air and 5% CO2. Cell viability was evaluated in terms of lactate dehydrogenase activity in conditioned medium.
Enzyme assays
The presence of MMP2 and MMP9 in organ culture medium and in blister fluid was checked by zymography using 0.1% sodium dodecyl sulphate (SDS) polyacrylamide gels impregnated with 1 mg/ml type I gelatin [2]. Gelatinolytic activities appeared on the zymogram as unstained lysis bands. Protein standards were subjected to a parallel electrophoresis to determine the molecular weight of the lysis bands. To assign these bands to a proteinase class, the following reagents (all obtained from Sigma) were added to the incubation buffer: EDTA (15 mmol/l) or 1,10-phenanthroline (15 mmol/l) for metalloproteinases, phenylmethyl sulphonyl fluoride (PMSF, 2 mmol/l) or Pefablock (2 mmol/l) for serine proteinases, and N-ethylmaleimide (2 mmol/l) for cysteine proteinases.
MMP2 and MMP9 were identified immunologically in culture conditioned medium by Western blotting using monoclonal antibodies directed against these enzymes (Valbiotech, France).
Quantification of gelatinolytic activities
The average surface area of the lysis bands on the zymograms was determined semiautomatically following their contour with a calibrated electronic slide. They were then viewed with a video camera and black and white images were converted into 256 different grey levels using a Sophretec MVM 600 image memory, transferred to a BFM microcomputer and analysed using mathematical morphology software [24]. Gelatinase activities detected on zymograms were derived from the expression surface area of the lysis band in pixels × grey level in arbitrary units per milligram of tissue.
Morphology and immunostaining
Skin biopsies were fixed in paraformaldehyde before being embedded in paraffin by routine procedures. Serial tissue sections, 5 μm thick, were stained with haematoxylin-eosin to visualize the tissue quality.
For immunostaining, primary monoclonal antibodies directed against human MMP2 and MMP9 both from Calbiochem (La Jolla, Calif.) were used, and the avidin-biotin method was applied with appropriate secondary antibodies. Nonspecific reactivity of the antibodies was checked by omitting the primary antibody; we also checked the nonspecific reactivity of the antibodies by using irrelevant secondary antibodies.
ELISA
MMP2 and tissue inhibitor of MMP2 (TIMP2) levels were determined in the blister fluid and after 48 h in the culture medium of organ cultures of biopsies from patients suffering from TEN and SJS. MMP2 and TIMP2 protein levels were determined using an ELISA kit (R&D Systems, Minneapolis, Minn.). All samples and standards were assayed twice. The results are reported as nanograms of cytokine per millilitre of blister fluid.
Results
Qualitative and quantitative analysis of gelatinases secreted from skin explants
Gelatinolytic activities were determined by gelatin zymography and further quantified by image analysis as a function of time of culture. The amount of enzymes increased in a quasilinear manner during the first 72 h of culture then reached a plateau phase. For this reason the data reported are those obtained after 72 h of organ culture. For all species the activities were proportional to the amount of conditioned medium (0.5–5 μl) deposited onto the gel (not shown).
Following 72 h of culture, skin explants from the two healthy donors showed gelatinolytic activity, which appeared as faint bands at 92 kDa (progelatinase B) and 72 kDa (progelatinase A; Fig. 1, lanes f, g). The intensity of these bands was much greater on the zymograms of the culture conditioned medium of the explants from the three SJS patients (Fig. 1, lanes b, c, d). On the zymograms of the conditioned medium of the explants from the five patients, three SJS and two TEN, a gelatinolytic band was present with an apparent molecular mass of 66 kDa corresponding to the activated form of MMP2 (Fig. 1, lanes a–e), and on the zymogram for SJS patient no. 1 a gelatinolytic band was present with an apparent molecular mass of 88 kDa corresponding to the activated form of gelatinase B (MMP9). All activities were suppressed by supplementing the incubation buffer with EDTA (15 mmol/l) but remained unaffected by Pefablock (not shown).
Gelatin zymography following 72 h of incubation in organ culture medium of skin biopsies from TEN and SJS patients and two control subjects. Lane a TEN patient 1, lane b SJS patient 1, lane c SJS patient 2, lane d SJS patient 3, lane e TEN patient 2, lane f control 1, lane g control 2; 72 kDa progelatinase A (proMMP2), 66 kDa activated gelatinase A (MMP2), 92 kDa progelatinase B (proMMP9), 88 kDa activated gelatinase B (MMP9)
The metalloproteinase secreted (progelatinase B, 92 kDa; activated gelatinase B, 88 kDa; progelatinase A, 72 kDa; activated gelatinase A, 66 kDa) were demonstrated by gelatin zymography and were confirmed by Western blotting (not shown).
