Abstract
Introduction
The presence of lumbar spine arthrodesis (SA) is associated with abnormal spinopelvic characteristics and inferior outcome post total hip arthroplasty (THA). However, whether patients with upper segment SA are also at increased risk of complications is unknown. This study aims to (1) determine if upper segment SA is associated with inferior THA outcomes; (2) assess spino-pelvic characteristics; and (3) test whether static or dynamic spinopelvic characteristics correlate with outcome post-THA.
Materials and methods
In this retrospective, case-matched, cohort study from a tertiary referral centre, 40 patients (59 hips) that had undergone both THA and any level of spinal arthrodesis (49 THA-Lumb and 10 THA-Cerv) were compared with 41 patients (59 hips) who had THA-only without known spinal pathology. Spino-pelvic characteristics [including severity of Degenerative-Disc-Disease (DDD); spinal balance and stiffness] and outcome, including patient reported outcome measures (PROMs), at minimum of 1-year post-THA were assessed.
Results
THA-Lumb and THA-Cerv groups had greater number of complications and inferior hip and spinal PROMs compared to THA-Only (p < 0.001). Similar spinopelvic characteristics were seen between the THA-Cerv and THA-Lumb, which were significantly different to the THA-only group. The presence of DDD and unbalanced or stiff spine was associated with increased dislocation and inferior PROMs in the whole cohort.
Conclusions
THA in the presence of SA, regardless of level, is associated with inferior outcomes and an increased risk for dislocation. The presence of a SA is associated with increased risk of adverse spinopelvic characteristics. Such characteristics were strongly associated with increased dislocation-risk and inferior PROMs. It is likely that these adverse characteristics are the most important adverse predictor, rather than segment of SA per se.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The growth of an aging population is associated with an increasing prevalence of degenerative musculoskeletal disease [1]. Surgical interventions like total hip arthroplasty (THA) and spinal arthrodesis (SA) have evolved significantly and are now performed with patients having less complications and reporting better patient reported outcomes (PROMs) [2, 3]. Expectantly, the demand of these surgical procedures has increased [4,5,6]. With the improved efficacy of these procedures and the aging population it is inevitable to more frequently encounter patients with degenerate spines (with or without a SA) requiring a THA [1, 7,8,9].
The effect of a stiff spine (such as in the presence of a SA) on THA outcomes has been a topic of significant interest over the recent years [10, 11]. Many studies have determined the negative effect on THA outcomes and the increased risk of complications that such patients experience [12, 13]. These studies have predominantly focused on the role that lumbar spine arthrodesis has on spino-pelvic mobility and in turn THA mechanics [14]. Lumbar spine position is known to have an effect on pelvic position in turn affecting acetabular orientation [15, 16] and thus THA outcome [17]. Patients with lumbar SA have altered spino-pelvic mobility, leaving them susceptible for total hip dislocation despite having appropriate cup orientation on supine radiographs [18]. The deleterious effect of SA is dependent on whether it extends into the sacrum and its length (number of segments involved); the longer the SA, the greater the risk of complications [9, 19, 20]. Together these studies have led arthroplasty surgeons to attempt to account for a patient’s underlying spinal condition to mitigate any future risk for THA complications [16, 21].
To-date it has not been studied whether patients with upper segment SA not involving the lumbar spine are at increased risk of complications, similar to patients with lumbar SA. Furthermore, how the degenerate spine, in the absence of previous spinal surgery, influences THA outcome is inadequately characterised. The study aims to 1. Determine if upper segment SA, akin to observations seen with lumbar SA, is associated with inferior THA outcomes compared to patients without a SA; 2. Assess whether patients with concomitant THA and upper segment SA, exhibited abnormal spino-pelvic characteristics, similar to those seen in the presence of lumbar SA and; 3. Test whether static or dynamic spinopelvic characteristics correlate with outcome post-THA.
Materials and methods
This is an IRB-approved (OHSN-REB 20170312-01H), prospective, cohort study, registered at clinicaltrials.gov (NCT03240484). It stems from a tertiary referral centre with 13 fellowship-trained hip arthroplasty-surgeons and 13 fellowship-trained spinal-surgeons. Study protocol and results of part of this cohort have previously been published [18]. All participants provided written informed consent.
