Abstract
Introduction
Total hip arthroplasty (THA) rates have increased dramatically in the recent decades worldwide, with Germany being one of the leading countries in the prevalence of THA. Simultaneously, a rising number of revision procedures is expected, which will put an enormous economic burden on future health care systems.
Methods
Nationwide data provided by the Federal Statistical Office of Germany were used to quantify primary and revision arthroplasty rates as a function of age and gender. Projections were performed with use of Negative Binomial and Poisson regression models on historical procedure rates in relation to population projections from 2020 to 2060.
Results
A 62% increase in the incidence rate of primary THAs is projected until 2060. At the same time, the annual total number of revision procedures is forecast to rise about 40% by the year 2060. The highest numbers of revision arthroplasties were calculated around year 2043. The greatest proportions of revision surgery will be observed in women and in those aged 70 years or older. The revision burden is projected to stabilize around 15% by 2060.
Conclusions
The present projections allow a quantification of the increasing economic burden that (revision) THA will place on the German health care system in the upcoming decades. This study may serve as a model for other countries with similar demographic development as the country-specific approach predicts a substantial increase in the number of these procedures. This highlights the need for appropriate financial and human resource management in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite varying incidences of total hip arthroplasty (THA) in different countries [1,2,3,4], a future increase in total number has been predicted worldwide. Many reasons for this trend have to be taken into account, including not only the demographic change of the general population and the increase of unfavorable risk factors (obesity, osteoathritis), but also a steadily rising number of studies reporting the benefits in patients’ quality of life and function, which has led to an expansion of surgical indications over time [5]. While in the United States (and also in some European countries like the UK, France or Scandinavia) the population is still growing due to high immigration and fertility rates, the demographic and economic characteristics of the United States cannot be generalized to other industrialized countries, although the global demographic pattern is similar around the world. Germany and others (such as Italy, Russia or most Eastern European countries) face population declines in the near future due to lower birth and immigration rates, that are unable to make up for the aging of the population. Based on current projections, many other countries will likely be heading in the same direction within the next few decades [6]. In Germany, the incidence of THA is amongst the highest around the world, due to a relatively old population and a social healthcare system, which provides almost unlimited access to all parts of orthopedic treatment. However, as the working population is shrinking and increasingly aging, the healthcare system faces the challenge of higher demand and costs.
Simultaneously, nations will inevitably be confronted with the challenge of a rising number of revision procedures. Revision may be due to deep infection, aseptic loosening, instability, periprosthetic fracture, prosthetic failure and wear as well as unexplained pain, to list the most common causes. In contrast to primary THA, revision THA is technically more demanding requiring extensive surgical exposure and careful management of periprosthetic bone loss [7,8,9]. Furthermore, higher hospital cost, longer length of stay, and longer operative time along with an associated higher perioperative risk of complications and mortality [10, 11] add to the complexity of revision THA [12], emphasizing its great economic burden.
In Germany, the incidence of THA is one of the highest worldwide and currently ranked second among the countries of the Organization for Economic Cooperation and Development (OECD), accounting for over 230,000 operations (283 THA per 100,000 residents) in 2016. According to national projections [4], this rate might further rise considerably due to the demographic change in the upcoming years. Subsequently, the implications of the constantly aging population, with a higher rate of comorbidities and risk for revision surgery, will certainly affect the inpatient care.
Therefore, the aim of the current study was to provide reliable projections regarding the demand for primary and revision arthroplasties which are crucial for political decision-makers and also for other stakeholders like insurances, industry or hospitals.
Patients and methods
Although the German national registry for hip and knee arthroplasties (Endoprothesenregister Deutschland, EPRD) has been constantly evolving since its establishment in 2010, the completeness of coverage reached just around 60% in 2017 [13]. Therefore, the current analysis was not based on the data from this registry, but from the national inpatient statistics of Germany. This national database contains all annual inpatient discharge reports performed in German hospitals and medical institutions, with the exception of military and psychiatric facilities. The data are based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Edition (ICD-10) and the German procedure classification system (OPS), which is the official classification system for encoding surgical procedures in Germany. These statistics contain anonymized data from the Federal Bureau of Statistics, sustaining plausibility checks and data validations on a medical and economic level. All cases reported between 2007 and 2017 were analyzed based on the corresponding OPS codes in its actual version (See Table 1, Supplementary material). During the study period, no coding changes were performed. Age was categorized in 11 groups: < 45, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, and 90 years and older.