Levels of gelatinase normalized to tissue weight were quantified in the conditioned medium from all skin explants after 72 h of culture. The distributions in percentage of the latent and activated forms of MMP9 and MMP2 were evaluated (not shown). The main difference between control skin and pathological skin from the two TEN and the three SJS patients concerned MMP2 which appeared as the latent (72 kDa) and activated forms (66 kDa) in the skin from the five patients while in control skin only a zymogen form of MMP2 (72 kDa) was seen (Fig. 2). Furthermore, activated MMP9 (88 kDa) was observed in the skin of only one SJS patient and not in the skin of the other patients (see Fig. 1).
Quantification of gelatinolytic activity of latent proMMP2 and activated MMP2 expressed in skin biopsies from two TEN patients and three SJS patients and from two controls in conditioned medium of organ cultures following 72 h of incubation. The gelatinolytic activity was derived from the expression surface area of the lysis band in pixels × grey level in arbitrary units/mg of tissue weight
Qualitative analysis of gelatinases secreted in blister fluid
Gelatinolytic activities identified by gelatin zymography appeared as unstained bands on the zymograms. In the lesional skin with blisters of the one TEN and two SJS patients, gelatinolytic activities migrating with an apparent molecular mass at 92 kDa (progelatinase B), at 72 kDa (progelatinase A), and at 66 kDa (activated gelatinase A) were observed (Fig. 3). Due to the presence on the gelatin zymograms of proteins stained by Coomassie blue with an apparent molecular masses between 72 and 66 kDa interfering with the lysis bands at 72 kDa and 66 kDa, no quantitative analysis was possible (Fig. 3).
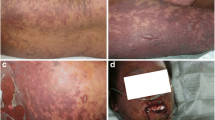
Histology and immunohistology
The skin biopsies of the healthy subjects appeared histologically normal without an inflammatory infiltrate. The biopsies from the TEN patients showed epidermal detachment with a slight inflammatory infiltrate. The skin from the two healthy subjects showed very faint labelling for MMP2 and MMP9 in the dermis and epidermis by indirect immunodetection. The epidermis of the two TEN and three SJS patients was positive for MMP2 and MMP9 with a more intense labelling located at the level of the detached epidermis, and the dermal extracellular matrix of these five patients showed a very faint positivity for MMP2 as well as for MMP9, and the intensity of this labelling was comparable to that observed in the dermis of the two healthy subjects (see Fig. 4).
ELISA
In organ culture (Fig. 5), the amounts of MMP2 were estimated at 33.81, 14.64, 98.5, 198.2, 34.58, 336.65 and 153,15 ng/ml, and the amounts of TIMP2 at 36.76, 8.4, 36.86, 17.43, 17.68, 6.46 and 47.98 ng/ml for control 1, control 2, TEN patient 1, SJS patient 1, SJS patient 2, SJS patient 3 and TEN patient 2, respectively.
In blister fluids (Fig. 6), the amounts of MMP2 were estimated at 2645.77, 1876.7 and 2062.26 ng/ml, and the amounts of TIMP2 at 423.2, 287.33 and 434.77 ng/ml for TEN patient 1, SJS patient 3 and TEN patient 2, respectively.
Discussion
TEN represents 1% of all drug-related skin reactions requiring hospitalization. Epidemiological studies have shown an identical rate of 1 to 1.3 new cases per million of population annually [20, 22, 27]. Clinically, lesions are heralded by a brief prodromal phase with symptoms strongly resembling those of influenza. It is followed by an eruptive phase occurring between 12 and 14 days after drug administration, shorter in the exceptional cases of recurrence. Some patients show haematological disorders with variable frequencies [4, 17, 19]. The drugs most frequently involved are sulphonamides, anticonvulsants, allopurinol, phenylbutazone derivatives and, less frequently, other NSAIDs. Most of the visceral manifestations observed in TEN are identical to those seen in extensive burns. Without any emergency treatment the disease can be fatal within 2 to 3 days. The disease responds favourably to rapid and appropriate management, with reepithelialization of most of the skin within 2 to 3 weeks.
In this work we demonstrated by indirect immunodetection, using monoclonal antibodies directed against MMP2 and MMP9, positivity for these two metalloproteinases in the epidermis of patients suffering from TEN (two patients) and SJS (three patients) compared to the skin of two healthy donors.
The cellular sources of gelatinases A and B are multiple. Gelatinase A (also named type IV collagenase or MMP2) is produced by dermal fibroblasts [23], keratinocytes [9], Langerhans cells [16], lymphocytes T [28], macrophages [6] and neutrophils [5]. None of these cellular sources can be excluded except neutrophils, which have been shown to be absent in TEN lesions [15].