SA-THA cohorts
Enquiring the hospital’s database, a total of 103 patients who underwent both spine arthrodesis and total hip replacements between 2002 and 2018 were identified. Exclusion criteria for participation was severe dementia; inability to answer the questionnaires or come for a clinical review; inability to have radiographs for medical reasons; age over 80 years; and evidence of SA non-union. There were 3 patients who underwent THA with both upper and lumbar spine arthrodesis. These patients were also excluded from the analysis of this study. Finally, 40 patients were eligible to participate and presented for a review; there were 6 Upper Segment SA-THA (THA-Cerv) patients (10 hips) and 34 Lumbar-Spine SA-THA (THA-Lumb) patients (49 hips) (Fig. 1A–C).
THA-Cerv group
The most frequent diagnosis for THA was osteoarthritis (85%). The most common approach used for the THA was posterior (n = 7) and three had a lateral approach. The upper SA fusions predominantly included 1 level anterior cervical decompression fusions (n = 2) and 2 level posterior decompression instrumented fusions (PDIF) (n = 1). The remaining were > 3 level PDIF (n = 1) not extending to the thoracic spine and > 6 level PDIF extending to the thoracic spine (n = 2). All THA-Cerv patients had the THA first, with a mean interval between procedures of 2.2 ± 2.2 years. Most THAs were performed in males (n = 8) and the mean age at review was 70.1 (± 7.2) years. The mean BMI was 29.3 (± 3.9). Detailed demographics of the cases are provided in Table 1.
THA-Lumb group
The most common diagnosis for THA was osteoarthritis (87%). Seventeen THAs (35%) were performed prior to the lumbar SA, while 32 (65%) THAs were performed post-SA. The mean interval between THA and lumbar SA was 5.6 (± 4.5) years. The most common approach used was lateral (n = 24) approach, followed by posterior (n = 16) and direct anterior (n = 9) (Table 2). Most hips received uncemented implants (95%). The most common level of SA was of L4–5 (n = 8), followed by L3–5 (n = 6) and L4–S1 (n = 5) Most SA were 1- or 2-level fusions (20/34), the remaining 14 were of 3 levels or more. Sixteen SA extended into the sacrum. Most THAs were performed in females (n = 26, 53%) and the mean age at review was 71.8 (± 5.2) years. The mean BMI was 28.6 (± 4.1). Detailed demographics of the cases are provided in Table 1.
Controls (THA-only group)
The control group was case matched with the SA groups according to sex, age and BMI (1:1 ratio). Controls were 41 volunteers post-THA (59 hips) recruited from follow-up clinics, ensuring appropriate inclusion criteria were met with a minimum follow-up post-THA of 1 year. The same surgeons operated upon the patients and details are provided in Table 2. None of the controls had any spinal surgery in the past or had previously been reviewed by a spinal surgeon.
Assessments
Patient review—outcome measures
All patients presenting for a review, were asked to complete four validated Patient Reported Outcome Measures (PROMs) questionnaires assessing hip- and spine-function as well as their overall well-being. These included the Oxford Hip Score (OHS) [22], Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score [23], the Oswestry Spine Disability index score (ODI) [24], and the SF-12 physical and mental scores [25]. Patients with bilateral THAs were asked to fill-in WOMAC and OHS questionnaires for each hip.
Thereafter, a clinical review lead by an arthroplasty fellow was performed, during which medical–surgical complications and re-operations were recorded and a clinical examination was performed. The THA-Cerv group patients had a formal assessment of their underlying myelopathy completed with the mJOA as was the only group with myelopathic findings [26].
Radiographic assessments
All patients underwent 4 radiographs at final follow-up:
-
1.
Supine antero-posterior (AP) pelvis
-
2.
Standing AP pelvis
-
3.
Lateral, standing spine–pelvis–hip–proximal femur
-
4.
Lateral, flexed (deep) seated spine–pelvis–hip–proximal femur as per patient comfort—this position was chosen as this is considered a position of increased risk for dislocation and edge loading [27, 28].
The same radiographers, using an agreed protocol, obtained all radiographs [29]. Detailed description of the protocol was previously published [18].
