Abstract
Introduction
The aim of this study was to examine if robotic-assisted total knee arthroplasty (RATKA) is cost- and time-effective in terms of implant stock and perioperative parameters, as optimizing perioperative efficiency may contribute to value-based care.
Materials and methods
Four hundred thirty-two consecutive patients who received primary total knee arthroplasties (TKAs) from May 2017 to March 2020 in a regional hospital were included in this study. Operating room time (OR time), surgical time, number of trays, insert thickness, and length of stay (LOS) were assessed and compared for a cohort group with navigation-assisted procedures to a group with robotic-assisted procedures (MAKO, Stryker, USA). Prediction of implant size was assessed for the robotic-assisted group. The Mann–Whitney U test was used for comparisons between groups when the normality assumption was not met. Categorical variables were assessed using the Fisher’s exact test. p < 0.05 was considered statistically significant.
Results
In the RATKA group, we noticed a significant mean reduction of 11 min in total OR time (p < 0.001), the use of thinner insert (p < 0.001), and a shorter mean length of stay of 1 day (p < 0.001). Compared to the navigation group, surgical time was not significantly longer, nor clinically relevant (0.238). In 76.9% of the robotic-assisted cases, the estimated implant size was equal to the final size and in all other cases, the preoperative implant size was oversized.
Conclusion
The introduction of the MAKO robotic-assisted total knee arthroplasty resulted in a gain in operating room time, a thinner and more predictable insert thickness, a shorter length of stay in hospital, and less instrumentation compared to navigation-assisted procedures.
Level of evidence
Level III, Retrospective cohort study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Robotic-assisted surgery for joint arthroplasties is evolving rapidly during the past decades [1, 2]. Nowadays, for total knee replacements, robotic-assisted total knee arthroplasty (RATKA) is claiming better clinical outcomes [3,4,5,6]. However, nor efficiency of the RATKA procedure, nor associated costs, have been studied thoroughly. Higher costs for purchase, maintenance, and robotic-specific disposables are offset by cost savings primarily driven by reduced instrumentation, reduced opioids use, shorter length of stay, and reduced post discharge resource utilization [7, 8]. Cost-effectiveness could also be accredited to better implant survivorship for RATKA. Although longer term studies are required to determine if improved implant positioning, resulting in a better balanced knee, genuinely leads to lower revision rates [9].
Learning curve studies illustrate that an orthopedic surgeon necessitates several months to master the technology of RATKA and that it could become even more time-effective than conventional techniques [10, 11]. A learning curve effect would be present in the first seven cases for integration in the surgical workflow [12].
The MAKO robotic-assisted total knee arthroplasty (Stryker, USA) was introduced in our hospital in April 23rd 2018. Meanwhile RATKA is a commonly performed procedure in our hand and we gained considerable experience passing the learning curve effect. We postulate that optimizing perioperative efficiency, which seems to improve, may contribute to value-based care. Furthermore, we consider this technique cost-effective in terms of implant stock and instrumentation based on predictability for implant size and insert thickness by planning preoperatively and adjusting implants peroperatively.
Accordingly, the purpose of our study was to examine the efficiency of MAKO robotic-assisted total knee arthroplasty in our hospital, compared to the earlier technique of navigation-assisted procedures. The primary outcome parameter was operating room (OR) time, secondary outcome parameters were surgical time, number of trays used, insert thickness, size prediction, and length of stay (LOS). Our hypothesis was that RATKA will be both more time- and cost-effective compared to navigation-assisted procedures.
Materials and methods
Four hundred thirty-two consecutive patients (one hundred ninety-eight navigation-assisted, two hundred thirty-four robotic-assisted) were retrospectively enrolled in our study. The navigation-assisted procedures were performed from May 2017 to April 2018 and the robotic-assisted procedures from April 2018 to March 2020. Patients were included if they had symptomatic knee osteoarthritis undergoing primary TKA. Exclusion criteria were previous knee surgery with implants in or around the joint. The first 15 patients of the robotic-assisted group were excluded to bypass the learning curve effect [12]. The arthroplasties were accomplished by one experienced surgeon (GL), who was familiar with both navigation- and robotic-assisted TKAs. The patients were not randomized to a procedure, but rather assigned sequentially, as the used technique in time in our hospital was first navigation and presently RATKA. The study was approved by the institutional review board (IRB) prior to research.