Gelatinase B (also referred to as 92 kDa type IV collagenase or MMP9) was originally classified as a macrophage collagenase. MMP9 appears to be expressed by a variety of cell types such as keratinocytes [8] and fibroblasts [10]. During TEN and SJS syndromes the overexpression of MMPs by keratinocytes via a particular mechanism cannot be excluded. For example, contact between inflammatory cells and keratinocytes could lead to mutual stimulation. Precise localization of MMP2 and MMP9 by in situ hybridization, for example, could provide important extra information to identify the different cell types involved in such gelatinase expression.
By zymography we demonstrated that MMP2 and MMP9 were liberated in the organ culture of control and pathological skin. This suggests skin necrosis. But as mentioned in Materials and Methods, the culture medium contained 1.5 mmol/l Ca2+. It has been demonstrated by Variani [25] that tissue degeneration is preserved in organ culture when the Ca2+ concentrations are at least 1.4 mmol/l. Under these conditions the cultured skin is maintained in a histologically and biochemically active state for 12–20 days without degeneration. Furthermore, lactate dehydrogenase was not detected in our organ culture medium following 5 days of culture.
Interestingly, all conditioned culture media after 3 days of culture of lesional skin from the two TEN and three SJS exhibited high levels of both 72 kDa progelatinase A and 66 kDa activated gelatinase A, and the 66 kDa activated form was not observed in cultures of control skin. We showed that active MMP2 was present in the blister fluid of patients suffering from TEN, in accordance with previously reported results [12, 15] and in patients with burn wounds [29].
As well as gelatin zymography showing the presence of the active MMP2 in blister fluid and in organ culture medium, large amounts of MMP2 compared to TIMP2 were also shown by ELISA. Increased activation of gelatinase A may be caused by increased membrane type I MMP (MT1-MMP) expression or downregulation of TIMP2, or both [3]. ELISA showed unchanged secretion of TIMP2 in skin of SJS and TEN patients compare to secretion in control skin, while secretion of MMP2 was considerably increased, and these findings are in favour of an altered balance of MMP2 and TIMP2 in SJS and TEN patients. Gelatinase A in its activated form, and also activated MMP9, could jointly act in epidermal detachment observed during SJS and TEN. The role of MMPs has to be correlated with the main pathogenic mechanism in TEN which involve FAS-FASL keratinocyte apoptosis [26].
Another interesting point concerns cytokines. It has been reported that TNFα is involved in the pathogenesis of TEN [13, 14]. The presence of MMP2 and MMP9 has been shown to favour the liberation of the active cytokine by proteolytic processes from the membrane-anchor precursor [7]. TGFβ, which has been shown to upregulate type IV collagenase expression by human keratinocytes in culture [21], could be involved in such a pathological process.
In conclusion, increased gelatinase activity in the culture medium of skin from TEN and SJS patients maintained in organ culture and in blister fluid may be responsible for the detachment of the epidermis in these drug-induced necrolyses. Further experiments are needed to establish and investigate the correlation if any between cytokines and gelatinases, and also between collagenases and extracellular matrix degradation products which result in epidermal necrolyses.
References
Bastuji-Garin S, Rzany B, Stern RS, et al (1993) Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol 129:92–96
Beranger JY, Godeau G, Frances C, Robert L, Hornebeck W (1994) Presence of gelatinase A and metalloelastase type protease at the plasma membrane of human skin fibroblasts. Influence of cytokines and growth factors on cell-associated metalloendopeptidase levels. Cell Biol Int 18:715–722
Birkedal-Hansen H (1995) Proteolytic remodeling of extracellular matrix. Curr Opin Cell Biol 7:728–735
Bombal C, Roujeau JC, Kuentz M, Revuz J, Touraine R (1983) Hematologic anomalies in Lyell’s syndrome. Study of 26 cases. Ann Dermatol Venereol 110:113–119
Cuello C, Wakefield D, Di Girolamo N (2002) Neutrophil accumulation correlates with type IV collagenase/gelatinase activity in endotoxin induced uveitis. Br J Ophthalmol 86:290–295