A musculoskeletal staff radiologist reviewed the imaging and reported on any degenerative changes to the lumbar spine for patients in the control and the THA-Cerv group, using the grading scheme for degenerative disc disease (DDD) as described by Esposito et al. [19]. DDD was categorized if two or more diseased levels were present as normal, mild, moderate or severe DDD.
Measurements performed
Radiographic cup orientation (inclination/anteversion) was measured from the AP pelvic radiographs using a validated software (EBRA-cup) [30, 31]. Cup measurements of all patients were performed, independently, by 2 observers (an arthroplasty fellow and a resident) blinded to patient outcome; furthermore, 10 patients underwent a repeat measurement by the fellow. The differences in inclination/anteversion between the standing and sitting positions, defined as Δ, were calculated as:
ΔInclination = Standing_Inclination − Supine_Inclination.
ΔAnteversion = Standing_Anteversion − Supine_Anteversion.
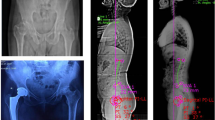
A number of spinopelvic parameters were measured from the spine–pelvis–hip radiographs (Fig. 2A–D) by a fellowship-trained musculo-skeletal radiologist. These included pelvic–incidence (PI) [32,33,34], sacral slope (SS), pelvic tilt (PT), lumbar lordosis angle (LL), pelvic–femoral angle (PFA) [35], and ante-inclination of the cup [34].
Radiographic assessment of spine–pelvic mobility and acetabular cup orientation. A Supine AP pelvis, B Standing AP pelvis with EBRA cup measurements overlaid, C Sitting lateral radiograph, D standing lateral radiographs with pelvic measurements demonstrated: sacral slope (SS), pelvic incidence (PI), pelvic femoral angle (PFA), acetabular anti-inclination (AI)
Parameters calculated
-
The difference in PT between standing and sitting (ΔPTstanding/seated) was calculated as:
ΔPTstanding/seated = PTseated − PTstanding.
-
The difference in PFA between standing and sitting (ΔPFAstanding/seated), reflects the arc of hip movement in this transition and was calculated as:
ΔPFAstanding/seated = PFAseated − PFAstanding.
-
The difference in Lumbar lordosis between standing to sitting (ΔLumbarLordosisstanding/seated), was calculated as:
ΔLumbarLordosisstanding/seated = LLstanding – LLseated.
-
The total sagittal, flexion arc of movement was calculated as the sum of hip and lumbar spine flexion (Total Flexion Arc; TFA).
TFAstanding/seated = ΔPFAstanding/seated + ΔLumbarLordosisstanding/seated.
-
The difference between pelvic incidence and lumbar lordosis was calculated as PI-LL = PI-LLstanding. A PI-LL of > 10° was defined as a mismatch within the “flatback” range.
-
A hip user index was calculated as \(\frac{\Delta \mathrm{PFA}}{\Delta \mathrm{LL}+ \Delta \mathrm{PFA}} \times 100\). A high percentage indicates that hip and pelvic movement contribute much and lumbar spine flexion little to overall sagittal movement [36]. Previous normative data from a pre-operative cohort has indicated a threshold value of 80% for being a hip user [36].
-
The patient’s combined sagittal index was calculated as the sum of the cup ante-inclination and pelvic–femoral angle [37]. Values were calculated from both the seated and standing position lateral radiographs.
-
Patients were categorised according to the dynamic spino-pelvic characteristics (Phan et al., [16]):
Power analysis based on one prior study [7] on the proportion of patients who experienced dislocation after THA either with or without spinal arthrodesis determined that 43 hips in each group would be needed for sufficient power (b = 0.8, a = 0.05).
Statistics
Comparison were performed between Groups (THA-Cerv; THA-Lumb; THA-only) and between THAs with different degree of degenerative spinal deformity as per static and dynamic radiographic evaluations. Static evaluations included 3 group comparisons (normal or mild; moderate; and severe DDD). Dynamic evaluations included 2 group comparisons—balanced and flexible and abnormal combinations (unbalanced and flexible; balanced and rigid and unbalanced and rigid). Sub-analysis was also performed accounting for surgical approach and excluding cases that underwent direct anterior approach as this approach has been reported to be associated with reduced incidence of instability in the setting of spinal arthrodesis. Statistical analysis was carried out with non-parametric tests. The Mann–Whitney U and Kruskal Wallis tests were used for scale data. The Fisher’s exact and Chi-square tests were used for categorical data. Spearman’s test was used for correlations. Statistical significance was set at p < 0.05. All statistical analysis was carried out, using SPSS software, version 21, IBM.