In the RATKA group, draping the robotic arm and setting up of the robot were carried out initially. Also different for this group was that the MAKO product specialist was always present before the start up. Furthermore, all the equipment was opened before the patient entered the operating room for both the robotic- and navigation-assisted groups. The knee was installed in the preparation room before entering the operating room. Once the patient has entered the room, the only things that had to be done before incision were the anesthesia, disinfection, and draping of the patient.
The surgical procedure was in all cases performed without tourniquet, using a subvastus approach. All patients received the cemented Triathlon (Stryker, USA) prosthesis, including a resurfacing of the patella. During surgery, it was the preference of the surgeon to preserve as much bone stock as possible and to aim for the thinnest possible insert thickness. The preoperative protocol was the same for both patient groups, with the exception that all patients of the RATKA group underwent a CT scan of the knee according to the MAKO protocol. The navigation system that was used was OrthoMap (Stryker, USA).
The postoperative care and revalidation protocol was the same for both groups: no drain was left, immediate mobilization, crutches if necessary, continuous passive motion (CPM), low-molecular-weight heparins (LMWH) for 10 days.
All patients were assessed for: OR time (defined as opening of the first set until exit of the OR), surgical time (first skin incision to wound closure), number of trays, insert thickness, and length of stay (LOS). Additionally, in the RATKA group, there was an assessment of the planned versus the definitive implant size. The criteria to discharge patients were again the same for both groups: no wound drainage, medical fitness, no social constraint, range of motion and autonomous transfers.
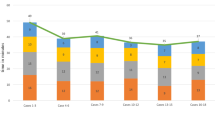
The statistical analysis was performed with the use of SPSS (IBM SPSS Statistics, Chigaco, USA). Continuous data are presented as mean and standard deviation (SD). Between-group comparisons were performed using the Mann–Whitney U test as the variables did not meet the normality assumption (Figs. 1 and 2). Categorical variables were assessed using the Fisher’s exact test. p < 0.05 was considered statistically significant.
Results
There was no statistically significant difference in population characteristics between patients undergoing TKA with navigation and those with MAKO (Table 1).
Those in the RATKA group had a 11-min shorter OR time (p < 0.001). Surgical time was not significantly different (p < 0.238). There was a significant difference in insert thickness (p < 0.001), which was 11.3 ± 0.1 mm for the navigation group and 10.0 ± 1.0 for the MAKO group. The mean LOS for MAKO was 3.8 ± 0.1 days, which was 1.3 days shorter than the navigation group (5.1 ± 0.2 days, p < 0.001; Table 2). Less instrumentation was needed for the robotic-assisted procedure compared to the navigation group, there was a reduction of three trays (respectively, seven and ten trays; Table 2).
In only 130 of the 234 robotic-assisted procedures, the estimated implant size was noted. Unfortunately for the other 104 patients, there was no preoperative screen capture available from which the planned implant size could be read. The final reported femoral and tibial implant size was equal to the planned implant size in 100 (76.9%) cases. There was a planning mismatch in 30 (23.1%) cases. In 6.9% of those cases, the planned tibial tray was oversized with one size. In 10% of the cases, the femoral component had been oversized with one size and in 5.4%, there was an oversizing of both components. There was no undersizing reported. In one case (0.8%), there was an oversizing of two sizes on the tibia (Table 3).
Discussion
The most important findings of this retrospective study, comparing navigation- with robotic-assisted surgery, were a significant shorter OR time, a thinner insert thickness, and a shorter mean length of stay for the RATKA group. Less instrumentation was needed compared to the navigation group. The surgical time was not statistically different.