Population data were available from the official statistics of population projection until 2060 [14]. These population projections take into account of future mortality, and immigration rate (Fig. 1). The projection model was based on a moderate life expectancy (male: 84.4 years, female: 88.1 years) with constant trend of birth (1.55 children per female) and death rates and a higher rate of immigration (immigration rate: 250,000 per year).
Statistics
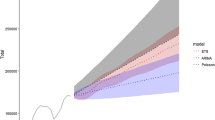
The annual incidence and prevalence of primary and revision THA was modelled by means of Negative Binomial and Poisson regression techniques, respectively, using age, gender and calendar year as covariates to account for differences in prevalence among population subgroups as well as changes over time.
Models were fit based both on the Negative Binomial distribution and Quasi-Poisson likelihood, and over-dispersion was accounted for using the SAS procedure genmod. The two model approaches yielded virtually identical results. Given that the Pearson Chi-Square residuals displayed less spread using the Negative Binomial distribution, all analyses were finally carried out using the Negative Binomial model (Table 2 and Fig. 1, Supplementary material).
The incidence rates (IR) were calculated by dividing the estimated number of arthroplasties for the national total and for each age subgroup by the corresponding official population forecast.
As the incidence rate from 2007 to 2017 displayed a non-linear pattern (see also Fig. 4), it was inappropriate to fit a parametric slope. Instead, the average incidence for 2007–2017 was used to represent baseline incidence for predictions which also accounted for the changing population at risk over time (i.e., due to changing demographics or age structure of the population). Expected mean incidence was adjusted for population size using age-specific population numbers.
For further investigation, we separately modeled the number of revision arthroplasties and revision procedures without change of the implant, as well as THA removals, to analyze possible differences and changes over time, regarding one-stage or two-stage revision surgery.
Additionally, we estimated the revision burden by dividing the number of revisions in the form of replacements or extractions by the number of all primary and revision hip arthroplasties based on the baseline years (2007–2017), which is a concept previously introduced by Malchau et al. [15].
All statistical analyses were performed with SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline years: 2007–2017
From 2007 to 2017, a total of 2,395,113 primary hip arthroplasties were recorded in Germany. During that time, the annual number of procedures rose from 204,018 in 2007 to 238,072 in 2017, representing an increase of 16.7% (Table 1). With repect to the population growth, the annual overall incidence changed substantially from 248 per 100,000 to 292 per 100,000 residents (P < 0.001).
At the same time, 379,960 revision procedures of THA were performed, with the annual total number and the incidence (43.4 per 100,000 inhabitants in 2007 and 43.8 per 100,000 in 2017) remaining fairly constant over time. Due to the rising number of primary THA, the revision burden decreased from 14.6% in 2007 to 13.2% in 2017, which, in contrast, did not reach statistical significance (P > 0.05). While the total number and incidence of revision arthroplasties showed no significant change during the study period, the number of revisions without change of the primary implant substantially decreased (− 20.4%). At the same time, a rising number of THA removals (+ 35.6%) has been reported, indicating a possibly greater utilization of two or multi-stage revision surgery.
Overall, women had a 1.2 times higher relative risk for revision surgery compared to men, the number of which increases significantly towards higher age, with an over twofold higher relative risk among females in patients aged 80 and older.
Projection years: 2018–2060
Based on our projection models, we project a 62% increase in the incidence rate of primary THAs between 2018 and 2060 for Germany (2018: IR = 287.2 per 100,000, [95% CI 280.9–293.6 per 100,000] versus 2060: IR = 402.5 per 100,000, [95% CI 393.6–411.5 per 100,000]) (Fig. 2), leading to a projected total number of 271,223 primary THAs in 2060 (95% CI 265,279–277,301). The highest increase in patients was modeled in patients older than 80 years, which will increase over 70%; whereas, hip replacements in younger patients are forecast to follow a constant or even negative trend (Fig. 3).