Results
Excellent intra- and inter-observer reliabilities were identified for both cup and spinal measurements. Intra- and inter-class variability for cup orientation were ICC: 0.86 (95% CI 0.82–0.90) (p < 0.001) and ICC: 0.93 (0.90–0.96), (p < 0.001).
Clinical outcomes of THA with Lumbar and Cervical SA (Table 3)
Both the THA-Lumb and THA-Cerv groups had greater number of complications when compared to THA-Only (p < 0.001). Both the THA-Lumb (OHS:33.0, WOMAC:71.9, ODI:31.2%) and THA-Cerv (OHS:27.0, WOMAC:64.5, ODI:33.9%) groups had inferior hip and spinal PROMs when compared to the THA-only group (OHS:42.9, WOMAC:89.2, ODI:11.7%) (p < 0.001) (Table 3). In addition, 69% THA-Cerv patients were found to have mild to moderate myelopathy as measured with the modified Japanese Orthopaedic Association (mJOA) score. There was no difference in complication rates for the THA-SA groups between different approaches (DAA: 1/9; lateral: 4/27; Posterior: 3/23; p = 0.957). Considering THAs with lateral and posterior approaches only, the presence of SA was associated with increased risk of complications (15/50) compared to THA-only (0/21; p < 0.001). This included the increased dislocation risk (7/50; THA-Cerv: 3, THA-Lum: 4) compared to THA-only (0/21) (p = 0.002). One of the dislocations in the THA-Lumb group was sustained after a direct anterior approach (1/9).
Static and dynamic spinopelvic characteristics by group (Tables 4, 5)
The cohort’ mean supine cup orientation had an inclination/anteversion of 42.7/22.0°. There was no difference in inclination between groups. The THA-Cerv group had a significantly lower anteversion (11.0° ± 8.2°) compared to the THA-Lumb (23.2° ± 9.0°) and the THA-only (23.2° ± 8.6°) groups (Table 3). The change in cup orientation when moving from supine to standing was similar across all groups.
Similar spinopelvic characteristics were seen between the THA-Cerv and THA-Lumb, which were significantly different to the THA-only group. The THA-Cerv (56.1° ± 9.7°) and THA-Lumb (61.5° ± 11.9°) groups had significantly greater PI compared to the THA-only (46.5° ± 12.6°) group (p = 0.002). When standing both the THA-Lumb and THA-Cerv had significantly smaller lumbar lordosis and greater standing Pelvic–Tilt and Pelvic–Femoral Angle compared to the THA-only group. Accordingly, PI-LL was significantly greater in the THA-Cerv (20.0° ± 18.7°) and the THA-Lumb (18.8° ± 15.0°) groups compared to the THA-only group (− 1.2° ± 9.9°) (p < 0.001). The THA-Cerv and THA-Lumb Groups had a lesser ΔLumbarLordosisstanding/seated than the THA-only group. There was no difference in ΔPFAstanding/seated between the 3 groups. However, the TFAstanding/seated was significantly less in the THA-Cerv and THA-Lumb Groups. The Hip-User-Index was greatest in the THA-Lumb (83.1%) followed by the THA-Cerv (77.6%) and the THA-only groups (71.4%) (p < 0.0001).
Abnormal SP characteristics were more prevalent (OR: 14; 95% CI: 5.8–34.1) in patients with SA (both of the lumbar– and cervical–spine) compared to controls. The degree of DDD was associated with different static and dynamic SP characteristics and outcome, as detailed in Table 5. Patients with severe DDD had increased standing Pelvic–Tilt and reduced Lumbar Lordosis angle compared to patients with moderate and mild/no DDD. Patients with severe DD had reduced ΔLumbarLordosisstanding/seated compared to moderate and mild/no DDD. The TFAstanding/seated was reduced in the severe DDD group. The ΔPFAstanding/seated was similar between all groups. Thus, HUI was greater in the severe DDD group.