A shorter OR time can be explained by the less pronounced variability in time for difficult knees, besides the smoothness of the surgical preparation for the robotic-assisted procedures. For the RATKA procedures, the surgeon disposes of a tool that accurately executes bone cuts according to the presurgical planning, as well as intraoperative feedback for restoring knee kinematics and soft tissue balance. Consequently, there are no “difficult knees” anymore and the surgeon does not lose time, as there is an interpretation of the problem based on the surgical planning preoperatively and recuts are hardly ever necessary. A study of Deckey et al. showed a significant reduction of recuts in RATKA compared to conventional procedures [13]. A feasibility study of unicompartmental procedures showed that MAKO-assisted procedures could overcome technical challenges [4]. A learning curve study, comparing MAKO RATKA with manual procedures, demonstrated significant lower OR times after 1 year and similar times after 6 months. The same study showed that mean surgical time continued to decrease after 6 months [11]. Accessory, a study of Mulier et al. showed that the use of a preparation room as in our study could shorten the non-operative time [14]. Although the installation protocol was similar for the navigation-assisted procedures and even there is no robot that must be draped and calibrated, we observed a smoother installation protocol for the RATKA procedures by the presence of the MAKO product specialist who is attuned on the surgeon and nurse team. In the navigation group, the product specialist is also present in the room, but he is less involved with the installation.
The reduction of insert thickness and less variability in used inserts is a repercussion of the predictability by preoperative planning and peroperative adjustment of the gapsize. The predictability of insert sizes influences implant stock, as the imperative presence of multiple, bigger insert sizes could be reduced using the robot. Furthermore, also implant size of femur and tibia component was known preoperatively, so standard implant stock in the hospital could be reduced as well and eventually be supplied the day before surgery by consulting the programmed cases for the next day. In 77% of the cases in our study, the femoral and tibial implant size was equal to the planned implant size. 26% of the implants were oversized on the preoperative plan, but this was a concern of surgical preference, as the MAKO robot only resects the slice of the tibia that is required for that specific size of prosthesis. In some cases, this leads to a remaining peripheral rim of bone, which makes it difficult to remove the resected tibial slice. By oversizing the tibial component by one size, this issue was solved. A recent study demonstrated a high accuracy in achieving preoperatively planned bone resection [15]. Similar results of implant prediction were found in a study of Marchand et al., with definitive implants within one size of the planned size in 100% of the cases and an exact match for 80% [16].
Surprisingly, there was a mean reduced LOS of 1.3 days (-25%), despite an identical fast-track revalidation, pain management, and discharge criteria. This could possibly be contributed to the reduced pain experience because of better soft tissue handling or the perception of better stability, due to better implantation accuracy. A recent systematic review and meta-analysis mentioned improved implantation accuracy and patient-reported outcomes for RATKA. However, a difference in soft tissue healing could not be demonstrated compared to the conventional TKA procedure [17]. Archer et al. found a reduced LOS for RATKA compared to the conventional technique [18]. However, a study of Tompkins et al. found that there was no significant difference in LOS and complications for RATKA compared to the manual technique [19]. It must be noted that in the last years, the overall trend for all TKA techniques, even the manual technique, is the fast-track revalidation. This could have influenced the length of stay of the navigation-assisted compared to the robotic-assisted procedures, as there was a sequential selection of patients in time. However, the overall postoperative protocol had not changed in these years in our center.
There was a reduction of three instrument trays compared to navigation-assisted TKAs. This reduction in number of trays is cost-effective, because of the reduced inventory and costs for sterilization. Nevertheless, the financial benefits must be weighed carefully against the additional costs associated with MAKO total knee robotic-assisted surgery, such as the purchase, maintenance, robotic-specific disposables, and preoperative CT. The cost for the preoperative CT is negligible [20]. Especially, by lowering the operating time, you save costs for the personnel and OR time. A recent systematic review estimated a cost of 0.55$ for 1 min in the operation room [21]. In our study, surgical time was not significantly different for the robotic-assisted group. Accessory, our center was the pioneer in Belgium for MAKO TKA procedures. This resulted in a lot of interest of visitors during the first years of the RATKA, which probably also influenced the surgical time in a negative way.