Overall, the annual total number of revision procedures (all procedures relating to the index arthroplasty) is expected to rise about 40% by the year 2060, accounting for 47,794 (95% CI44,405–51,455; IR = 70.6 per 100,000, 95% CI 66.5–75.7) procedures (Fig. 4). Revision arthroplasties are projected to grow from 28,231 in 2017 to 37,773 (95% CI 35,125–40,558) in 2060, which represent an increase of 34%, while the number of THA removals is forecasedt to grow moderately to 5,040 (95% CI 4730–5373) (+ 10%).
In total, the incidence of revision arthroplasties is projected to rise significantly to 55.7 per 100,000 residents (+ 40%) in 2060 (P < 0.01) (Fig. 5).
The highest numbers of revision arthroplasties and overall revision procedures are expected around year 2043, with a total number of 52,152 (95% CI 48,471–56,092) overall revision procedures and 41,283 (95% CI 38,431–44,348) revision arthroplasties. These numbers represent an increase of over 44%.
On the basis of these estimates, the revision burden for total hip replacements is projected to stabilize around 15% by 2060.
We observed the greatest proportions of revision THA in women and in those aged 80 years or older (Fig. 6).
Discussion
Based on our analysis, we project a substantial increase in total number and incidence of primary and revision THA over the next four decades. The trend in demand combined with the increasing number of revision procedures represents an immense future burden for an already financially strained healthcare system. It emphasizes the need for qualified surgeons to meet the demand and further research to improve the reliability and survivorship of hip arthroplasties [2]. To our knowledge, this is the first study to provide quantification of the demand for primary and revision hip arthroplasties in Germany through 2060.
The analyses were modeled separately for females and males. Due to the change of demographics within the projection period, the highest numbers of hip revision surgery were calculated around year 2043, followed by a consistently high incidence until 2060. Incidences of revision arthroplasties were found to be markedly higher in females and patients aged 80 years or older.
Currently, there are few studies examining future trends relating to hip revision surgery, both internationally and specifically for Germany. Recently, Pilz et al. published projections of primary hip arthroplasty until the year of 2040. They found a growth rate of 27% in THA counts, whereas incidence rate remained constant over all age classes. Thus, the future demographic change to an older population as well as an increase in life expectancy, rather than a general increase in the operation frequency, was concluded to be the main reason for the increasing patient numbers [4].
In the present study, we provide an even longer-term projection span (by year 2060) and are also able to identify an increase of almost 62% until 2060 for primary THA in Germany. However, throughout the two decades following the year 2040, a gradual stabilization of the incidence rate can be identified, which can be interpreted as a sign of a potential saturation in demand. A similar development has already been reported for the four most common orthopedic/trauma surgery diseases in Germany by Petzold et al. [16], who reported an increase in physician consultations until 2040, with a subsequent decrease until 2050. The authors concluded that comprehensive needs assessment and planning are needed to create health care provision structures and processes that address potential changes in utilization behavior, emphasizing the need for reliable projections of future demand for the most common orthopedic procedures.
Although a direct comparison between different countries is complicated by various factors, such as different demographics, inclusion criteria as well as social and economic influences, the calculations appear to be consistent with the reports from other countries. Kurtz et al. [2] forecasted the highest growth of 174% between 2005 and 2030 in the United States, whereas a 66% increase in the incidence rate of primary THA between 2013 and 2046 is projected for Australia [1]. Presumably due to decreasing population numbers (i.e., lower birth rates), the growth rate is less pronounced in European populations. Culliford et al. predicted an increase of 32% from 2015 to 2035 in the UK [17] and a Swedish publication reported a 25% increase in THA from 2013 to 2030 [3].
Regarding projection of revision THA, only few publications are available in the literature, whereas none can be found for Germany. A recent publication from France predicted a 43.8% or 43.5% increase for the period 2018–2050, depending on different scenarios that were calculated [18]. These projections can be confirmed by the calculations of the present study with an overall increase of revision THA of 40% in Germany until 2060. In the USA, the total number of revision arthroplasty procedures performed in 2005 was calculated to double by the year 2026, with an increase of 137% until 2030 [2].
The increase in revision surgeries following THA seems to be a result of the combination of trends, such as higher implantation numbers of primary THA, younger surgical candidates, and increasing life expectancy, resulting in an increased population at risk [19]. Additionally, the incidence of obesity is postulated to increase the rate of primary THA as obese patients might develop arthritis at an earlier stage [20]. This will also affect the rates of revision surgery as primary THA again will be potentially performed in younger patients, who may require revision surgery at an earlier stage [21].