Clinical outcome and spinopelvic characteristics
Clinical outcome was associated with spinopelvic characteristics. THAs that dislocated had significantly greater PI-LL compared to THAs that didn’t (24.2 ± 9.2 vs. 9.3 ± 16.1; p < 0.0001). Patients with dislocation had an unbalanced and mobile (n = 5) or an unbalanced and stiff (n = 3) spine. Patients with severe DDD had inferior PROMs for all measures obtained (Table 5). Similarly, patients with balanced and flexible lumbar spine had significantly superior OHS (42.0 ± 5.8 vs. 32.4 ± 11.0; p < 0.0001), ODI (13.1 ± 13.1 vs. 33.2 ± 10.0; p < 0.0001), WOMAC (85.3 ± 18.7 vs. 72.5 ± 21.8; p < 0.0001), SF12physical (43.9 ± 11.0 vs. 33.5 ± 13.4; p < 0.0001) and SF12mental (56.4 ± 9.9 vs. 51.1 ± 11.8; p = 0.014) compared to the other groups.
Conclusions
Previous studies [12, 13, 18], showed that the presence of a Lumbar-SA is associated with inferior THA outcome. In this study, we go further to reveal that any level of spinal arthrodesis, regardless of whether it involves the upper or lower spine, is associated with inferior patient outcome and should alert arthroplasty surgeons of the inferior outcomes such patients for multitude of reasons, amongst which is the likely to be the altered spinopelvic characteristics and any residual neurological deformity. The presence of a pathological lumbar spine (whether in presence of an arthrodesis or not) is associated with specific altered spinopelvic characteristics (i.e., spinal stiffness, spino-pelvic imbalance) which would be of value to be identified prior to the arthroplasty procedure as this study illustrated that these characteristics are associated with increased risk of complications and reduced patients reported outcomes even in patients without SA. Given that these parameters do not change with a THA, surgeons should be aware of their presence and appropriately council patients and position/select components to allow for impingement-free range of movement in such patients that demand more sagittal movement arc of their THAs.
Patients with SA, regardless of its location exhibited inferior outcome regardless of the outcome measure used. Both the THA-Lumb and THA-Cerv groups had a significantly greater prevalence of complications (especially dislocation) and need for further surgery. Furthermore, both groups had inferior OHS, WOMAC and ODI scores, compared to the THA-only group. It is thus evident that the presence of a cervical SA, despite the lack of extension into the lumbar spine is associated with inferior outcome post THA. This is likely to be the case due to a number of reasons that this study has highlighted. First, these patients are more likely to suffer with DDD of the lumbar spine and have abnormal dynamic spinopelvic characteristics (only 1 out 10 illustrated a flexible and balanced spine). Such spinopelvic characteristics are akin to those seen in patients with lumbar SA, despite the lack of symptoms or history of lumbar pathology. Second, a factor that requires further analysis is the patient’s neurological baseline. Many patients with history of lumbar SA may have permanent weakness or altered proprioception as a result of their underlying conditions. Furthermore, the indication for cervical spine decompression and fusion remains cervical cord compression with cervical myelomalacia [38]. In line with the literature, 69% of the THA-Cerv group was found to have some degree of myelomalacia. Given the low cohort numbers and this singular assessment of myelopathy it is difficult to conclude that the patient’s neurological status played a significant role in the outcome or hip instability. What role a patient’s neurologic function has on their spino-pelvic mobility has yet to be studied and, therefore, remains a possible important avenue for further research to further elucidate the true role spinal pathology has on spino-pelvic mobility.
In this study, findings that complement the literature on spinopelvic characteristics were identified. Esposito et al. in 2016 showed the role that lumbar arthrosis, caused by degenerative disc disease (DDD), has on spino pelvic characteristics. The authors found that patients with DDD had greater amount of standing pelvic tilt and lowered sacral slope and lordosis levels than patients without spinal pathology [19]. Contrary to Esposito et al. patients in all groups exhibited the same amount of hip flexion. This is likely to be the case, because the study protocol involved deep seated radiographs which have shown to be more testing on the hip and spine range of movement compared to the relaxed-seated position reported by Esposito et al. [19]. It was of interest that a significant proportion of patients without known spinal problems exhibited moderate or severe DDD (34/59) and 14/59 exhibited some form of abnormal spinopelvic characteristic as per Phan et al. [16]. This raises the importance of reviewing spinopelvic characteristics in patients presenting for THA and is in line with observations by Vigdorchik et al. that most patients with a stiff spine presenting for a THA, do not have a spinal arthrodesis in situ [39].