Although cost savings resulting from operative time, tray, stock and hospital stay reduction were not quantified in this study, other studies indicated substantial relevance of reduced instrumentation, shorter LOS and secondary reduced prescribed opioids and post-discharge resource utilization compared to manual TKA procedures [8]. However, Christopher et al. mentioned higher hospital costs, despite a lower LOS, but longer OR time, higher instruments and personnel costs [22]. We believe that cost-effectiveness should be considered at more long-term follow-up, as a better survival rate could have a major impact on total health cost for this population of patients and should also be considered. Maritan et al. revealed in a retrospective study with 5-year follow-up that conventional lateral UKAs and robotic-assisted had similar clinical outcomes and revision rates [23]. Overall, there is a lower average 90-day episode-of-care costs and superior quality for RATKA compared to the conventional technique [8, 24, 25]. The assumption that reduced OR time is cost-effective relies on the assumption that extra time is gained for performing additional minor surgeries, which has yet to be proven. Further research comparing cost-effectiveness for robotic-assisted procedures could clarify that this matter and long-term data are essential to fully ascertain its cost-effectiveness.
Limitations of this study are its retrospective, non-randomized design, the sequential group allocation, and the comparison of cohorts in different years. Another limitation is the lack of data from the planned implant size and missing data for preoperative alignment for both groups. Conversely, the current analysis benefits from its large sample size and the analysis of one prothesis placed by one surgeon.
Conclusion
Regarding efficiency compared between navigation- and robotic-assisted procedures, the MAKO robotic-assisted total knee arthroplasty was shorter in operating room time, there was a thinner insert thickness, a shorter length of stay in hospital, and less instrumentation was needed. In the future, implant stock could be reduced because of implant prediction. The combination of these outcomes could make MAKO total knee robotic-assisted surgery time and cost-effective to outweigh its initial cost for purchase and maintenance.
Data availability
All data are anonymous available in a computer database.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- CPM:
-
Continuous passive motion
- IRB:
-
Institutional review board
- LMWH:
-
Low-molecular-weight heparins
- LOS:
-
Length of stay
- OR:
-
Operation room
- RATKA:
-
Robotic-assisted total knee arthroplasty
- SD:
-
Standard deviation
- THA:
-
Total hip arthroplasty
- TKA:
-
Total Knee Arthroplasty
- UKA:
-
Unicompartmental knee arthroplasty
References
Naziri Q, Burekhovich SA, Mixa PJ et al (2019) The trends in robotic-assisted knee arthroplasty: a statewide database study. J Orthop 16:298–301. https://doi.org/10.1016/j.jor.2019.04.020
Lang JE, Mannava S, Floyd AJ et al (2011) Robotic systems in orthopaedic surgery. J. Bone Jt. Surg. Ser. B 93:1296–1299
Jacofsky DJ, Allen M (2016) Robotics in arthroplasty: a comprehensive review. J Arthroplasty 31:2353–2363
Lonner JH (2009) Indications for unicompartmental knee arthroplasty and rationale for robotic arm-assisted technology. Am J Orthop (Belle Mead NJ) 38:3–6
Lonner JH, Moretti VM (2016) The evolution of image-free robotic assistance in unicompartmental knee arthroplasty. Am J Orthop (Belle Mead NJ) 45:249–254
Lonner JH, Fillingham YA (2018) Pros and cons: a balanced view of robotics in knee arthroplasty. J Arthroplasty 33:2007–2013. https://doi.org/10.1016/j.arth.2018.03.056
Pierce J, Needham K, Adams C et al (2020) Robotic arm-assisted knee surgery: an economic analysis. Am J Manag Care 26:205–210. https://doi.org/10.37765/AJMC.2020.43763
Cotter EJ, Wang J, Illgen RL (2020) Comparative cost analysis of robotic-assisted and jig-based manual primary total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/S-0040-1713895