When taking a historical view, revision THA volume in the USA increased from 28,429 in 1993 to 48,295 in 2014. However, the relative proportion of revision compared to primary THA, the so-called revision burden, during this time period decreased from 21.3% in 1993 to 13.0% in 2014, due to the tremendous increase in primary THA [22]. This ratio can easily be calculated but is a complex measure affected by both more recent surgical practices and also by historical treatment methods. It has several advantages related to large population reporting. It can be calculated for any population or registry and may be followed for change or trends over time. It does not require direct data linkage between the original and revision surgery, which in general is difficult to perform [23].
According to the present data, we identified a slight decrease in revision burden in the past decade in Germany. However, we presume that this is due to the continuously rising number of primary THA as the “denominator variable”. Given a stabilization and falling of these numbers in the further course of the next decades, the revision burden is projected to remain steady around 15% by the year of 2060, which is why our projections have to be rather seen as a conservative approach. Still, the rising total number and incidence of revision procedures implies higher hospital costs, due to longer length of stay, and longer operative time along with an associated higher perioperative risk of complications and mortality [2, 9]. This inevitably raises the question, if our current health care system will be able to finance the progressive costs and if the provision of high-quality surgical care can be guaranteed in its current form in the future—or if profound changes in indication and access to (surgical) care are necessary to meet the future demand, as projected.
Our study has several limitations, mainly due to the design of our database. In our model, revision hip arthroplasty is handled as an independent orthopedic procedure, although it would seem more appropriate to estimate these projections on the basis of the number of primary arthroplasties performed and an assumed Kaplan–Meier-type survivorship model for the different population subgroups. Although such data can in principle be derived from a national joint registry, it is not yet available in Germany, since the German arthroplasty registry (EPRD) was first established in Germany in 2010. However, the development of such a complex model would only be reasonable, if there would have been evidence that the revision burden had been significantly changing historically over time, which has not been the case in Germany. On the contrary, the revision burden has remained rather unchanged in this country for over a decade, which has also been reported in the United States [2]. Still, our revision projections may be interpreted as a conservative estimation for our future socio-economic health community, if primary implant survival cannot be improved in the upcoming years.
Since the calculations are based on the historical growth of THA and revision THA counts as well as the population projection of the Federal Bureau of Statistics, they might be biased from past trends that may change in the future [4]. Although the official forecast on population developments is included in the projections, we could not take changes of lifestyle (such as becoming more active following primary THA due to steadily improving functional results and subsequently an increased demand for THA) into account. This might directly affect the upcoming need for hip revision surgery mainly by increasing wear [24]. However, at the same time, implant designs and materials may further improve, as already seen in the development of highly cross-linked polythylene [25], potentially being associated with a greater implant survival rate. Additionally, potential limitations in the availability of surgeons or the limited economic resources of private and public payers and hospitals, as well as changes in indication or access to medical care could not be taken into consideration. However, these factors are hard to predict and typically occur gradually, which makes them unlikely to change the trend of our projections during the next couple of years.
Nevertheless, we believe that our regression framework offers an economically acceptable model and its applicability in forecasting total joint replacement is widely accepted. This makes our findings also especially relevant to other countries, like the United States or the UK, where a high incidence and volume of THA already exist.
Conclusion
The demand for revision THA will rise substantially over the next four decades, due to demographic changes, younger recipients of primary THA and an increased life expectancy. This will inevitably result in a constantly increasing socio-economic burden for patients, surgeons, hospitals, insurances and political stakeholders. The projections of the present study provide the necessary foundation for future analyses at a national level, and help to quantify the increasing future challenge of revision hip arthroplasty in Germany and countries with comparable demography.