This study included patients with a variety of spinal characteristics (known and unknown disease). We were thus able to test for associations between static (DDD) and dynamic (as per Phan et al.) radiographic findings of spinal disease. It was evident that patients with severe DDD and abnormal findings (unbalanced and or stiff) had a greater prevalence of complications and inferior PROMs for all outcome measures obtained compared to patients with no DDD and/or balanced and flexible spine. Although such characteristics were more prevalent (OR 14; 95% CI 5.8–34.1) in patients with SA (both of the lumbar– and cervical–spine), these characteristics were also present in patients without SA and had overall had a strong association with inferior outcome. It is hypothesised that it is the presence of the characteristics, rather than the presence or a SA, that is the stronger predictor of inferior outcome. Since ΔLL and PI-LL do not change as part of the THA, surgeons should be aware of these findings and appropriately consult patients. Patients with spinal stiffness, may require more from their hip to achieve a given task and surgeons should be encouraged to robustly pre-operatively plan in terms of component orientation (acetabular and femoral orientation and offset) and choice of component used (e.g., dual mobility). Furthermore, our study findings are in line with those reported by DelSole et al. [40], patients that exhibited instability post-THA showed greater lumbar–spine imbalance (PI-LL).
This study is not without its limitations. The overall number of recruited patients with both THA and Cervical SA is low as this is a single-centre study. Recruitment of this patient group was exceptionally difficult with many patients arguing their low mobility as a main limitation to present for clinical review. This may have created a selection bias for those patients that did present to clinic for those that are of better health and overall better mobility. Despite this even with the low number of THA-Cerv patients our most important assessments (i.e., number of dislocations, Hip PROMs) were found to be significantly affected by the presence of cervical spinal arthrodesis. As per power calculation, the study is underpowered in terms of the THA-Cerv group; however, statistical significance was still present illustrating the important associations detecting in this group. Due to the low number of patients who have both a cervical SA and a primary THA this group consists of different fusion levels. This results in a heterogenous group. The subdivision of this group into more homogeneous subgroups could not be carried out due to the small number. This limitation also applies to the lumbar group. Here, the patients with SA up to S1 and the patients who only received SA in the lumbar spine were combined. Again, the number of subgroups would be too small for a meaningful analysis. However, to date, there are no studies which compare patients with cervical arthrodesis and THA only patients. Hence, this is the first study of its kind and thus of clinical importance, as it highlights the relevant associations. Further collaborative studies or registry data would be able to provide more additional information and evidence on the novel findings reported. Second, we matched patients as per demographic parameters of gender, age and BMI. Surgical parameters that could have potentially influenced outcome of THA such as approach were not matched for. However, studies have failed to show a significant difference in THA outcome with the different approaches [41]. To account for any surgical approach-biases, sub-analyses were performed which failed to show an approach-related effect. Furthermore, one of the hips sustained a dislocation after a direct anterior approach to the hip.
In conclusion, THA in the presence of SA, regardless of level, is associated with inferior outcomes and an increased risk for dislocation. The presence of a SA is associated with increased risk of adverse spinopelvic characteristics (statically and dynamically). Such characteristics were strongly associated with increased dislocation-risk as well as inferior patient reported outcome scores and it is likely that these adverse characteristics are the most important adverse predictor, rather than segment of SA per se. We argue that any patient with a history of any level of spinal arthrodesis undergoing THA should have dynamic lateral radiographs obtained to better examine their spinopelvic movement to better mitigate their risk of complication and inferior functional outcomes.
Data, materials and/or code availability
N/A.