Finlay GA, O’Driscoll LR, Russell KJ, et al (1997) Matrix metalloproteinase expression and production by alveolar macrophages in emphysema. Am J Respir Crit Care Med 156:240–247
Gearing AJ, Beckett P, Christodoulou M, et al (1994) Processing of tumour necrosis factor-alpha precursor by metalloproteinases. Nature 370:555–557
Katz AB, Taichman LB (1999) A partial catalog of proteins secreted by epidermal keratinocytes in culture. J Invest Dermatol 112:818–821
Kobayashi T, Hattori S, Nagai Y, Tajima S, Nishikawa T (1998) Differential regulation of MMP-2 and MMP-9 gelatinases in cultured human keratinocytes. Dermatology 197:1–5
Munaut C, Noel A, Weidle UH, Krell HW, Foidart JM (1995) Modulation of the expression of interstitial and type-IV collagenases in coculture of HT1080 fibrosarcoma cells and fibroblasts. Invasion Metastasis 15:169–178
Nagase H (1997) Activation mechanisms of matrix metalloproteinases. Biol Chem 378:151–160
Oikarinen A, Kylmaniemi M, Autio-Harmainen H, Autio P, Salo T (1993) Demonstration of 72-kDa and 92-kDa forms of type IV collagenase in human skin: variable expression in various blistering diseases, induction during re-epithelialization, and decrease by topical glucocorticoids. J Invest Dermatol 101:205–210
Paquet P, Pierard GE (1997) Erythema multiforme and toxic epidermal necrolysis: a comparative study. Am J Dermatopathol 19:127–132
Paquet P, Nikkels A, Arrese JE, Vanderkelen A, Pierard GE (1994) Macrophages and tumor necrosis factor alpha in toxic epidermal necrolysis. Arch Dermatol 130:605–608
Paquet P, Nusgens BV, Pierard GE, et al (1998) Gelatinases in drug-induced toxic epidermal necrolysis. Eur J Clin Invest 28:528–532
Ratzinger G, Stoitzner P, Ebner S, et al (2002) Matrix metalloproteinases 9 and 2 are necessary for the migration of Langerhans cells and dermal dendritic cells from human and murine skin. J Immunol 168:4361–4371
Revuz J, Penso D, Roujeau JC, et al (1987) Toxic epidermal necrolysis. Clinical findings and prognosis factors in 87 patients. Arch Dermatol 123:1160–1165
Roujeau JC (1997) Stevens-Johnson syndrome and toxic epidermal necrosis are severity variants of the same disease which differs from erythema multiforme. J Dermatol 24:726–729
Roujeau JC, Moritz S, Guillaume JC, et al (1985) Lymphopenia and abnormal balance of T-lymphocyte subpopulations in toxic epidermal necrolysis. Arch Dermatol Res 277:24–27
Roujeau JC, Guillaume JC, Fabre JP, Penso D, Flechet ML, Girre JP (1990) Toxic epidermal necrolysis (Lyell syndrome). Incidence and drug etiology in France, 1981–1985. Arch Dermatol 126:37–42
Salo T, Lyons JG, Rahemtulla F, Birkedal-Hansen H, Larjava H (1991) Transforming growth factor-beta 1 up-regulates type IV collagenase expression in cultured human keratinocytes. J Biol Chem 266:11436–11441
Schopf E, Stuhmer A, Rzany B, Victor N, Zentgraf R, Kapp JF (1991) Toxic epidermal necrolysis and Stevens-Johnson syndrome. An epidemiologic study from West Germany. Arch Dermatol 127:839–842
Senior RM, Griffin GL, Fliszar CJ, Shapiro SD, Goldberg GI, Welgus HG (1991) Human 92- and 72-kilodalton type IV collagenases are elastases. J Biol Chem 266:7870–7875
Serra J (1987) Morphological optics. J Microsc 145 (Pt 1):1–22
Varani J (1998) Preservation of human skin structure and function in organ culture (review). Histol Histopathol 13:775–783
Viard I, Wehrli P, Bullani R, et al (1998) Inhibition of toxic epidermal necrolysis by blockade of CD95 with human intravenous immunoglobulin. Science 282:490–493
Villada G, Roujeau JC, Cordonnier C, et al (1990) Toxic epidermal necrolysis after bone marrow transplantation: study of nine cases. J Am Acad Dermatol 23(5 Pt 1):870–875
Weeks BS, Schnaper HW, Handy M, Holloway E, Kleinman HK (1993) Human T lymphocytes synthesize the 92 kDa type IV collagenase (gelatinase B). J Cell Physiol 157:644–649
Young PK, Grinnell F (1994) Metalloproteinase activation cascade after burn injury: a longitudinal analysis of the human wound environment. J Invest Dermatol 103:660–664
Acknowledgements
We would like to thank Prof. Roujeau for his generous gift of skin biopsies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gaultier, F., Ejeil, AL., Igondjo-Tchen, S. et al. Possible involvement of gelatinase A (MMP2) and gelatinase B (MMP9) in toxic epidermal necrolysis or Stevens-Johnson syndrome. Arch Dermatol Res 296, 220–225 (2004). https://doi.org/10.1007/s00403-004-0506-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-004-0506-z