References
Inacio MCS, Graves SE, Pratt NL, Roughead EE, Nemes S (2017) Increase in total joint arthroplasty projected from 2014 to 2046 in Australia: a conservative local model with international implications. ClinOrthopRelat Res 475(8):2130–2137
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone JtSurg Am 89(4):780–785
Nemes S, Gordon M, Rogmark C, Rolfson O (2014) Projections of total hip replacement in Sweden from 2013 to 2030. Acta Orthop 85(3):238–243
Pilz V, Hanstein T, Skripitz R (2018) Projections of primary hip arthroplasty in Germany until 2040. Acta Orthop 89(3):308–313
Losina E, Thornhill TS, Rome BN, Wright J, Katz JN (2012) The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone JtSurg Am 94(3):201–207
Coleman D, Rowthorn R (2011) Who’s afraid of population decline? A critical examination of its consequences. Popul Dev Rev 37(Suppl 1):217–248
Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J (2005) Hospital resource utilization for primary and revision total hip arthroplasty. J Bone JtSurg Am 87(3):570–576
Bozic KJ, Ries MD (2005) The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone JtSurg Am 87(8):1746–1751
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27(8 Suppl):61-65.e61
Prokopetz JJ, Losina E, Bliss RL, Wright J, Baron JA, Katz JN (2012) Risk factors for revision of primary total hip arthroplasty: a systematic review. BMC MusculoskeletDisord 13:251
Pulido L, Parvizi J, Macgibeny M et al (2008) In hospital complications after total joint arthroplasty. J Arthroplasty 23(6 Suppl 1):139–145
Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS (2012) A financialanalysis of revision hip arthroplasty: the economicburden in relation to the national tariff. J BoneJtSurg (British volume) 94(5):619–623
Lubbeke A, Silman AJ, Barea C, Prieto-Alhambra D, Carr AJ (2018) Mapping existing hip and knee replacement registries in Europe. Health Policy (Amsterdam, Netherlands) 122(5):548–557
Pötzsch ORF (2015) Demographic analyses, methods and projections, births and deaths: Germany’s population by. 2060. Results of the 13th coordinated population projection. Federal Statistical Office, Wiesbaden.
Malchau H, Herberts P, Eisler T, Garellick G, Soderman P (2002) The Swedish total hip replacement register. J BoneJtSurg Am 84-A(Suppl 2):2–20
Petzold T, Haase E, Niethard FU, Schmitt J (2016) Orthopaedic and trauma surgical care until 2050. Analysis of the utilization behavior for relevant diseases and derivation of the number of medical service providers. Orthopade 45(2):167–173
Culliford D, Maskell J, Judge A et al (2015) Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthr Cartilage 23(4):594–600
Erivan R, Villatte G, Dartus J, Reina N, Descamps S, Boisgard S (2019) Progression and projection for hip surgery in France, 2008–2070: epidemiologic study with trend and projection analysis. OrthopTraumatolSurg Res 105(7):1227–1235
Leitner L, Turk S, Heidinger M et al (2018) Trends and economic impact of hip and knee arthroplasty in Central Europe: findings from the Austrian national database. Sci Rep 8(1):4707
Musumeci A, Pranovi G, Masiero S (2018) Patient education and rehabilitation after hip arthroplasty in an Italian spa center: a pilot study on its feasibility. Int J Biometeorol 62(8):1489–1496
Patel A, Pavlou G, Mujica-Mota RE, Toms AD (2015) The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Jt J 97-b(8):1076–1081
Paprosky WG, Sloan M, Sheth NP (2019) Trends in revision total hip arthroplasty, 1993–2014. Orthopaed Proc 101B((Supp_12)):33–33
Sabah SA, Henckel J, Koutsouris S et al (2016) Are all metal-on-metal hip revisionoperationscontributing to the National Joint Registry implant survivalcurves? : a studycomparing the London Implant Retrieval Centre and National Joint Registrydatasets. BoneJt J 98-B(1):33–39
Schmalzried TP (2012) The painful hip: diagnosis and deliverance. J Bone JtSurg (British volume) 94(11 Suppl A):55–57
Devane PA, Horne JG, Ashmore A, Mutimer J, Kim W, Stanley J (2017) Highly cross-linked polyethylene reduces wear and revision rates in total hip arthroplasty: a 10-year double-blinded randomized controlled trial. J Bone JtSurg Am 99(20):1703–1714
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. None of the authors, their immediate families, nor any research foundation with which they are affiliated, received any financial payments or other benefits from any commercial entity related to the subject of this article.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Klug, A., Pfluger, D.H., Gramlich, Y. et al. Future burden of primary and revision hip arthroplasty in Germany: a socio-economic challenge. Arch Orthop Trauma Surg 141, 2001–2010 (2021). https://doi.org/10.1007/s00402-021-03884-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03884-2