References
Park JH, Hong JY, Han K, Suh SW, Park SY, Yang JH et al (2017) Prevalence of symptomatic hip, knee, and spine osteoarthritis nationwide health survey analysis of an elderly Korean population. Medicine 96(12):e6372
Hassanzadeh H, Jain A, El Dafrawy MH, Mesfin A, Neubauer PR, Skolasky RL et al (2013) Clinical results and functional outcomes of primary and revision spinal deformity surgery in adults. J Bone Jt Surg Am 95(15):1413–1419
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet (London, England) 370(9597):1508–1519
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am 89(4):780–785
Rajaee SS, Bae HW, Kanim LE, Delamarter RB (2012) Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine 37(1):67–76
Rushton A, Wright C, Heap A, White L, Eveleigh G, Heneghan N (2014) Survey of current physiotherapy practice for patients undergoing lumbar spinal fusion in the United Kingdom. Spine 39(23):E1380–E1387
Barry JJ, Sing DC, Vail TP, Hansen EN (2017) Early outcomes of primary total hip arthroplasty after prior lumbar spinal fusion. J Arthroplasty 32(2):470–474
Bedard NA, Martin CT, Slaven SE, Pugely AJ, Mendoza-Lattes SA, Callaghan JJ (2016) Abnormally high dislocation rates of total hip arthroplasty after spinal deformity surgery. J Arthroplasty 31(12):2884–2885
Perfetti DC, Schwarzkopf R, Buckland AJ, Paulino CB, Vigdorchik JM (2017) Prosthetic dislocation and revision after primary total hip arthroplasty in lumbar fusion patients: a propensity score matched-pair analysis. J Arthroplasty 32(5):1635–40.e1
King CA, Landy DC, Martell JM, Luu HH, Shi LL, Lee MJ (2018) Time to dislocation analysis of lumbar spine fusion following total hip arthroplasty: breaking up a happy home. J Arthroplasty 33(12):3768–3772
Malkani AL, Himschoot KJ, Ong KL, Lau EC, Baykal D, Dimar JR et al (2019) Does timing of primary total hip arthroplasty prior to or after lumbar spine fusion have an effect on dislocation and revision rates? J Arthroplasty 34(5):907–911
Buckland AJ, Puvanesarajah V, Vigdorchik J, Schwarzkopf R, Jain A, Klineberg EO et al (2017) Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Jt J 99(5):585–591
Diebo BG, Beyer GA, Grieco PW, Liu S, Day LM, Abraham R et al (2018) Complications in patients undergoing spinal fusion after THA. Clin Orthop Relat Res 476(2):412–417
Sultan AA, Khlopas A, Piuzzi NS, Chughtai M, Sodhi N, Mont MA (2018) The impact of spino-pelvic alignment on total hip arthroplasty outcomes: a critical analysis of current evidence. J Arthroplasty 33(5):1606–1616
Kanawade V, Dorr LD, Wan Z (2014) Predictability of acetabular component angular change with postural shift from standing to sitting position. J Bone Jt Surg Am 96(12):978–986
Phan D, Bederman SS, Schwarzkopf R (2015) The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Jt J 97-B(8):1017–1023
Grammatopoulos G, Thomas GE, Pandit H, Beard DJ, Gill HS, Murray DW (2015) The effect of orientation of the acetabular component on outcome following total hip arthroplasty with small diameter hard-on-soft bearings. Bone Jt J 97(2):164–172
Grammatopoulos G, Gofton W, Jibri Z, Coyle M, Dobransky J, Kreviazuk C et al (2019) 2018 frank stinchfield award: spinopelvic hypermobility is associated with an inferior outcome after tha: examining the effect of spinal arthrodesis. Clin Orthop Relat Res 477(2):310–321
Esposito CI, Miller TT, Kim HJ, Barlow BT, Wright TM, Padgett DE et al (2016) Does degenerative lumbar spine disease influence femoroacetabular flexion in patients undergoing total hip arthroplasty? Clin Orthop Relat Res 474(8):1788–1797
Salib CG, Reina N, Perry KI, Taunton MJ, Berry DJ, Abdel MP (2019) Lumbar fusion involving the sacrum increases dislocation risk in primary total hip arthroplasty. Bone Jt J 101(2):198–206
Luthringer TA, Vigdorchik JM (2019) A Preoperative workup of a “Hip-spine” total hip arthroplasty patient: a simplified approach to a complex problem. J Arthroplasty 34(7s):S57-s70
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ et al (2007) The use of the Oxford hip and knee scores. J Bone Jt Surg Br Vol 89(8):1010–1014
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15(12):1833–1840
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine 25(22):2940–2952
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Tetreault L, Kopjar B, Nouri A, Arnold P, Barbagallo G, Bartels R et al (2017) The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 26(1):78–84