Sousa PL, Sculco PK, Mayman DJ et al (2020) Robots in the operating room during hip and knee arthroplasty. Curr Rev Musculoskelet Med 13:309. https://doi.org/10.1007/S12178-020-09625-Z
Sodhi N, Khlopas A, Piuzzi NS et al (2018) The learning curve associated with robotic total knee arthroplasty. J Knee Surg 31:17–21. https://doi.org/10.1055/S-0037-1608809/ID/JR17SEP0024SSA-15
Marchand KB, Ehiorobo J, Mathew KK et al (2020) Learning curve of robotic-assisted total knee arthroplasty for a high-volume surgeon. J Knee Surg. https://doi.org/10.1055/S-0040-1715126/ID/JR190398OA-25
Kayani B, Konan S, Huq SS et al (2019) Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surgery, Sport Traumatol Arthrosc 27:1132. https://doi.org/10.1007/S00167-018-5138-5
Deckey DG, Rosenow CS, Verhey JT et al (2021) Robotic-assisted total knee arthroplasty improves accuracy and precision compared to conventional techniques. Bone Joint J 103:74–80. https://doi.org/10.1302/0301-620X.103B6.BJJ-2020-2003.R1
Mulier JP, De Boeck L, Meulders M et al (2015) Factors determining the smooth flow and the non-operative time in a one-induction room to one-operating room setting. J Eval Clin Pract 21:205–214. https://doi.org/10.1111/JEP.12288
Sires JD, Craik JD, Wilson CJ (2019) Accuracy of bone resection in MAKO total knee robotic-assisted surgery. J Knee Surg. https://doi.org/10.1055/s-0039-1700570
Marchand KB, Salem HS, Mathew KK et al (2021) The accuracy of computed tomography-based, three-dimensional implant planning in robotic-assisted total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/S-0041-1729548
Zhang J, Ndou WS, Ng N et al (2021) Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/S00167-021-06464-4
Archer A, Salem HS, Coppolecchia A, Mont MA (2021) Lengths of stay and discharge dispositions after total knee arthroplasty: a comparison of robotic-assisted and manual techniques. J Knee Surg. https://doi.org/10.1055/S-0041-1735280
Tompkins GS, Sypher KS, Li HF et al (2021) Robotic vs manual total knee arthroplasty in high volume surgeons: a comparison of cost and quality metrics. J Arthroplasty. https://doi.org/10.1016/J.ARTH.2021.12.018
Abdelfadeel W, Houston N, Star A et al (2020) CT planning studies for robotic total knee arthroplasty. Bone Joint J 102:79–84. https://doi.org/10.1302/0301-620X.102B6.BJJ-2019-1498.R1
Koolmees D, Bernstein DN, Makhni EC (2021) Time-driven activity-based costing provides a lower and more accurate assessment of costs in the field of orthopaedic surgery compared with traditional accounting methods. Arthroscopy 37:1620–1627. https://doi.org/10.1016/J.ARTHRO.2020.11.028
Fang CJ, Mazzocco JC, Sun DC et al (2022) Total knee arthroplasty hospital costs by time-driven activity-based costing: robotic vs conventional. Arthroplast Today 13:43. https://doi.org/10.1016/J.ARTD.2021.11.008
Maritan G, Franceschi G, Nardacchione R et al (2022) Similar survivorship at the 5-year follow-up comparing robotic-assisted and conventional lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/S00167-022-07218-6
Mont MA, Cool C, Gregory D et al (2021) Health care utilization and payer cost analysis of robotic arm assisted total knee arthroplasty at 30, 60, and 90 days. J Knee Surg 34:328–337. https://doi.org/10.1055/S-0039-1695741/ID/JR190145OA-23
Cool CL, Jacofsky DJ, Seeger KA et al (2019) A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res 8:327–336. https://doi.org/10.2217/CER-2018-0136/ASSET/IMAGES/LARGE/FIGURE1.JPEG
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
GL has a financial conflict of interest with Stryker, he received speaker and consultancy fee.
Institutional review board ethical approval was awarded prior to study initiation. This article was primary edited by L. Loomans.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Loomans, L., Leirs, G. & Vandenneucker, H. Operating room efficiency after the implementation of MAKO robotic-assisted total knee arthroplasty. Arch Orthop Trauma Surg 143, 5501–5506 (2023). https://doi.org/10.1007/s00402-023-04834-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04834-w