McDonnell SM, Boyce G, Baré J, Young D, Shimmin AJ (2013) The incidence of noise generation arising from the large-diameter Delta Motion ceramic total hip bearing. Bone Jt J 95(2):160–165
Pierrepont J, Hawdon G, Miles B, Connor BO, Baré J, Walter L et al (2017) Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. Bone Jt J 99(2):184–191
Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ et al (2008) A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Jt Surg Am Vol 90(Suppl 4):47–66
Krismer M, Bauer R, Tschupik J, Mayrhofer P (1995) EBRA: a method to measure migration of acetabular components. J Biomech 28(10):1225–1236
Langton DJ, Sprowson AP, Mahadeva D, Bhatnagar S, Holland JP, Nargol AV (2010) Cup anteversion in hip resurfacing: validation of EBRA and the presentation of a simple clinical grading system. J Arthroplasty 25(4):607–613
Le Huec JC, Saddiki R, Franke J, Rigal J, Aunoble S (2011) Equilibrium of the human body and the gravity line: the basics. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cervical Spine Res Soc 20(5):558–563
Le Huec JC, Aunoble S, Philippe L, Nicolas P (2011) Pelvic parameters: origin and significance. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cervical Spine Res Soc 20(Suppl 5):564–571
Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R et al (2017) Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Jt J 99(1_Suppl_A):37–45
Philippot R, Wegrzyn J, Farizon F, Fessy MH (2009) Pelvic balance in sagittal and Lewinnek reference planes in the standing, supine and sitting positions. Orthop Traumatol Surg Res OTSR 95(1):70–76
Innmann MM, Merle C, Phan P, Beaulé PE, Grammatopoulos G (2020) How can patients with mobile hips and stiff lumbar spines be identified prior to total hip arthroplasty? A prospective, diagnostic cohort study. J Arthroplasty 35(6s):S255–S261
Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, Dorr LD (2018) Late dislocation following total hip arthroplasty: spinopelvic imbalance as a causative factor. J Bone Jt Surg Am 100(21):1845–1853
Shimizu T, Lehman RA Jr, Pongmanee S, Alex Sielatycki J, Leung E, Riew KD et al (2019) Prevalence and predictive factors of concurrent cervical spinal cord compression in adult spinal deformity. Spine 44(15):1049–1056
Vigdorchik JM, Sharma AK, Dennis DA, Walter LR, Pierrepont JW, Shimmin AJ (2020) The majority of total hip arthroplasty patients with a stiff spine do not have an instrumented fusion. J Arthroplasty
DelSole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, Buckland AJ (2017) Total hip arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? J Arthroplasty 32(6):1910–1917
Meermans G, Konan S, Das R, Volpin A, Haddad FS (2017) The direct anterior approach in total hip arthroplasty: a systematic review of the literature. Bone Jt J 99(6):732–740
Acknowledgments
We thank Dr Zaid Jibri for his contributions in reviewing and reporting on the study imaging. Furthermore, we wish to acknowledge that author T.S.B. was supported by the fund ″Innovative Medical Research″ of the University of Muenster Medical School (Post Doc Fellowship SC 5 1 20 01).
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Study conception and design were performed by MJC, TS-B, WG, PP, PEB, and GG. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by MJC, TS-B, and GG and all authors commented on previous versions of the manuscript. All authors have read and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors A,B,C,D, and F declare they have no financial interests. Author E has received educational support from Zimmer-Biomet and MicroPort. Author G has received royalties from Corin, MicroPort, Medacta; has received consultancy fees from Corin, MicroPort, MatOrtho, Zimmer Biomet; has received research support from Zimmer Biomet; has received publishing royalties from Wolters Kluwer and is a committee member for the International Society for Hip Arthroscopy. Author H has received consultancy fees from Formus Labs. The authors have no conflicts of interest to disclose that are related to the submitted work.
Research Involving human participants and/or animals
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ottawa Health Science Network Research Ethics Board at The Ottawa Hospital (No. 20170312) approved this study
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schmidt-Braekling, T., Coyle, M.J., Dobransky, J. et al. Spinal pathology and outcome post-THA: does segment of arthrodesis matter?. Arch Orthop Trauma Surg 142, 3477–3487 (2022). https://doi.org/10.1007/s00402-021-04220-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04220-4